Korean J Hematol.
2007 Dec;42(4):397-403. 10.5045/kjh.2007.42.4.397.
Two Cases of Acute Leukemic Transformation with a Chromosome 17 Abnormality and p53 Overexpression Evolving from Essential Thrombocythemia
- Affiliations
-
- 1Department of Laboratory Medicine, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea. hschi@amc.seoul.kr
- 2Department of Internal Medicine, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea.
- KMID: 2252226
- DOI: http://doi.org/10.5045/kjh.2007.42.4.397
Abstract
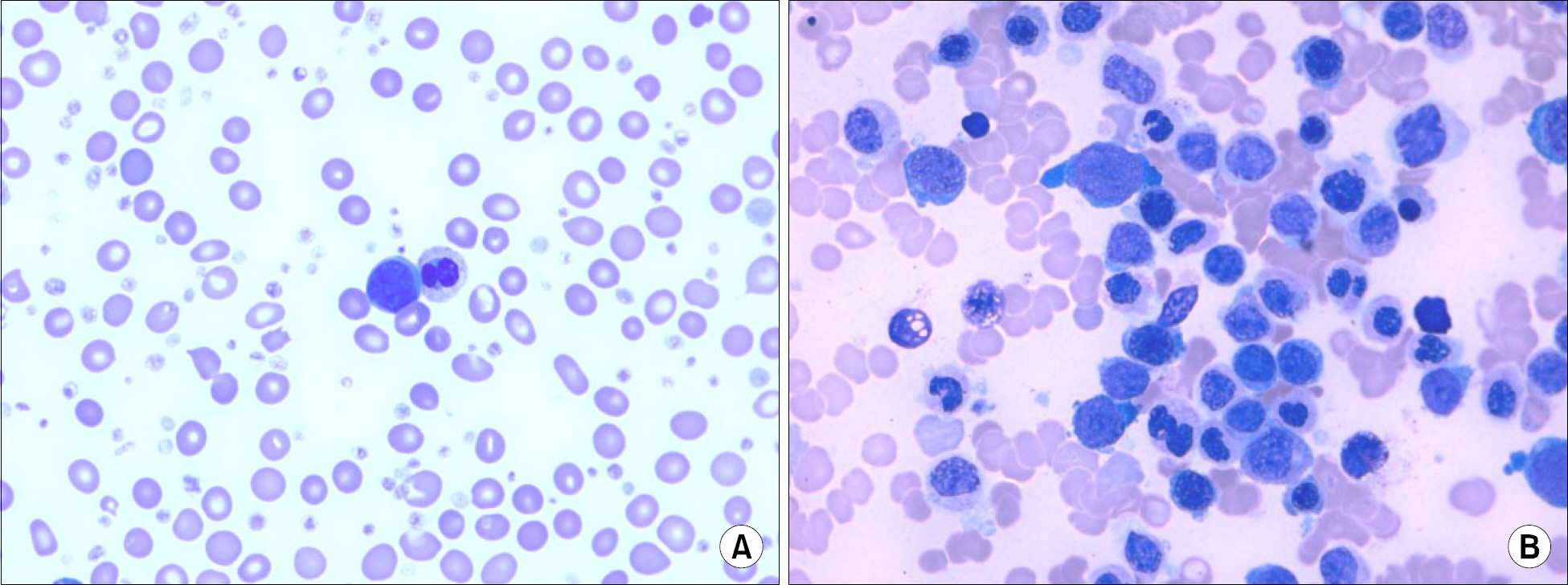
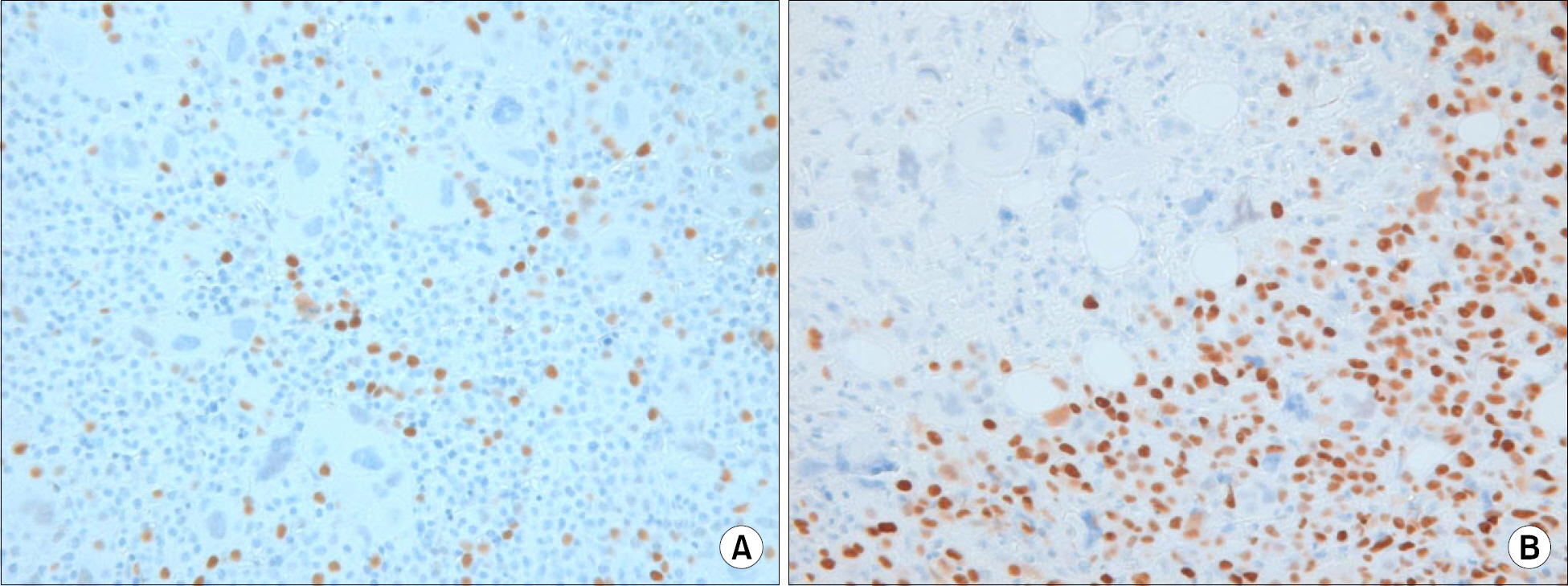
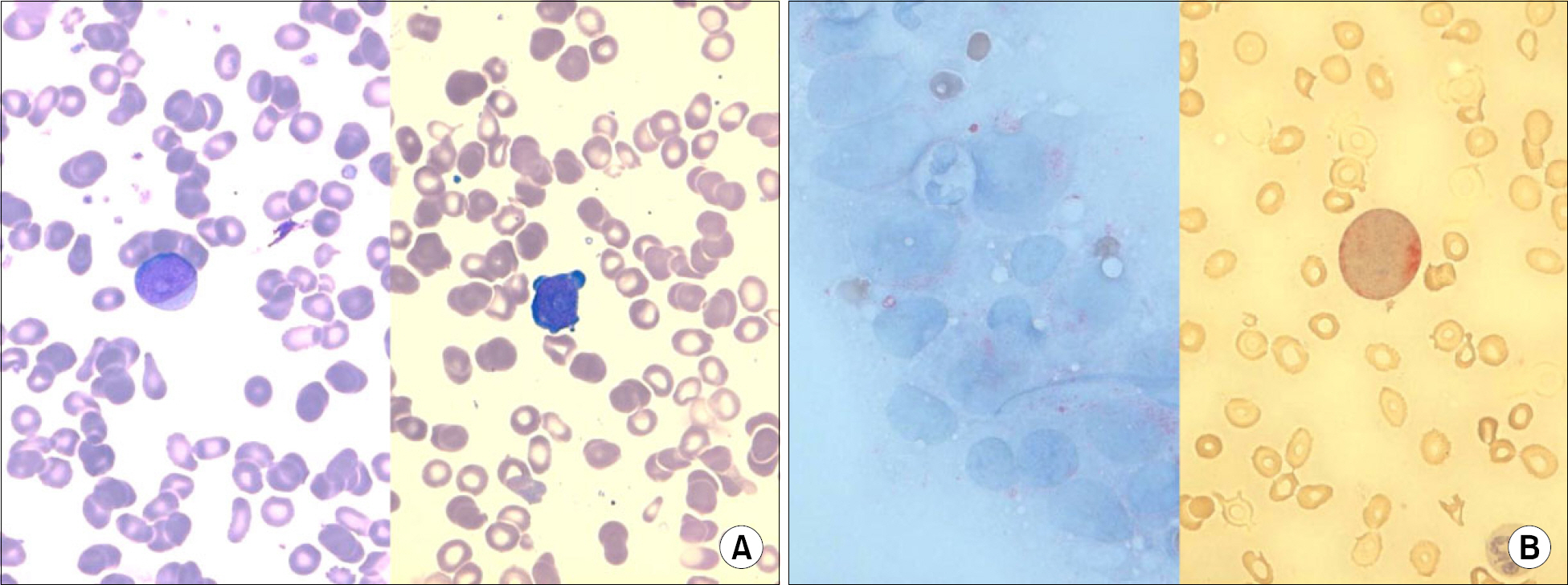
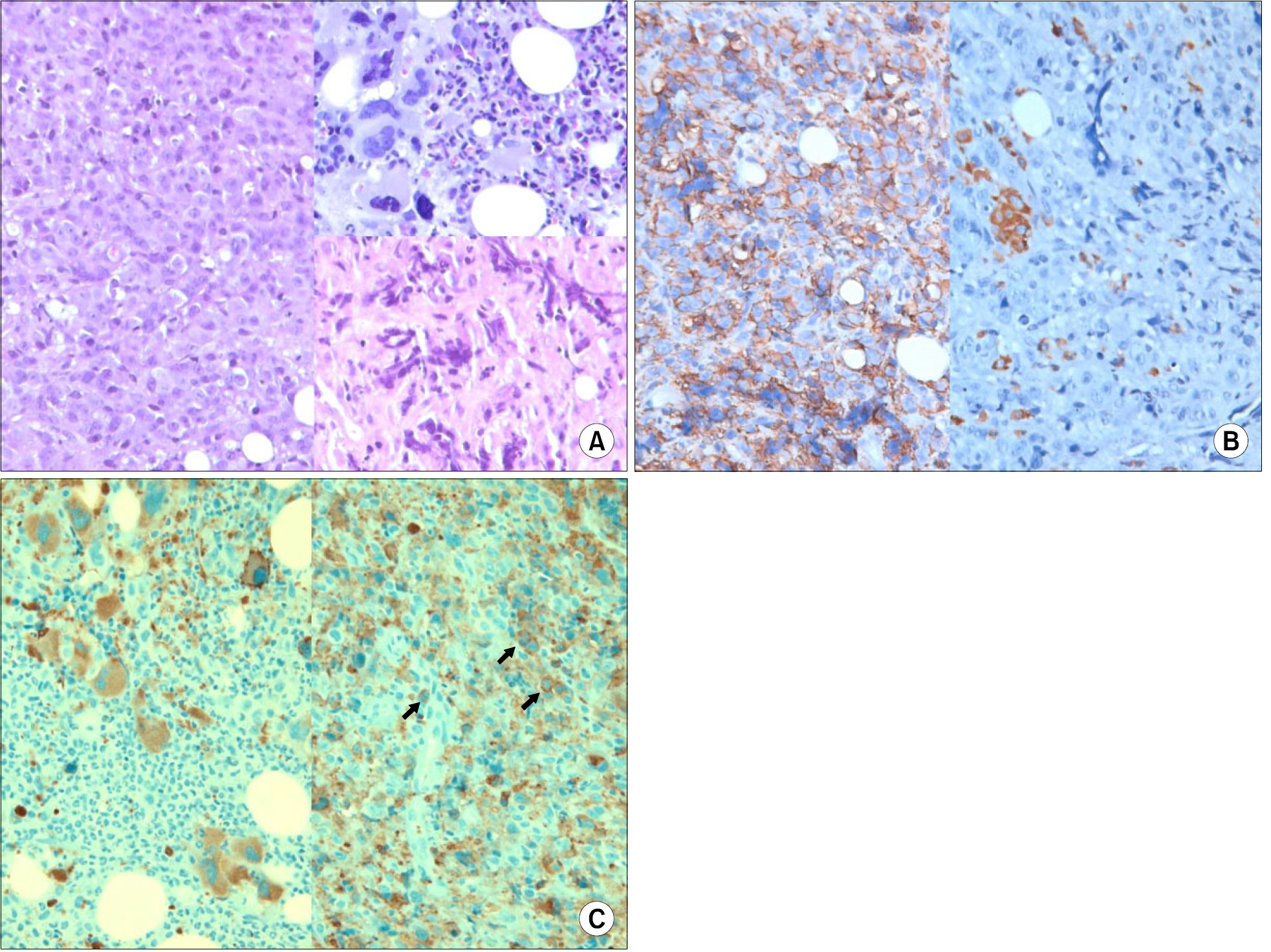
- Essential thrombocythemia (ET) is a clonalmyeloproliferative disorder that can rarely transform into acute leukemia in 1~5% of cases. A recent study has found that a significant proportion of leukemic cases from ET were associated with a cytogenetic abnormality (17p deletion). Herein, we report two cases of acute myeloid leukemic transformations harboring a 17p abnormality from a series of 119 ET patients. The first case, a 48-year-old female, developed acute myeloid leukemia with maturation (AML-M2) accompanying myelodysplasia was diagnosed 6.1 years after the initial diagnosis of ET. She was treated with hydroxyurea. Her karyotype showed a monosomy 17. The second case, a 61-year-old male, developed acute megakaryoblastic leukemia (AML-M7) with a very complex hyperdiploidy including addition of 17p13 that developed 6.5 years after the initial diagnosis. He was treated with hydroxyurea and anagrelide. The immunohistochemistry showed p53 overexpression in both cases. Our cases support the specificity of chromosome 17 abnormality and p53 overexpression in acute leukemic transformation from ET.
MeSH Terms
Figure
Reference
-
1). Imbert M., Vardiman JW., Pierre R., Brunning RD., Thiele J., Flandrin G. Essential thrombocythaemia. Jaffe ES, Harris NL, Stein H, Vardiman JW, editors. Tumours of haematopoietic and lymphoid tissues. 1st ed.Lyon, France: IARC Press;2001. p. 39–41.2). Sterkers Y., Preudhomme C., Lai JL, et al. Acute myeloid leukemia and myelodysplastic syndromes following essential thrombocythemia treated with hydroxyurea: high proportion of cases with 17p deletion. Blood. 1998. 91:616–22.
Article3). Finazzi G., Ruggeri M., Rodeghiero F., Barbui T. Second malignancies in patients with essential thrombocythaemia treated with busulphan and hydroxyurea: long-term follow-up of a randomized clinical trial. Br J Haematol. 2000. 110:577–83.
Article4). Lee JH., Kim TI., Kim GT, et al. A case of leukemic transformation in essential thrombocythemia treated with hydroxyurea. Korean J Hematol. 1997. 32:433–9.5). Fruchtman SM., Petitt RM., Gilbert HS., Fiddler G., Lyne A. Anagrelide Study Group. Anagrelide: analysis of long-term efficacy, safety and leukemogenic potential in myeloproliferative disorders. Leuk Res. 2005. 29:481–91.
Article6). Lai JL., Preudhomme C., Zandecki M, et al. Myelo-dysplastic syndromes and acute myeloid leukemia with 17p deletion. An entity characterized by specific dysgranulopoiesis and a high incidence of p53 mutations. Leukemia. 1995. 9:370–81.7). Merlat A., Lai JL., Sterkers Y, et al. Therapy-related myelodysplastic syndrome and acute myeloid leukemia with 17p deletion. A report on 25 cases. Leukemia. 1999. 13:250–7.
Article8). Bernasconi P., Boni M., Cavigliano PM, et al. Acute myeloid leukemia (AML) having evolved from essential thrombocythemia (ET): distinctive chromosome abnormalities in patients treated with pipobroman or hydroxyurea. Leukemia. 2002. 16:2078–83.
Article9). Radaelli F., Mazza R., Curioni E., Ciani A., Pomati M., Maiolo AT. Acute megakaryocytic leukemia in essential thrombocythemia: an unusual evolution? Eur J Haematol. 2002. 69:108–11.
Article10). Vianelli N., Baravelli S., Gugliotta L. Acute megaka-ryoblastic transformation of essential thrombocythemia. Haematologica. 1996. 81:288–9.11). Geurts van Kessel A., dos Santos NR., Simons A, et al. Molecular cytogenetics of bone and soft tissue tumors. Cancer Genet Cytogenet. 1997. 95:67–73.
Article12). de Bruijn DR., dos Santos NR., Thijssen J, et al. The synovial sarcoma associated protein SYT interacts with the acute leukemia associated AF10. Oncogene. 2001. 20:3281–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Leukemic Transformation in Essential Thrombocythemia Treated with Hydroxyurea
- Apoptosis and Overexpression of p53 in Patients with Myelodysplastic Syndrome and Acute Myelogenous Leukemia
- Two Cases of Philadelphia Chromosome-negative Essential Thrombocythemia Manifested bcr-abl Gene Rearrangement
- A Rare der(Y)t(Y;1)(q12;q12) in a Patient with Essential Thrombocythemia
- A case of chronic myeloid leukemia with features of essential thrombocythemia in peripheral blood and bone marrow