Korean J Hematol.
2009 Dec;44(4):298-303. 10.5045/kjh.2009.44.4.298.
Prolonged Extreme Thrombocytosis in a Postsplenectomy Patient with Hereditary Spherocytosis
- Affiliations
-
- 1Department of Internal Medicine, Gachon University of Medicine and Science, Gil Hospital, Incheon, Korea. jhagnes@gilhospital.com
- KMID: 2252116
- DOI: http://doi.org/10.5045/kjh.2009.44.4.298
Abstract
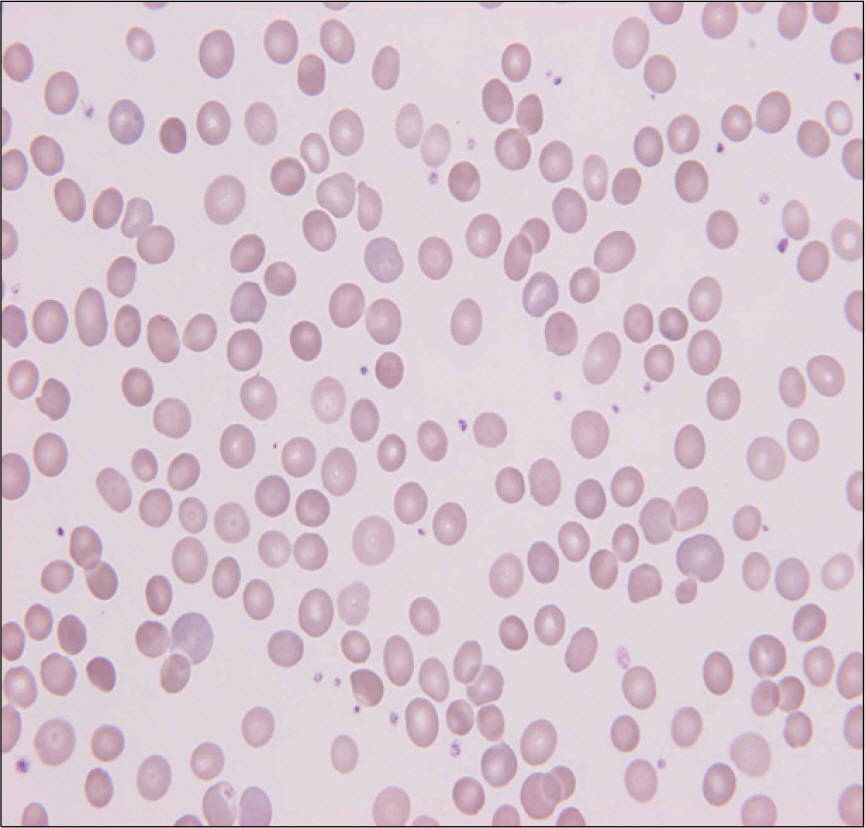
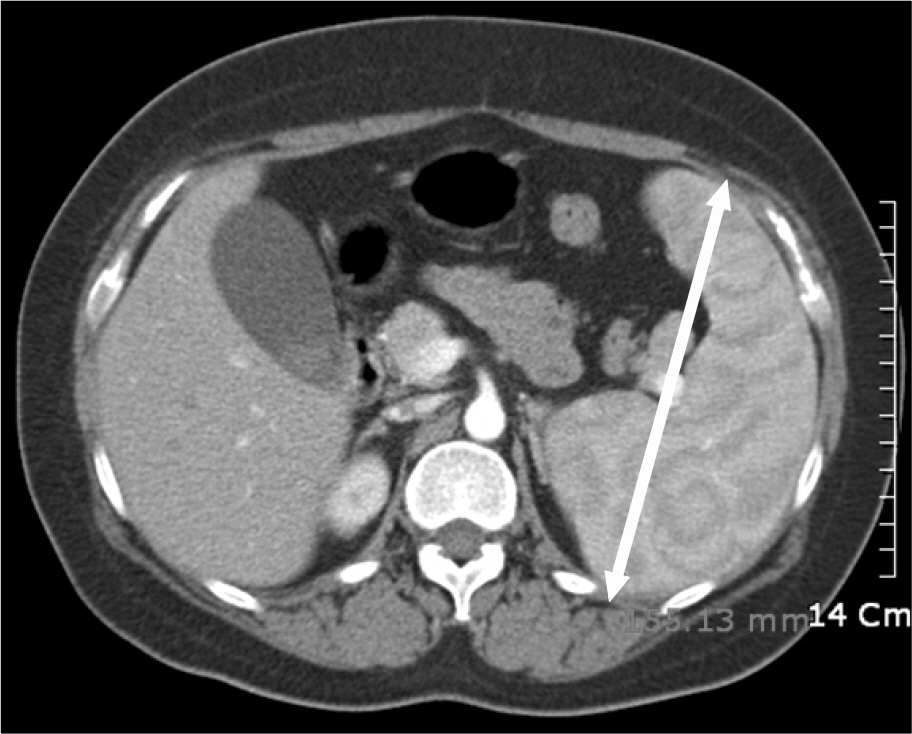
- We report a case of prolonged extreme reactive thrombocytosis in a post-splenectomy patient with hereditary spherocytosis. A 29-year-old female patient presented with gall stones detected incidentally by abdominal ultrasonography. Her laboratory findings showed hemolytic anemia with spherocytosis on the peripheral blood smear and increased osmotic fragility. She was diagnosed with hereditary spherocytosis and underwent a laparoscopic cholecystectomy and splenectomy. After undergoing surgery, the hemolytic anemia was resolved but thrombocytosis was newly detected. Nineteen months after the splenectomy, the thrombocytosis was still persistent and extremely high. To our knowledge, this is the first report of a prolonged extreme reactive thrombocytosis after a splenectomy in Korea.
MeSH Terms
Figure
Reference
-
References
1. Schafer AI. Thrombocytosis. N Engl J Med. 2004; 350:1211–9.
Article2. Greer JP, Foerster J, Rodgers GM, et al. Wintrobe's Clinical Hematology:. Philadelphia: Lippincott Williams & Wilkins;2006. p. 1128–34.3. Buss DH, Cashell AW, O'Connor ML, Richards F 2nd, Case LD. Occurrence, etiology, and clinical significance of extreme thrombocytosis: a study of 280 cases. Am J Med. 1994; 96:247–53.4. Santhosh-Kumar CR, Yohannan MD, Higgy KE, al-Mashhadani SA. Thrombocytosis in adults: analysis of 777 patients. J Intern Med. 1991; 229:493–5.
Article5. Tefferi A, Ho TC, Ahmann GJ, Katzmann JA, Greipp PR. Plasma interleukin-6 and C-reactive protein levels in reactive versus clonal thrombocytosis. Am J Med. 1994; 97:374–8.
Article6. Boxer MA, Braun J, Ellman L. Thromboembolic risk of postsplenectomy thrombocytosis. Arch Surg. 1978; 113:808–9.
Article7. Khan PN, Nair RJ, Olivares J, Tingle LE, Li Z. Postsplenectomy reactive thrombocytosis. Proc (Bayl Univ Med Cent). 2009; 22:9–12.
Article8. Bullen AW, Losowsky MS. Consequences of impaired splenic function. Clin Sci (Lond). 1979; 57:129–37.
Article9. Johnson M, Gernsheimer T, Johansen K. Essential thrombocytosis: underemphasized cause of large-vessel thrombosis. J Vasc Surg. 1995; 22:443–7.
Article10. Daya SK, Gowda RM, Landis WA, Khan IA. Essential thrombocythemia-related acute ST-segment elevation myocardial infarction. A case report and literature review. Angiology. 2004; 55:319–23.11. Wehmeier A, Südhoff T, Meierkord F. Relation of platelet abnormalities to thrombosis and hemorrhage in chronic myeloproliferative disorders. Semin Thromb Hemost. 1997; 23:391–402.
Article12. Hayes DM, Spurr CL, Hutaff LW, Sheets JA. Postsplenectomy thrombocytosis. Ann Intern Med. 1963; 58:259–67.
Article13. Stamou KM, Toutouzas KG, Kekis PB, et al. Prospective study of the incidence and risk factors of postsplenectomy thrombosis of the portal, mesenteric, and splenic veins. Arch Surg. 2006; 141:663–9.
Article14. Buss DH, Stuart JJ, Lipscomb GE. The incidence of thrombotic and hemorrhagic disorders in association with extreme thrombocytosis: an analysis of 129 cases. Am J Hematol. 1985; 20:365–72.
Article15. Kesler A, Ellis MH, Manor Y, Gadoth N, Lishner M. Neurological complications of essential thrombocytosis (ET). Acta Neurol Scand. 2000; 102:299–302.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coexistence of Gilbert Syndrome and Hereditary Spherocytosis in a Child Presenting with Extreme Jaundice
- Splenectomy in Children
- Serial CT Findings of Resolving Extramedullary Hematopoiesis as Unilateral Posterior Mediastinal Mass after Splenectomy in Hereditary Spherocytosis: A Case Report
- A Case of Adrenal Myelolipoma Associated with Hereditary Spherocytosis
- Extramedullary Hematopoiesis at the Posterior Mediastinum in Patient with Hereditary Spherocytosis: A Case Report