Korean J Hepatobiliary Pancreat Surg.
2011 Nov;15(4):225-230. 10.14701/kjhbps.2011.15.4.225.
Efficacy and feasibility of laparoscopic subtotal cholecystectomy for acute cholecystitis
- Affiliations
-
- 1Department of Surgery, Inha University College of Medicine, Incheon, Korea. siahn@inha.ac.kr
- KMID: 2244129
- DOI: http://doi.org/10.14701/kjhbps.2011.15.4.225
Abstract
- BACKGROUNDS/AIMS
For patients with acute cholecystitis, conversion from laparoscopic cholecystectomy to open surgery is not uncommon due to possibilities of serious hemorrhage at the liver bed and bile duct injury. Recent studies reported successful laparoscopic subtotal cholecystectomy for acute cholecystitis. The purpose of this study was to determine the efficacy and feasibility of such an operation based on the experience of surgeons at our facility.
METHODS
In this study, we enrolled 144 patients who had received either laparoscopic subtotal cholecystectomy (LSC), laparoscopic cholecystectomy (LC), or open cholecystectomy (OC) for acute cholecystitis from January 2004 to December 2009 at the Department of Surgery of our hospital. Their symptoms, signs, operative findings, pathologic results and postoperative results were compared and analyzed.
RESULTS
There were 26 patients in the LSC group 80 in the LC group and 38 in the OC group. There were no differences in mean age, sex, and symptoms of acute cholecystitis. The LSC group showed higher CRP levels (p<0.001) and a higher grade according to the Tokyo criteria (p=0.001). The mean operative time was 115.6 minutes and mean blood loss was 158.9 ml without intra-operative or postoperative transfusion. There weren't any bile duct injuries during the operation. No group suffered bile leakage. Drains were removed 3.3 days after the operation in the LC group, the shortest time compared to the other groups (p<0.001). LC and LSC groups demonstrated shorter postoperative hospital days and time to diet resumption than the OC group (p<0.001).
CONCLUSIONS
LSC appears to be a safe and effective treatment in cases of severe acute cholecystitis that require consideration of conversion to open surgery.
MeSH Terms
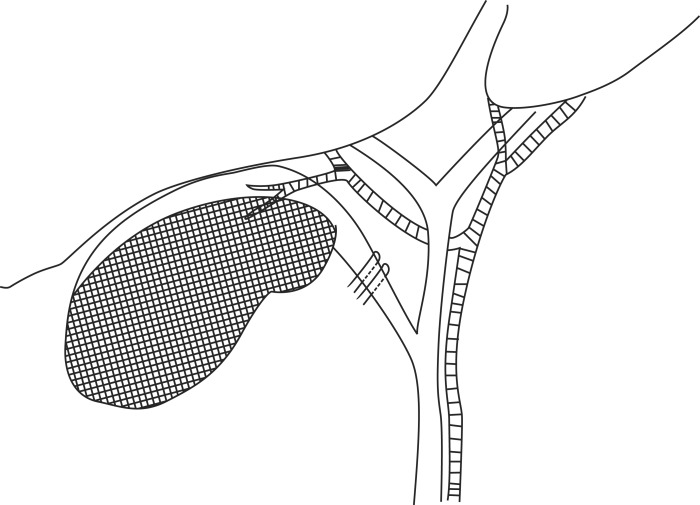
Figure
Reference
-
1. Jacobs M, Verdeja JC, Goldstein HS. Laparoscopic cholecystectomy in acute cholecystitis. J Laparoendosc Surg. 1991; 1:175–177. PMID: 1836405.
Article2. Cox MR, Wilson TG, Luck AJ, Jeans PL, Padbury RT, Toouli J. Laparoscopic cholecystectomy for acute inflammation of the gallbladder. Ann Surg. 1993; 218:630–634. PMID: 8239777.
Article3. Palanivelu C, Rajan PS, Jani K, et al. Laparoscopic cholecystectomy in cirrhotic patients: the role of subtotal cholecystectomy and its variants. J Am Coll Surg. 2006; 203:145–151. PMID: 16864026.
Article4. Chowbey PK, Sharma A, Khullar R, Mann V, Baijal M, Vashistha A. Laparoscopic subtotal cholecystectomy: a review of 56 procedures. J Laparoendosc Adv Surg Tech A. 2000; 10:31–34. PMID: 10706300.
Article5. Michalowski K, Bornman PC, Krige JE, Gallagher PJ, Terblanche J. Laparoscopic subtotal cholecystectomy in patients with complicated acute cholecystitis or fibrosis. Br J Surg. 1998; 85:904–906. PMID: 9692560.
Article6. Ransom KJ. Laparoscopic management of acute cholecystitis with subtotal cholecystectomy. Am Surg. 1998; 64:955–957. PMID: 9764700.7. Sekimoto M, Takada T, Kawarada Y, et al. Need for criteria for the diagnosis and severity assessment of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007; 14:11–14. PMID: 17252292.
Article8. Hirota M, Takada T, Kawarada Y, et al. Diagnostic criteria and severity assessment of acute cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007; 14:78–82. PMID: 17252300.9. Bornman PC, Terblanche J. Subtotal cholecystectomy: for the difficult gallbladder in portal hypertension and cholecystitis. Surgery. 1985; 98:1–6. PMID: 3892743.10. Bickel A, Shtamler B. Laparoscopic subtotal cholecystectomy. J Laparoendosc Surg. 1993; 3:365–367. PMID: 8268507.
Article11. Beldi G, Glättli A. Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg Endosc. 2003; 17:1437–1439. PMID: 12799885.
Article12. Ji W, Li LT, Li JS. Role of laparoscopic subtotal cholecystectomy in the treatment of complicated cholecystitis. Hepatobiliary Pancreat Dis Int. 2006; 5:584–589. PMID: 17085347.13. Philips JA, Lawes DA, Cook AJ, et al. The use of laparoscopic subtotal cholecystectomy for complicated cholelithiasis. Surg Endosc. 2008; 22:1697–1700. PMID: 18071804.
Article14. Sinha I, Smith ML, Safranek P, Dehn T, Booth M. Laparoscopic subtotal cholecystectomy without cystic duct ligation. Br J Surg. 2007; 94:1527–1529. PMID: 17701938.15. Hashizume M, Sugimachi K, MacFadyen BV. The clinical management and results of surgery for acute cholecystitis. Semin Laparosc Surg. 1998; 5:69–80. PMID: 9594034.
Article16. Johansson M, Thune A, Nelvin L, Stiernstam M, Westman B, Lundell L. Randomized clinical trial of open versus laparoscopic cholecystectomy in the treatment of acute cholecystitis. Br J Surg. 2005; 92:44–49. PMID: 15584058.
Article17. Nakajima J, Sasaki A, Obuchi T, Baba S, Nitta H, Wakabayashi G. Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg Today. 2009; 39:870–875. PMID: 19784726.
Article18. Rosenberg J, Bisgaard T. The difficult gallbladder: technical tips for laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2000; 10:249–252. PMID: 10961757.
Article19. Frazee RC, Roberts JW, Okeson GC, et al. Open versus laparoscopic cholecystectomy. A comparison of postoperative pulmonary function. Ann Surg. 1991; 213:651–653. PMID: 1828139.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Cholecystectomy in the Second Trimester of Pregnancy
- The Comparative Analysis of Therapeutic Results between a Laparoscopic Cholecystectomy and an Open cholecystectomy in Acute Cholecystitis
- Laparoscopic cholecystectomy for acute cholecystitis: Any time is a good time
- Application of Laparoscopic Cholecystectomy in Acute Cholecystitis
- What is the Optimal Timing for Laparoscopic Cholecystectomy in Acute Cholecystitis