Korean J Hepatobiliary Pancreat Surg.
2015 May;19(2):71-74. 10.14701/kjhbps.2015.19.2.71.
Long-term outcome of ischemic type biliary stricture after interventional treatment in liver living donors: a report of two cases
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- KMID: 2243052
- DOI: http://doi.org/10.14701/kjhbps.2015.19.2.71
Abstract
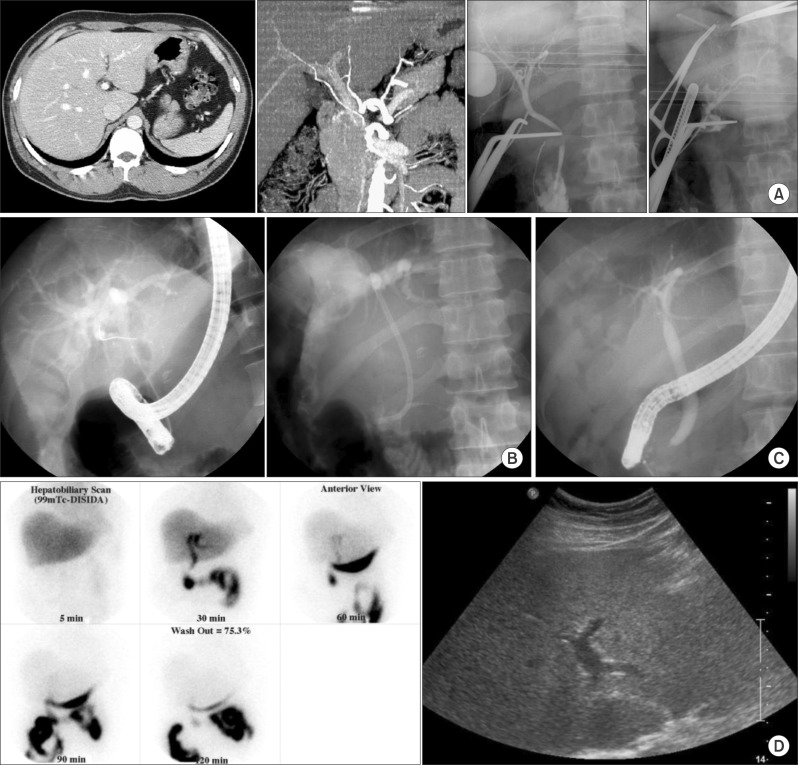
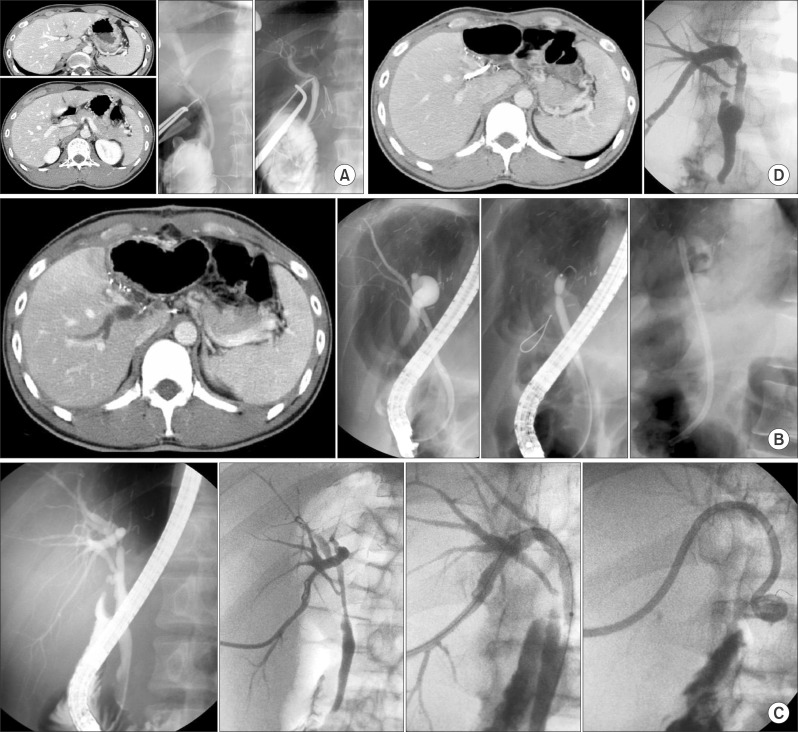
- The wall of normal proximal bile duct is occasionally thin with close approximation to the right hepatic artery. Thus, isolation of this hepatic artery can result in excessive weakening of the remnant proximal bile duct wall during hemiliver graft harvest. This type of injury can induce ischemic stricture of the donor common bile duct. This study aimed to review the clinical sequences of such ischemic type donor bile duct injuries primarily managed with endoscopic and radiological interventional treatments. A retrospective review of medical records was performed for two living donors who suffered from ischemic type donor bile duct injury. They were followed up for more than 10 years. The right and left liver grafts were harvested from these two donors. Bile duct anatomy was normal bifurcation in one and anomalous branching in the other. Bile duct stenosis was detected in them at 2 weeks and 1 week after liver donation. They underwent endoscopic balloon dilatation and temporary stent (endoscopic retrograde biliary drainage tube) insertion. After keeping the tube for 2 months, the tube was successfully removed in one donor. However, endoscopic treatment was not successful, thus additional radiological intervention was necessary in the other donor. On follow-up over 10 years, they are doing well so far with no recurrence of biliary stricture. Based on our limited experience, interventional treatment with subsequent long-term follow-up appears to be an essential and choice treatment for ischemic type biliary stricture occurring in liver living donors.
MeSH Terms
Figure
Reference
-
1. Shin M, Song S, Kim JM, Kwon CH, Kim SJ, Lee SK, et al. Donor morbidity including biliary complications in living-donor liver transplantation: single-center analysis of 827 cases. Transplantation. 2012; 93:942–948. PMID: 22357173.2. Kim SJ, Na GH, Choi HJ, Yoo YK, Kim DG. Surgical outcome of right liver donors in living donor liver transplantation: single-center experience with 500 cases. J Gastrointest Surg. 2012; 16:1160–1170. PMID: 22426687.
Article3. Yi NJ, Suh KS, Cho JY, Lee HW, Cho EH, Yang SH, et al. Three-quarters of right liver donors experienced postoperative complications. Liver Transpl. 2007; 13:797–806. PMID: 17539000.
Article4. Yuan Y, Gotoh M. Biliary complications in living liver donors. Surg Today. 2010; 40:411–417. PMID: 20425542.
Article5. Sultan AM, Salah T, Elshobary MM, Fathy OM, Elghawalby AN, Yassen AM, et al. Biliary complications in living donor right hepatectomy are affected by the method of bile duct division. Liver Transpl. 2014; 20:1393–1401. PMID: 25060964.
Article6. Gruttadauria S, Marsh JW, Vizzini GB, di Francesco F, Luca A, Volpes R, et al. Analysis of surgical and perioperative complications in seventy-five right hepatectomies for living donor liver transplantation. World J Gastroenterol. 2008; 14:3159–3164. PMID: 18506919.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic management of anastomotic stricture after living-donor liver transplantation
- Unilateral Versus Bilateral Biliary Drainage for Post-Transplant Anastomotic Stricture
- Biliary Stricture after Adult Right-Lobe Living-Donor Liver Transplantation with Duct-to-Duct Anastomosis: Long-Term Outcome and Its Related Factors after Endoscopic Treatment
- Long-term Outcome of Endoscopic Retrograde Biliary Drainage of Biliary Stricture Following Living Donor Liver Transplantation
- Outcome of donor biliary complications following living donor liver transplantation