Clin Orthop Surg.
2015 Sep;7(3):337-343. 10.4055/cios.2015.7.3.337.
Particular Features of Surgical Site Infection in Posterior Lumbar Interbody Fusion
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul Sacred Heart General Hospital, Seoul, Korea. adkajs@hanmail.net
- KMID: 2234088
- DOI: http://doi.org/10.4055/cios.2015.7.3.337
Abstract
- BACKGROUND
Previous reports have observed differences only in infection rates between posterolateral fusion and posterior lumbar interbody fusion (PLIF). There have been no reports that describe the particular features of surgical site infection (SSI) in PLIF. In this study, we endeavor to identify the distinguishing characteristics and risk factors of SSI in PLIF.
METHODS
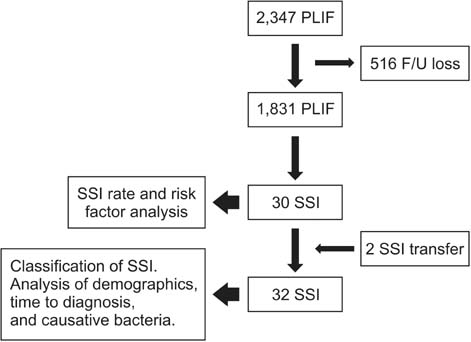
Our study undertook a review of a case series of an institute. Patients who had undergone PLIF consecutively in the author's hospital were reviewed. Two proactive procedures were introduced during the study period. One was irrigation of the autolocal bone, and the other was the intradiscal space irrigation with a nozzle. Infection rate and risk factors were analyzed. For subgroup analysis, the elapsed time to a diagnosis (ETD), clinical manifestations, hematologic findings, and causative bacteria were examined in patients with SSI.
RESULTS
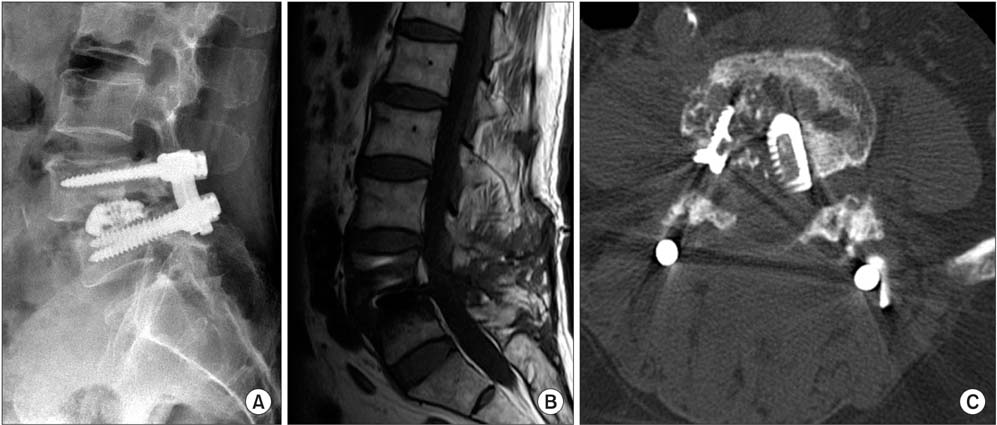
In a total of 1,831 cases, there were 30 cases of SSI (1.6%). Long operation time was an independent risk factor (p = 0.008), and local bone irrigation was an independent protective factor (p = 0.001). Two cases of referred SSI were included in the subgroup analysis. There were 6/32 (19%) superficial incisional infections (SII), 6/32 (19%) deep incisional infections (DII), and 20/32 (62%) organ/space infections (O/SI). The difference of incidence among three groups was significant (p = 0.002).The most common bacteria encountered were methicillin-resistant Staphylococcus epidermidis followed by methicillin-resistant S. aureus in incisional infections, and no growth followed by S. epidermidis in O/SI. ETD was 8.5 +/- 2.3 days in SII, 8.7 +/- 2.3 days in DII and 164.5 +/- 131.1 days in O/SI (p = 0.013).
CONCLUSIONS
The rate of SSI in PLIF was 1.6%, with the most common type being O/SI. The causative bacteria of O/SI was of lower virulence than in the incisional infection, and thus diagnosis was delayed due to its latent and insidious feature. Contamination of auto-local bone was presumed attributable to the progression of SSI. Irrigation of auto-local bone helped in the reduction of SSI.
Keyword
MeSH Terms
Figure
Reference
-
1. Ha KY, Na KH, Shin JH, Kim KW. Comparison of posterolateral fusion with and without additional posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Spinal Disord Tech. 2008; 21(4):229–234.
Article2. Musluman AM, Yilmaz A, Cansever T, et al. Posterior lumbar interbody fusion versus posterolateral fusion with instrumentation in the treatment of low-grade isthmic spondylolisthesis: midterm clinical outcomes. J Neurosurg Spine. 2011; 14(4):488–496.
Article3. Farrokhi MR, Rahmanian A, Masoudi MS. Posterolateral versus posterior interbody fusion in isthmic spondylolisthesis. J Neurotrauma. 2012; 29(8):1567–1573.
Article4. Liu X, Wang Y, Qiu G, Weng X, Yu B. A systematic review with meta-analysis of posterior interbody fusion versus posterolateral fusion in lumbar spondylolisthesis. Eur Spine J. 2014; 23(1):43–56.
Article5. Ye YP, Xu H, Chen D. Comparison between posterior lumbar interbody fusion and posterolateral fusion with transpedicular screw fixation for isthmic spondylolithesis: a meta-analysis. Arch Orthop Trauma Surg. 2013; 133(12):1649–1655.
Article6. Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Posterior lumbar interbody fusion: a retrospective study of complications after facet joint excision and pedicle screw fixation in 148 cases. Acta Orthop Scand. 1999; 70(4):329–334.
Article7. Pappou IP, Papadopoulos EC, Sama AA, Girardi FP, Cammisa FP. Postoperative infections in interbody fusion for degenerative spinal disease. Clin Orthop Relat Res. 2006; 444:120–128.
Article8. Ahn DK, Park HS, Choi DJ, et al. The difference of surgical site infection according to the methods of lumbar fusion surgery. J Spinal Disord Tech. 2012; 25(8):E230–E234.
Article9. Yashiro K, Homma T, Hokari Y, Katsumi Y, Okumura H, Hirano A. The Steffee variable screw placement system using different methods of bone grafting. Spine (Phila Pa 1976). 1991; 16(11):1329–1334.
Article10. Mirovsky Y, Floman Y, Smorgick Y, et al. Management of deep wound infection after posterior lumbar interbody fusion with cages. J Spinal Disord Tech. 2007; 20(2):127–131.
Article11. Ahn DK, Choi DJ, Park HS, Kim TW, Chun TH, Yang JH. Precautions against infection following posterior spinal fusion based on types of infection and risk factors. J Korean Soc Spine Surg. 2009; 16(4):274–284.
Article12. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999; 27(2):97–132.13. Richards BS. Delayed infections following posterior spinal instrumentation for the treatment of idiopathic scoliosis. J Bone Joint Surg Am. 1995; 77(4):524–529.
Article14. Clark CE, Shufflebarger HL. Late-developing infection in instrumented idiopathic scoliosis. Spine (Phila Pa 1976). 1999; 24(18):1909–1912.
Article15. Richards BR, Emara KM. Delayed infections after posterior TSRH spinal instrumentation for idiopathic scoliosis: revisited. Spine (Phila Pa 1976). 2001; 26(18):1990–1996.16. Albert HB, Sorensen JS, Christensen BS, Manniche C. Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. Eur Spine J. 2013; 22(4):697–707.
Article17. Albert HB, Lambert P, Rollason J, et al. Does nuclear tissue infected with bacteria following disc herniations lead to Modic changes in the adjacent vertebrae? Eur Spine J. 2013; 22(4):690–696.
Article18. Carricajo A, Nuti C, Aubert E, et al. Propionibacterium acnes contamination in lumbar disc surgery. J Hosp Infect. 2007; 66(3):275–277.
Article19. Stirling A, Worthington T, Rafiq M, Lambert PA, Elliott TS. Association between sciatica and Propionibacterium acnes. Lancet. 2001; 357(9273):2024–2025.
Article20. Dietz FR, Koontz FP, Found EM, Marsh JL. The importance of positive bacterial cultures of specimens obtained during clean orthopaedic operations. J Bone Joint Surg Am. 1991; 73(8):1200–1207.
Article21. Ahn DK, Park HS, Kim TW, et al. The degree of bacterial contamination while performing spine surgery. Asian Spine J. 2013; 7(1):8–13.
Article22. Carmouche JJ, Molinari RW. Epidural abscess and discitis complicating instrumented posterior lumbar interbody fusion: a case report. Spine (Phila Pa 1976). 2004; 29(23):E542–E546.
Article23. Tokuhashi Y, Ajiro Y, Umezawa N. Conservative follow-up after epidural abscess and diskitis complicating instrumented metal interbody cage. Orthopedics. 2008; 31(6):611.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- Posterior Lumbar Interbody Fusion
- A Comparison of Posterolateral and Posterior Interbody Fusion in the Surgical Treatment of Lumbar Spondylolisthesis
- Clinical Comparison between Decompression and Posterior Lumbar Interbody Fusion in Chronic Lower Back Pain Involving Degenerative Disc Disease and Spinal Stenosis
- Evaluation of Posterior Lumbar Interbody Fusion