Clin Orthop Surg.
2015 Sep;7(3):291-297. 10.4055/cios.2015.7.3.291.
Comparison of the Sliding and Femoral Head Rotation among Three Different Femoral Head Fixation Devices for Trochanteric Fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, Kobe University Graduate School of Medicine, Kobe, Japan.
- 2Department of Orthopedic Surgery, Takatsuki General Hospital, Takatsuki, Japan. takafumi.hiranaka@gmail.com
- 3Department of Orthopaedic Surgery, Iwate Medical University School of Medicine, Morioka, Japan.
- KMID: 2234081
- DOI: http://doi.org/10.4055/cios.2015.7.3.291
Abstract
- BACKGROUND
Recently, various femoral head fixation devices (HFDs) for trochanteric fractures have become available. However, there are some cases in which femoral head rotation with excessive sliding of the HFD is observed and it is often followed by cutout. The purpose of this study is to compare the ability of the three types of HFDs to prevent femoral head rotation.
METHODS
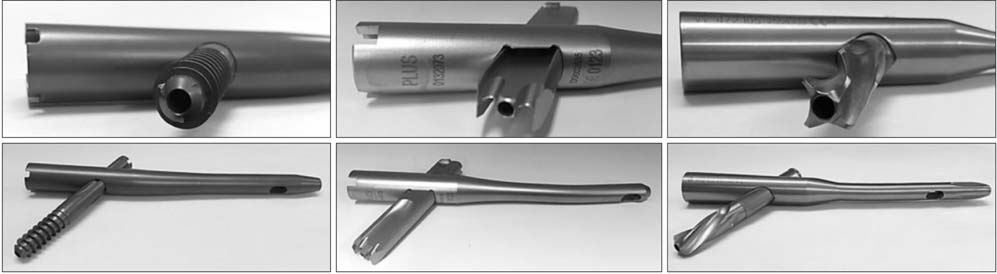
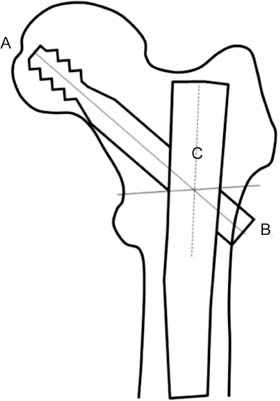
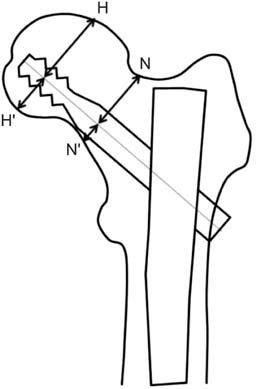
Between July 2005 and December 2009, 206 patients aged over 60 years with trochanteric fractures who had undergone surgical treatment using a short femoral nail in our institution were enrolled into the study. We used the gamma 3 nail (GMN) as the screw-type HFD in 66 cases, the gliding nail (GLN) as a non-cylindrical blade in 76 cases, and the proximal femoral nail antirotation (PFNA) as a cylindrical blade in 64 cases. The sliding length of HFDs and the occurrence of femoral head rotation were evaluated by assessing radiographs as the main outcome, and the results were compared among these devices.
RESULTS
A comparison of the degree of sliding in the GMN group showed that femoral head rotation was observed significantly more frequently in cases with rotation. Further, it appeared that femoral head rotation occurred more frequently in comminuted fractures. However, no significant differences between the sliding lengths of the different HFDs were observed among three groups. Femoral head rotation was observed in 15 cases of GMN (22.7%), 0 case of GLN, and 5 case of PFNA (7.8%). Significant differences with regard to the occurrence of femoral head rotation were observed among the three groups. Furthermore, significant differences were also observed between GLN and PFNA with respect to the occurrence of femoral head rotation.
CONCLUSIONS
The ability to stabilize femoral head appears to be greater with blade-type materials than with screw-type materials. Furthermore, we believe that a non-cylindrical blade is preferable to a cylindrical blade for the surgical treatment of comminuted, unstable trochanteric fractures in order to prevent femoral head rotation and cut-out.
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Outcomes of U-blade Gamma3 Nails Used to Treat Patients with Trochanteric Fractures: Retrospective Multicenter Study
Jehyun Yoo, Sangmin Kim, Hojung Jung, Jihyo Hwang
Hip Pelvis. 2019;31(2):95-101. doi: 10.5371/hp.2019.31.2.95.
Reference
-
1. Kannus P, Parkkari J, Sievanen H, Heinonen A, Vuori I, Jarvinen M. Epidemiology of hip fractures. Bone. 1996; 18:1 Suppl. 57S–63S.2. Xu YZ, Geng DC, Mao HQ, Zhu XS, Yang HL. A comparison of the proximal femoral nail antirotation device and dynamic hip screw in the treatment of unstable pertrochanteric fracture. J Int Med Res. 2010; 38(4):1266–1275.3. Fritz T, Weiss C, Krieglstein C, Quentmeier A. The classic nail in the therapy of trochanteric fractures: a prospective, controlled study. Arch Orthop Trauma Surg. 1999; 119(5-6):308–314.4. Curtis MJ, Jinnah RH, Wilson V, Cunningham BW. Proximal femoral fractures: a biomechanical study to compare intramedullary and extramedullary fixation. Injury. 1994; 25(2):99–104.5. Radford PJ, Needoff M, Webb JK. A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J Bone Joint Surg Br. 1993; 75(5):789–793.6. Saudan M, Lubbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer P. Pertrochanteric fractures: is there an advantage to an intramedullary nail?: a randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma. 2002; 16(6):386–393.7. Gehr J, Arnold T, Hilsenbeck F, Friedl W. The gliding nail, a universal implant in the treatment of proximal femur fractures. Eur J Trauma. 2006; 32(6):562–569.8. Baumgaertner MR, Solberg BD. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br. 1997; 79(6):969–971.9. Halder SC. The Gamma nail for peritrochanteric fractures. J Bone Joint Surg Br. 1992; 74(3):340–344.10. Zhou F, Zhang ZS, Yang H, et al. Less invasive stabilization system (LISS) versus proximal femoral nail anti-rotation (PFNA) in treating proximal femoral fractures: a prospective randomized study. J Orthop Trauma. 2012; 26(3):155–162.11. Cheung JP, Chan CF. Cutout of proximal femoral nail antirotation resulting from blocking of the gliding mechanism during fracture collapse. J Orthop Trauma. 2011; 25(6):e51–e55.12. Friedl W, Clausen J. Experimental examination for optimized stabilisation of trochanteric femur fractures, intra- or extramedullary implant localisation and influence of femur neck component profile on cut-out risk. Chirurg. 2001; 72(11):1344–1352.13. Lucke M, Burghardt RD, Siebenlist S, Ganslmeier A, Stockle U. Medial migration of lag screw with intrapelvic dislocation in gamma nailing: a unique problem? A report of 2 cases. J Orthop Trauma. 2010; 24(2):e6–e11.14. Hiranaka T, Chinzei N, Hida Y, Tsuji M. Accurate measurement of the sliding length of femoral head fixation devices of intramedullary nail for trochanteric fractures. Kossetsu. 2011; 33(3):652–654.15. Tsukada S, Okumura G, Matsueda M. Postoperative stability on lateral radiographs in the surgical treatment of pertrochanteric hip fractures. Arch Orthop Trauma Surg. 2012; 132(6):839–846.16. Pascarella R, Cucca G, Maresca A, et al. Methods to avoid gamma nail complications. Chir Organi Mov. 2008; 91(3):133–139.17. De Bruijn K, den Hartog D, Tuinebreijer W, Roukema G. Reliability of predictors for screw cutout in intertrochanteric hip fractures. J Bone Joint Surg Am. 2012; 94(14):1266–1272.18. Brown RH, Burstein AH, Frankel VH. Telemetering in vivo loads from nail plate implants. J Biomech. 1982; 15(11):815–823.19. Bergmann G, Graichen F, Rohlmann A. Hip joint loading during walking and running, measured in two patients. J Biomech. 1993; 26(8):969–990.20. Sommers MB, Roth C, Hall H, et al. A laboratory model to evaluate cutout resistance of implants for pertrochanteric fracture fixation. J Orthop Trauma. 2004; 18(6):361–368.21. Ehmke LW, Fitzpatrick DC, Krieg JC, Madey SM, Bottlang M. Lag screws for hip fracture fixation: evaluation of migration resistance under simulated walking. J Orthop Res. 2005; 23(6):1329–1335.22. Bojan AJ, Beimel C, Taglang G, Collin D, Ekholm C, Jonsson A. Critical factors in cut-out complication after Gamma Nail treatment of proximal femoral fractures. BMC Musculoskelet Disord. 2013; 14:1.
Article23. Brunner A, Jockel JA, Babst R. The PFNA proximal femur nail in treatment of unstable proximal femur fractures: 3 cases of postoperative perforation of the helical blade into the hip joint. J Orthop Trauma. 2008; 22(10):731–736.
Article24. Tyllianakis M, Panagopoulos A, Papadopoulos A, Papasimos S, Mousafiris K. Treatment of extracapsular hip fractures with the proximal femoral nail (PFN): long term results in 45 patients. Acta Orthop Belg. 2004; 70(5):444–454.25. Al-yassari G, Langstaff RJ, Jones JW, Al-Lami M. The AO/ASIF proximal femoral nail (PFN) for the treatment of unstable trochanteric femoral fracture. Injury. 2002; 33(5):395–399.
Article26. Wild M, Jungbluth P, Thelen S, et al. The dynamics of proximal femoral nails: a clinical comparison between PFNA and Targon PF. Orthopedics. 2010; 33(8):DOI: 10.3928/01477447-20100625-04.
Article27. Strauss E, Frank J, Lee J, Kummer FJ, Tejwani N. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: a biomechanical evaluation. Injury. 2006; 37(10):984–989.
Article28. Windolf M, Braunstein V, Dutoit C, Schwieger K. Is a helical shaped implant a superior alternative to the Dynamic Hip Screw for unstable femoral neck fractures? A biomechanical investigation. Clin Biomech (Bristol, Avon). 2009; 24(1):59–64.
Article29. Xu Y, Geng D, Yang H, Wang X, Zhu G. Treatment of unstable proximal femoral fractures: comparison of the proximal femoral nail antirotation and gamma nail 3. Orthopedics. 2010; 33(7):473.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fixation Failure of Proximal Femoral Nail Anti-rotation in Femoral Intertrochanteric Fracture
- Treatment of Trochanteric Fractures of the Femur with Compression Hip Screw-Analysis of Factors associated with Failure of Fixation-
- Excessive Sliding of the Helical Blade and the Femoral Neck Fracture after Insertion of Proximal Femoral Nail Anti-Rotation for Type A2 Intertrochanteric Fractures - A Case Report -
- Femoral Neck Fracture After Removal of the Intramedullary Nail for the Fixation of an Intertrochanteric Fracture: Report of 2 Cases
- Fixation Failure after internal Fixation in Intertrochanteric Fractures