Korean Circ J.
2008 Nov;38(11):590-595. 10.4070/kcj.2008.38.11.590.
Similar Degree in Mechanical Left Ventricular Dyssynchrony Between Right Ventricular Outflow Tract and Right Ventricular Apical Pacing: A Strain Doppler Imaging Study
- Affiliations
-
- 1Department of Cardiology, Catholic University of Daegu, Korea.
- 2Keimyung University Dongsan Medical Center, Daegu, Korea. swhan@dsmc.or.kr
- 3University of Washington School of Medicine, Seattle, Washington, USA.
- KMID: 2225706
- DOI: http://doi.org/10.4070/kcj.2008.38.11.590
Abstract
- BACKGROUND AND OBJECTIVES
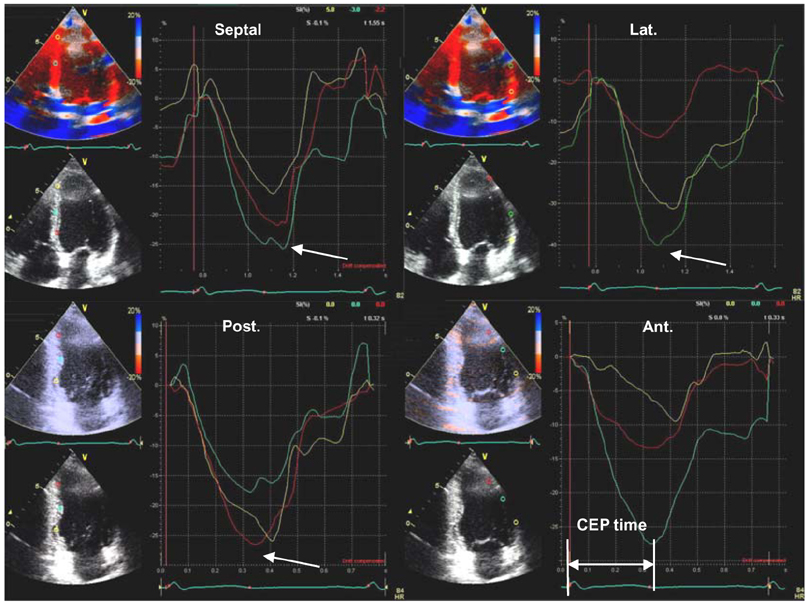
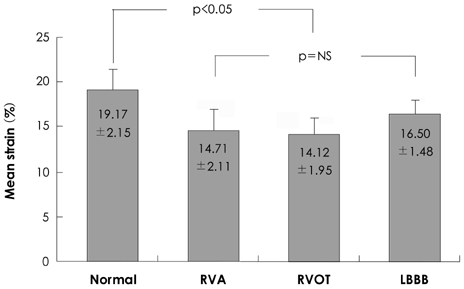
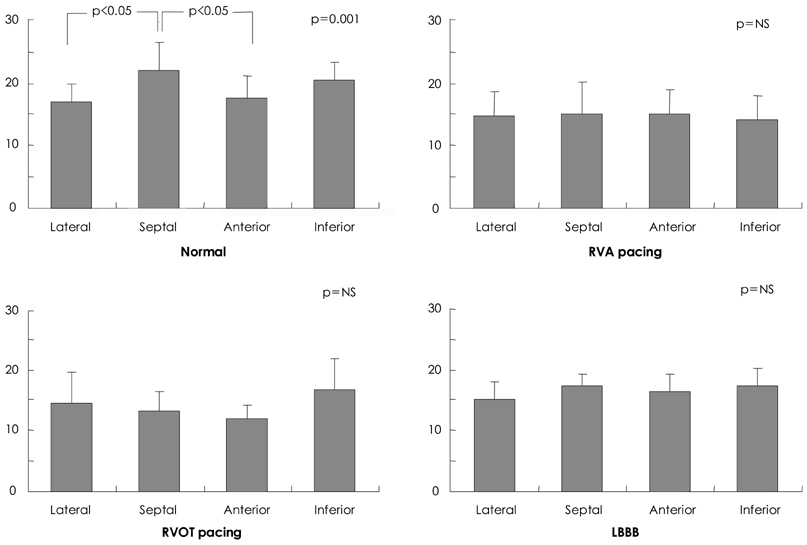
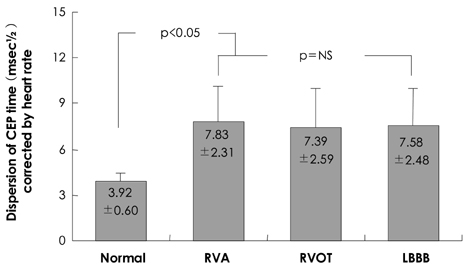
Long-term right ventricular (RV) apex pacing has been associated with left ventricular (LV) systolic dysfunction. However, pacing in the RV outflow tract (RVOT) is associated with a narrower QRS duration and may have a more normal LV activation in comparison to RV apical (RVA) pacing. We hypothesized that RVOT pacing is associated with less mechanical dyssynchrony compared to RVA pacing and that it also more closely resembles mechanical activation in normal controls with a narrow QRS. SUBJECTS AND METHODS: We studied 9 patients with RV pacing, 9 with left bundle branch block (LBBB), and 15 normal controls with a narrow QRS. In the RV pacing group, we paced from the RVA and RVOT. At the end of each pacing train, we obtained echocardiographic images in the apical 4- and 2-chamber views and obtained the following parameters: the compression/expansion crossover point (CEP) for myocardial strain and the time from QRS onset to the CEP in the strain image. The degree of dyssynchrony was evaluated using the dispersion and standard deviation of CEP times in 12 segments of the LV. RESULTS: Significant dyssynchrony was observed in the RVOT pacing group compared to the group with normal QRS. No significant difference was observed in LV mechanical dyssynchrony among the RVOT pacing, RVA pacing, and LBBB groups. CONCLUSION: RVOT pacing is associated with significant LV dyssynchrony. Although the RVOT has been recommended as an alternative site for pacing, this approach may have adverse effects on long-term LV function.
Keyword
Figure
Reference
-
1. Wilkoff BL. The Dual Chamber, and VVI Implantable Defibrillator (DAVID) Trial: rationale, design, results, clinical implications and lessons for future trials. Card Electrophysiol Rev. 2003. 7:468–472.2. Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2006. 346:877–883.3. Lee MY, Rho TH, Yoo KD, et al. The relationship between QRS duration and LV systolic function in paced patients. Korean Circ J. 2001. 31:327–334.4. Tse HF, Lau CP. Long-term effect of right ventricular pacing on myocardial perfusion and function. J Am Coll Cardiol. 1997. 29:744–749.5. Cha KS, Min JJ, Kim JH, et al. Alterations in myocardial perfusion and regional wall motion in patients with permanent pacemaker. Korean Circ J. 1998. 28:506–515.6. McGavigan AD, Mond HG. Selective site ventricular pacing. Curr Opin Cardiol. 2006. 21:7–14.7. Sweeney MO, Prinzen FW. A new paradigm for physiologic ventricular pacing. J Am Coll Cardiol. 2006. 47:282–288.8. Gold MR, Shorofsky SR, Metcalf MD, Feliciano Z, Fisher ML, Gottlieb SS. The acute hemodynamic effects of right ventricular septal pacing in patients with congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 1997. 79:679–681.9. Kim HY, Kim JH, Rho TH, et al. Hemodynamic responses to different ventricular pacing sites and pacing rates in dog. Korean Circ J. 1998. 28:1605–1615.10. De Cock CC, Meyer A, Kamp O, Visser CA. Hemodynamic benefits of right ventricular outflow tract pacing: comparison with right ventricular apex pacing. Pacing Clin Electrophysiol. 1998. 21:536–541.11. Mabo P, Scherlag BJ, Munsif A, Otomo K, Lazzara R. A technique for stable His-bundle recording and pacing: electrophysiological and hemodynamic correlates. Pacing Clin Electrophysiol. 1995. 18:1894–1901.12. Gorcsan J 3rd, Kanzaki H, Bazaz R, Dohi K, Schwartzman D. Usefulness of echocardiographic tissue synchronization imaging to predict acute response to cardiac resynchronization therapy. Am J Cardiol. 2004. 93:1178–1181.13. Dohi K, Suffoletto MS, Schwartzman D, Ganz L, Pinsky MR, Gorcsan J 3rd. Utility of echocardiographic radial strain imaging to quantify left ventricular dyssynchrony and predict acute response to cardiac resynchronization therapy. Am J Cardiol. 2005. 96:112–116.14. Bazett HC. An analysis of the time-relation of electrocardiograms. Heart. 1920. 7:353–370.15. De Cock CC, Giudici MC, Twisk JW. Comparison of the haemodynamic effects of right ventricular outflow-tract pacing with right ventricular apex pacing: a quantitative review. Europace. 2003. 5:275–278.16. Giudici MC, Thomburg GA, Buck DL, et al. Comparision of right ventricular outflow tract and apical lead permanent pacing on cardiac output. Am J Cardiol. 1997. 79:209–212.17. Tse HF, Yu C, Wong KK, et al. Functional abnormalities in patients with permanent right ventricular pacing: the effect of sites of electrical stimulation. J Am Coll Cardiol. 2002. 40:1451–1458.18. Buckingham TA, Candinas R, Attenhofer C, et al. Systolic and diastolic function with alternate and combined site pacing in the right ventricle. Pacing Clin Electrophysiol. 1998. 21:1077–1084.19. Victor F, Leclercq C, Mabo P, et al. Optimal right ventricular pacing site in chronically implanted patients: a prospective randomized crossover comparison of apical and outflow tract pacing. J Am Coll Cardiol. 1999. 33:311–316.20. Stambler BS, Ellenbogen K, Zhang X, et al. Right ventricular outflow versus apical pacing in pacemaker patients with congestive heart failure and atrial fibrillation. J Cardiovasc Electrophysiol. 2003. 14:1180–1186.21. Rosenqvist M, Bergfeldt L, Haga Y, Rydén J, Rydén L, Owall A. The effect of ventricular activation sequence on cardiac performance during pacing. Pacing Clin Electrophysiol. 1996. 19:1279–1286.22. Riedlbauchova L, Kautzner J, Hatala R, Buchingham TS. Is right ventricular outflow tract pacing an alternative to left ventricular/ biventricular pacing? Pacing Clin Electrophysiol. 2004. 27:871–877.23. Thambo JB, Bordachar P, Garrigue S, et al. Detrimental ventricular remodeling in patients with congenital complete heart block and chronic right ventricular apical pacing. Circulation. 2004. 110:3766–3772.24. Bax JJ, Ansalone G, Breithardt OA, et al. Echocardiographic evaluation of cardiac resynchronization therapy: ready for routine clinical use?: a critical appraisal. J Am Coll Cardiol. 2004. 44:1–9.25. Bax JJ, Marwick TH, Molhoek SG, et al. Left ventricular dyssynchrony predicts benefit of cardiac resynchronization therapy in patients with end stage heart failure before pacemaker implantation. Am J Cardiol. 2003. 92:1238–1240.26. Yu CM, Fung JW, Zhang Q, et al. Tissue Doppler imaging is superior to strain rate imaging and postsystolic shortening on the prediction of reverse remodeling in both ischemic and nonischemic heart failure after cardiac resynchronization therapy. Circulation. 2004. 110:66–73.27. Dohi K, Suffoleto MS, Schwarzman D, Ganz L, Pinsky MR, Gorcsan J 3rd. Utility of echocardiographic radial strain imaging to quantify left ventricular dyssynchrony and predict acute response to cardiac resynchronization therapy. Am J Cardiol. 2005. 96:112–116.28. Abraham TP, Nishimura RA, Holmes DR Jr, Belohlavek M, Seward JB. Strain rate imaging for assessment of regional myocardial function: results from a clinical model of septal ablation. Circulation. 2002. 105:1403–1406.29. Blanc JJ, Etienne Y, Gilard M, et al. Evaluation of different ventricular pacing sites in patients with severe heart failure: results of an acute hemodynamic study. Circulation. 1997. 96:3273–3277.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ventricular dyssynchrony in patients with permanent pacemaker
- Impact of Right Ventricular Apical Pacing and Its Frequency on Left Atrial Function
- Huge Multilobulated Left Ventricular Outflow Tract Pseudoaneurysm Presenting with Ventricular Tachycardia
- A Case of Left Ventricular Outflow Obstruction Caused by Mitral Valve Replacement
- Relationship between Systolic Anterior Motion of the Mitral Valve and the Left Ventricular Outflow Pressure Gradient in Patients with Hypertrophic Obstructive Cardiomyopathy