J Cardiovasc Ultrasound.
2015 Dec;23(4):276-279. 10.4250/jcu.2015.23.4.276.
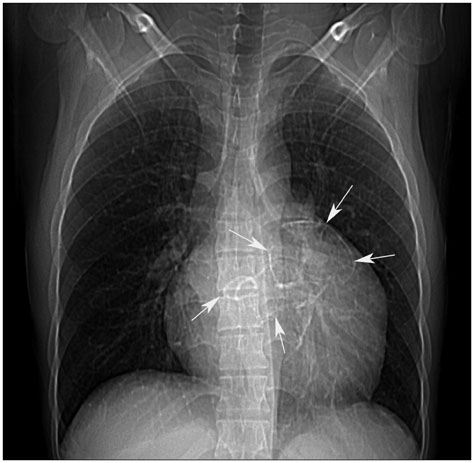
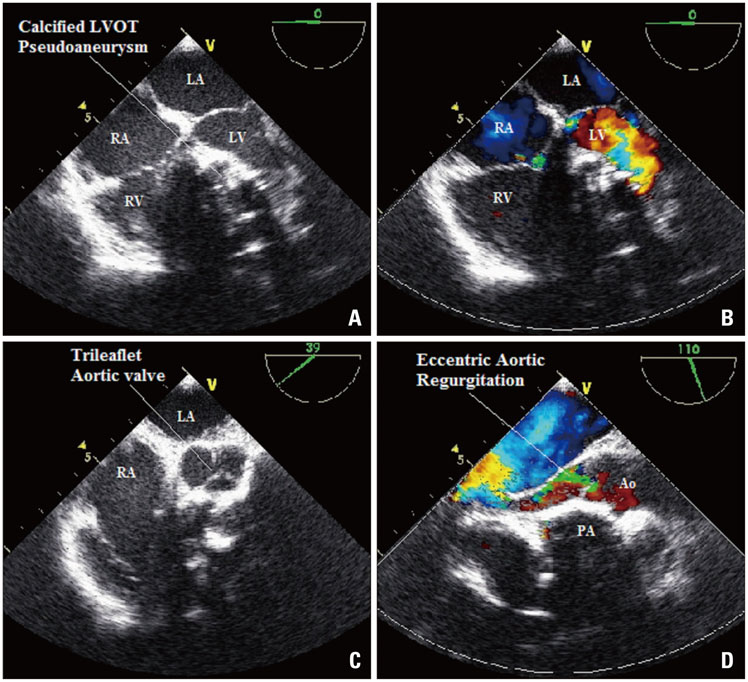
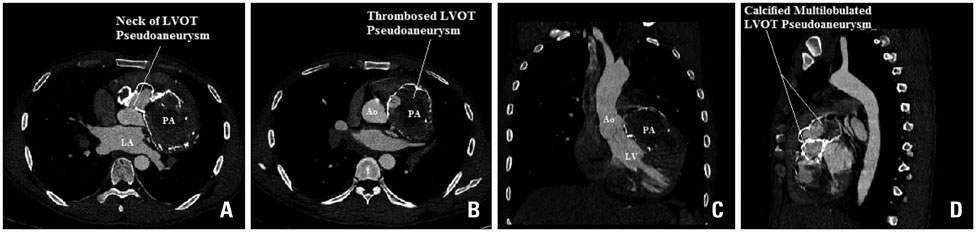
Huge Multilobulated Left Ventricular Outflow Tract Pseudoaneurysm Presenting with Ventricular Tachycardia
- Affiliations
-
- 1Department of Cardiology, U N Mehta Institute of Cardiology and Research Centre, Ahmedabad, Gujarat, India. dr.rajivkharwar@gmail.com
- KMID: 2144462
- DOI: http://doi.org/10.4250/jcu.2015.23.4.276
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
1. Afridi I, Apostolidou MA, Saad RM, Zoghbi WA. Pseudoaneurysms of the mitral-aortic intervalvular fibrosa: dynamic characterization using transesophageal echocardiographic and Doppler techniques. J Am Coll Cardiol. 1995; 25:137–145.2. Jha AK, Pandey R, Gharde P, Devagourou V, Kiran U. Idiopathic left ventricular outflow tract pseudoaneurysm. Ann Card Anaesth. 2013; 16:209–211.3. Kaul S, Josephson MA, Tei C, Wittig JH, Millman J, Shah PM. Atypical echocardiographic and angiographic presentation of a postoperative pseudoaneurysm of the left ventricle after repair of a true aneurysm. J Am Coll Cardiol. 1983; 2:780–784.4. Yeo TC, Malouf JF, Reeder GS, Oh JK. Clinical characteristics and outcome in postinfarction pseudoaneurysm. Am J Cardiol. 1999; 84:592–595.5. Da Col U, Ramoni E, Di Bella I, Ragni T. An unusual left ventricular outflow pseudoaneurysm: usefulness of echocardiography and multidetector computed tomography for surgical repair. Cardiovasc Intervent Radiol. 2009; 32:188–191.6. Savage MP, Hopkins JT, Templeton JY 3rd, Goldburgh WP, Goldberg S. Left ventricular pseudopseudoaneurysm: angiographic features and surgical treatment of impending cardiac rupture. Am Heart J. 1988; 116:864–866.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Polymorphic Ventricular Tachycardia: a “Benign Disease†with a Touch of Bad Luck?
- Giant Cardiac Rhabdomyoma with Mixed Atrial Tachycardia and Nonsustained Ventricular Tachycardia in a Newborn with Tuberous Sclerosis
- Multiple Rhabomyomas in left Ventricular Outflow Tract Combined with Tuberous Sclerosis: A Case Report
- Ventricular Tachycardia in Neonates: A Report of Two Cases and Review of the Literature
- A Rare Case of Unruptured Sinus of Valsalva Aneurysm Obstructing the Right Ventricular Outflow Tract