Korean Circ J.
2013 Sep;43(9):600-606. 10.4070/kcj.2013.43.9.600.
Effect of Abciximab on the Levels of Circulating Microparticles in Patients with Acute Myocardial Infarction Treated by Primary Angioplasty
- Affiliations
-
- 1Cardiology Division, Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. cardioblues@yuhs.ac
- 2Severance Institute for Vascular and Metabolic Research, Yonsei University College of Medicine, Seoul, Korea.
- 3Cardiovascular Product Evaluation Center, Yonsei University Health System, Seoul, Korea.
- KMID: 2224815
- DOI: http://doi.org/10.4070/kcj.2013.43.9.600
Abstract
- BACKGROUND AND OBJECTIVES
We investigated the effect of the additional use of abciximab during percutaneous coronary intervention (PCI) on the level of procoagulant microparticles (MPs) in patients with ST-segment elevation myocardial infarction (STEMI) who had undergone primary PCI.
SUBJECTS AND METHODS
In this study, we studied 86 patients with STEMI (72 men, age 58+/-13) who had undergone primary PCI. The decision to administer abciximab immediately prior to PCI was left to the discretion of the operator. Blood samples for analysis of MPs were obtained from the femoral artery before and after PCI. MPs with procoagulant potential were measured using a commercial kit. The cellular origins of MPs were determined by antigenic capture with specific antibodies.
RESULTS
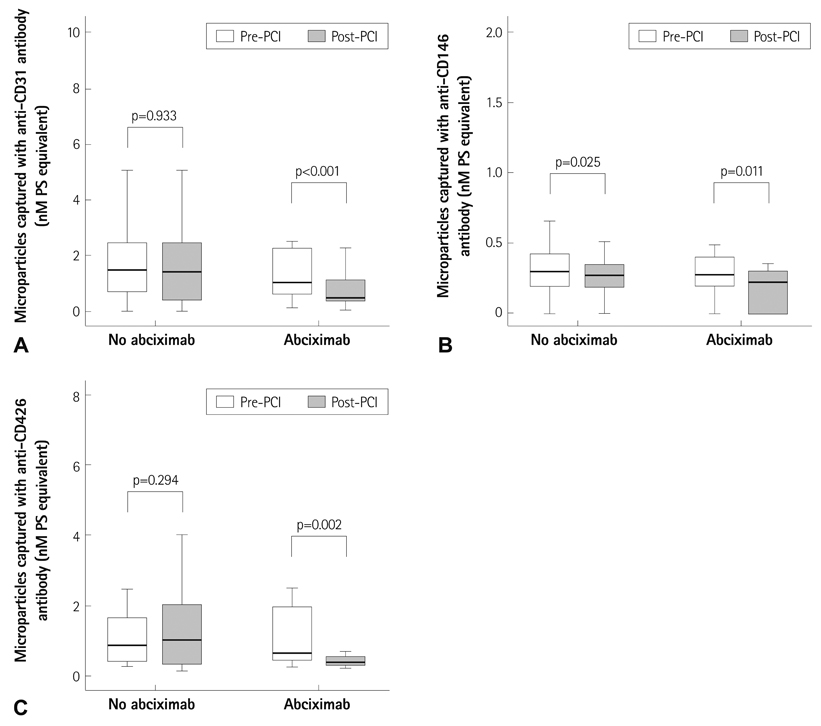
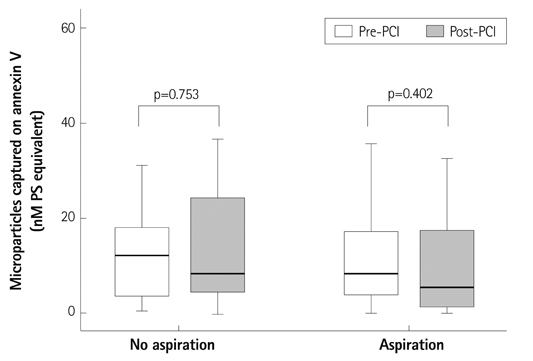
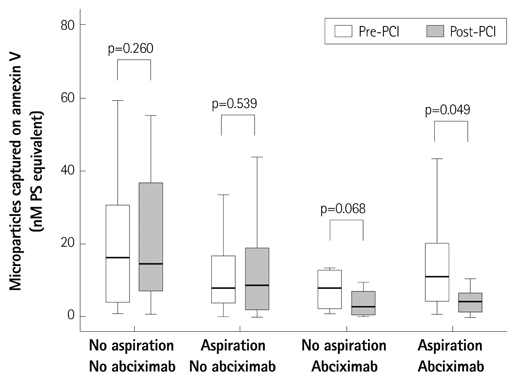
Procoagulant MPs captured onto annexin V were not changed significantly after PCI {13.4+/-13.2 nM vs. 13.2+/-16.1 nM phosphatidylserine equivalent (PS eq), p=0.479}. Abciximab was used in 30 of 86 patients (35%) immediately prior to PCI. In patients who had undergone PCI without abciximab, no significant change in the level of MPs was observed after PCI. However, in the abciximab group, the level of circulating MPs was significantly decreased after PCI (12.0+/-10.7 nM vs. 7.8+/-11.7 nM PS eq, p=0.018). Levels of endothelial- and platelet-derived MPs also showed a significant reduction after PCI in the abciximab group.
CONCLUSION
Primary PCI with additional abciximab significantly reduced the level of procoagulant MPs regardless of their cellular origins in patients with STEMI.
MeSH Terms
Figure
Reference
-
1. VanWijk MJ, VanBavel E, Sturk A, Nieuwland R. Microparticles in cardiovascular diseases. Cardiovasc Res. 2003; 59:277–287.2. Puddu P, Puddu GM, Cravero E, Muscari S, Muscari A. The involvement of circulating microparticles in inflammation, coagulation and cardiovascular diseases. Can J Cardiol. 2010; 26:140–145.3. Leroyer AS, Isobe H, Lesèche G, et al. Cellular origins and thrombogenic activity of microparticles isolated from human atherosclerotic plaques. J Am Coll Cardiol. 2007; 49:772–777.4. Mallat Z, Benamer H, Hugel B, et al. Elevated levels of shed membrane microparticles with procoagulant potential in the peripheral circulating blood of patients with acute coronary syndromes. Circulation. 2000; 101:841–843.5. Bernal-Mizrachi L, Jy W, Jimenez JJ, et al. High levels of circulating endothelial microparticles in patients with acute coronary syndromes. Am Heart J. 2003; 145:962–970.6. Morel O, Pereira B, Averous G, et al. Increased levels of procoagulant tissue factor-bearing microparticles within the occluded coronary artery of patients with ST-segment elevation myocardial infarction: role of endothelial damage and leukocyte activation. Atherosclerosis. 2009; 204:636–641.7. Min PK, Kim JY, Chung KH, et al. Local increase in microparticles from the aspirate of culprit coronary arteries in patients with ST-segment elevation myocardial infarction. Atherosclerosis. 2013; 227:323–328.8. Morel O, Hugel B, Jesel L, et al. Circulating procoagulant microparticles and soluble GPV in myocardial infarction treated by primary percutaneous transluminal coronary angioplasty. A possible role for GPIIb-IIIa antagonists. J Thromb Haemost. 2004; 2:1118–1126.9. Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000; 36:959–969.10. Jy W, Horstman LL, Jimenez JJ, et al. Measuring circulating cell-derived microparticles. J Thromb Haemost. 2004; 2:1842–1851.11. Jeske WP, Walenga JM, Szatkowski E, et al. Effect of glycoprotein IIb/IIIa antagonists on the HIT serum induced activation of platelets. Thromb Res. 1997; 88:271–281.12. Simon DI, Xu H, Ortlepp S, Rogers C, Rao NK. 7E3 monoclonal antibody directed against the platelet glycoprotein IIb/IIIa cross-reacts with the leukocyte integrin Mac-1 and blocks adhesion to fibrinogen and ICAM-1. Arterioscler Thromb Vasc Biol. 1997; 17:528–535.13. Gawaz M, Neumann FJ, Dickfeld T, et al. Vitronectin receptor (alpha(v) beta3) mediates platelet adhesion to the luminal aspect of endothelial cells: implications for reperfusion in acute myocardial infarction. Circulation. 1997; 96:1809–1818.14. Yeh CH, Peng HC, Huang TF. Accutin, a new disintegrin, inhibits angiogenesis in vitro and in vivo by acting as integrin alphavbeta3 antagonist and inducing apoptosis. Blood. 1998; 92:3268–3276.15. Aymong ED, Curtis MJ, Youssef M, et al. Abciximab attenuates coronary microvascular endothelial dysfunction after coronary stenting. Circulation. 2002; 105:2981–2985.16. Bernal-Mizrachi L, Jy W, Fierro C, et al. Endothelial microparticles correlate with high-risk angiographic lesions in acute coronary syndromes. Int J Cardiol. 2004; 97:439–446.17. Simak J, Gelderman MP, Yu H, Wright V, Baird AE. Circulating endothelial microparticles in acute ischemic stroke: a link to severity, lesion volume and outcome. J Thromb Haemost. 2006; 4:1296–1302.18. Koga H, Sugiyama S, Kugiyama K, et al. Elevated levels of VE-cadherinpositive endothelial microparticles in patients with type 2 diabetes mellitus and coronary artery disease. J Am Coll Cardiol. 2005; 45:1622–1630.19. Nozaki T, Sugiyama S, Sugamura K, et al. Prognostic value of endothelial microparticles in patients with heart failure. Eur J Heart Fail. 2010; 12:1223–1228.20. Amabile N, Heiss C, Chang V, et al. Increased CD62e(+) endothelial microparticle levels predict poor outcome in pulmonary hypertension patients. J Heart Lung Transplant. 2009; 28:1081–1086.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of change of coronary artery flow using corrected TIMI frame count following abciximab adminstration during primary angioplasty for acute myocardial infarction
- A case of acute profound thrombocytopenia following abciximab therapy
- The Effects of Abciximab on Left Ventricular Remodeling in Patient with Acute Myocardial Infarction Treated with Primary Percutaneous Coronary Intervention
- A Case of Acute Myocardial Infarction Associated with Myocardial Bridge Treated by Primary Coronary Stenting
- Rescue Utilization of Abciximab (ReoPro) for the Thrombus