Korean Circ J.
2014 Mar;44(2):118-121. 10.4070/kcj.2014.44.2.118.
Transvenous Pacemaker Lead Removal in Pacemaker Lead Endocarditis with Large Vegetations: A Report of Two Cases
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. cby6908@yuhs.ac
- KMID: 2223901
- DOI: http://doi.org/10.4070/kcj.2014.44.2.118
Abstract
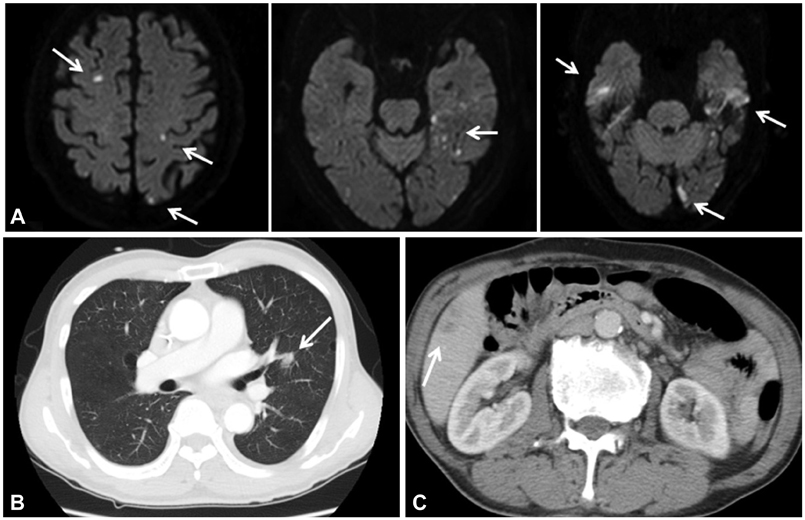
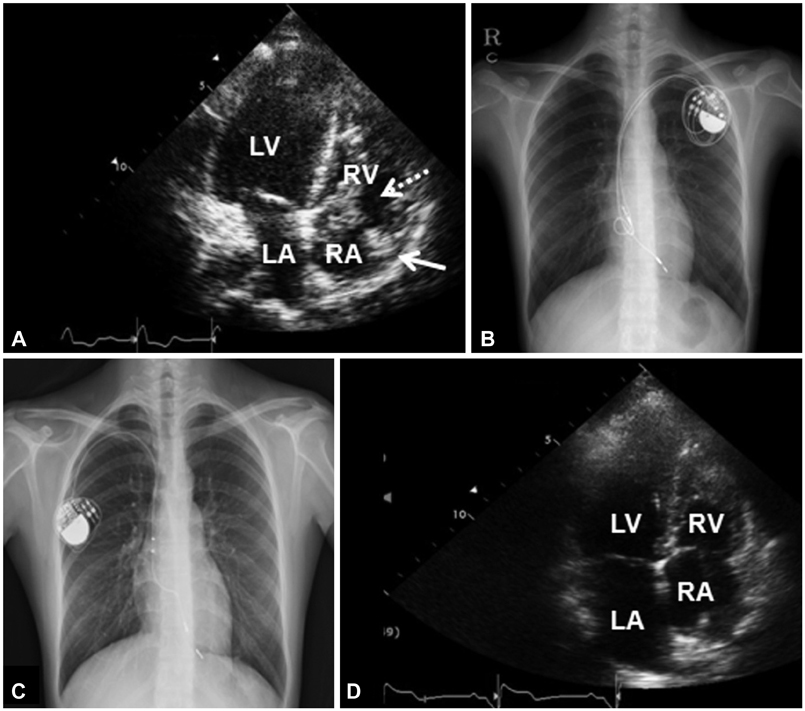
- Pacemaker lead endocarditis is treated with total removal of the infected device and proper antibiotics. The outcomes of patients undergoing percutaneous lead extraction for large vegetations (>2 cm) have not yet been shown. In this case report, we present two patients with pacemaker lead endocarditis with large vegetations of maximum diameter 2.4 cm and 3.2 cm. The first patient had multiple vegetations attached to the tricuspid and mitral valves and developed septic emboli to the brain, lung, and liver. The second patient had a large, persistent vegetation on the tricuspid valve, even two weeks after complete removal of the leads. Both patients were successfully treated with transvenous pacemaker lead removal and antibiotics.
MeSH Terms
Figure
Reference
-
1. Chua JD, Wilkoff BL, Lee I, Juratli N, Longworth DL, Gordon SM. Diagnosis and management of infections involving implantable electrophysiologic cardiac devices. Ann Intern Med. 2000; 133:604–608.2. Mond HG, Proclemer A. The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: calendar year 2009--a World Society of Arrhythmia's project. Pacing Clin Electrophysiol. 2011; 34:1013–1027.3. Klug D, Balde M, Pavin D, et al. Risk factors related to infections of implanted pacemakers and cardioverter-defibrillators: results of a large prospective study. Circulation. 2007; 116:1349–1355.4. Ruttmann E, Hangler HB, Kilo J, et al. Transvenous pacemaker lead removal is safe and effective even in large vegetations: an analysis of 53 cases of pacemaker lead endocarditis. Pacing Clin Electrophysiol. 2006; 29:231–236.5. Sohail MR, Uslan DZ, Khan AH, et al. Management and outcome of permanent pacemaker and implantable cardioverter-defibrillator infections. J Am Coll Cardiol. 2007; 49:1851–1859.6. Camus C, Leport C, Raffi F, et al. Sustained bacteremia in 26 patients with a permanent endocardial pacemaker: assessment of wire removal. Clin Infect Dis. 1993; 17:46–55.7. Meier-Ewert HK, Gray ME, John RM. Endocardial pacemaker or defibrillator leads with infected vegetations: a single-center experience and consequences of transvenous extraction. Am Heart J. 2003; 146:339–344.8. Klug D, Lacroix D, Savoye C, et al. Systemic infection related to endocarditis on pacemaker leads: clinical presentation and management. Circulation. 1997; 95:2098–2107.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endocarditis with Intracardiac Migration of Transvenous Permanent Pacing Lead: 1 Case Report
- Pacemaker Lead Endocarditis Combined with Rupture of Sinus Valsalva after Redo Aortic Valve Replacement
- Infected Endocarditis Related Pacemaker leads: A Case Report
- A Case of Pacemaker Implantation after Balloon Venoplasty on Innominate Vein Stenosis
- Removal of Entrapped Pacemaker Electrode: One Case Report