Korean Circ J.
2014 Sep;44(5):312-319. 10.4070/kcj.2014.44.5.312.
Late Gadolinium Enhancement in Cardiac MRI in Patients with Severe Aortic Stenosis and Preserved Left Ventricular Systolic Function Is Related to Attenuated Improvement of Left Ventricular Geometry and Filling Pressure after Aortic Valve Replacement
- Affiliations
-
- 1Division of Cardiology and Radiology, Severance Cardiovascular Hospital, Yonsei University Health System, Seoul, Korea. hjchang@yuhs.ac
- 2Severance Biomedical Science Institute, Yonsei University College of Medicine, Yonsei University Health System, Seoul, Korea.
- KMID: 2223870
- DOI: http://doi.org/10.4070/kcj.2014.44.5.312
Abstract
- BACKGROUND AND OBJECTIVES
We investigated echocardiographic predictors: left ventricular (LV) geometric changes following aortic valve replacement (AVR) according to the late gadolinium enhancement (LGE) on cardiac magnetic resonance imaging (CMR) in patients with severe aortic stenosis (AS) and preserved LV systolic function.
SUBJECTS AND METHODS
We analyzed 41 patients (24 males, 63.1+/-8.7 years) with preserved LV systolic function who were scheduled to undergo AVR for severe AS. All patients were examined with transthoracic echocardiography (TTE), CMR before and after AVR (in the hospital) and serial TTEs (at 6 and 12 months) were repeated.
RESULTS
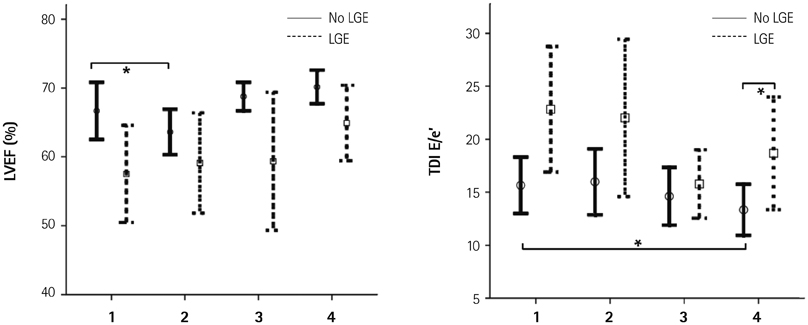
The group with LGE (LGE+) showed greater wall thickness (septum, 14.3+/-2.6 mm vs. 11.5+/-2.0 mm, p=0.001, posterior; 14.3+/-2.5 mm vs. 11.4+/-1.6 mm, p<0.001), lower tissue Doppler image (TDIS', 4.4+/-1.4 cm/s vs. 5.5+/-1.2 cm/s, p=0.021; TDI E', 3.2+/-0.9 cm/s vs. 4.8+/-1.4 cm/s, p=0.002), and greater E/e' (21.8+/-10.3 vs. 15.4+/-6.3, p=0.066) than those without LGE (LGE-). Multivariate analysis show that TDI e' (odds ratio=0.078, 95% confidence interval=0.007-0.888, p=0.040) was an independent determinant of LGE+. In an analysis of the 6- and 12-month follow-up compared with pre-AVR, LGE- showed decreased LV end-diastolic diameter (48.3+/-5.0 mm vs. 45.8+/-3.6 mm, p=0.027; 48.3+/-5.0 mm vs. 46.5+/-3.4 mm, p=0.019). Moreover, E/e' (at 12 months) showed further improved LV filling pressure (16.0+/-6.6 vs. 12.3+/-4.3, p=0.001) compared with pre-AVR. However, LGE+ showed no significant improvement.
CONCLUSION
The absence of LGE is associated with favorable improvements in LV geometry and filling pressure. TDI E' is an independent determinant of LGE in patients with severe AS and preserved LV systolic function.
Keyword
MeSH Terms
Figure
Reference
-
1. Czer LS, Gray RJ, Stewart ME, De Robertis M, Chaux A, Matloff JM. Reduction in sudden late death by concomitant revascularization with aortic valve replacement. J Thorac Cardiovasc Surg. 1988; 95:390–401.2. Morris JJ, Schaff HV, Mullany CJ, et al. Determinants of survival and recovery of left ventricular function after aortic valve replacement. Ann Thorac Surg. 1993; 56:22–29. discussion 29-30.3. Smith N, McAnulty JH, Rahimtoola SH. Severe aortic stenosis with impaired left ventricular function and clinical heart failure: results of valve replacement. Circulation. 1978; 58:255–264.4. Connolly HM, Oh JK, Orszulak TA, et al. Aortic valve replacement for aortic stenosis with severe left ventricular dysfunction. Prognostic indicators. Circulation. 1997; 95:2395–2400.5. Tarantini G, Buja P, Scognamiglio R, et al. Aortic valve replacement in severe aortic stenosis with left ventricular dysfunction: determinants of cardiac mortality and ventricular function recovery. Eur J Cardiothorac Surg. 2003; 24:879–885.6. Powell DE, Tunick PA, Rosenzweig BP, et al. Aortic valve replacement in patients with aortic stenosis and severe left ventricular dysfunction. Arch Intern Med. 2000; 160:1337–1341.7. Clavel MA, Fuchs C, Burwash IG, et al. Predictors of outcomes in low-flow, low-gradient aortic stenosis: results of the multicenter TOPAS Study. Circulation. 2008; 118:14 Suppl. S234–S242.8. Levy F, Laurent M, Monin JL, et al. Aortic valve replacement for low-flow/low-gradient aortic stenosis operative risk stratification and long-term outcome: a European multicenter study. J Am Coll Cardiol. 2008; 51:1466–1472.9. Hein S, Arnon E, Kostin S, et al. Progression from compensated hypertrophy to failure in the pressure-overloaded human heart: structural deterioration and compensatory mechanisms. Circulation. 2003; 107:984–991.10. Krayenbuehl HP, Hess OM, Monrad ES, Schneider J, Mall G, Turina M. Left ventricular myocardial structure in aortic valve disease before, intermediate, and late after aortic valve replacement. Circulation. 1989; 79:744–755.11. Maron BJ, Ferrans VJ, Roberts WC. Myocardial ultrastructure in patients with chronic aortic valve disease. Am J Cardiol. 1975; 35:725–739.12. Villari B, Vassalli G, Monrad ES, Chiariello M, Turina M, Hess OM. Normalization of diastolic dysfunction in aortic stenosis late after valve replacement. Circulation. 1995; 91:2353–2358.13. Hess OM, Ritter M, Schneider J, Grimm J, Turina M, Krayenbuehl HP. Diastolic stiffness and myocardial structure in aortic valve disease before and after valve replacement. Circulation. 1984; 69:855–865.14. Weidemann F, Herrmann S, Störk S, et al. Impact of myocardial fibrosis in patients with symptomatic severe aortic stenosis. Circulation. 2009; 120:577–584.15. Azevedo CF, Nigri M, Higuchi ML, et al. Prognostic significance of myocardial fibrosis quantification by histopathology and magnetic resonance imaging in patients with severe aortic valve disease. J Am Coll Cardiol. 2010; 56:278–287.16. Bonow RO, Carabello BA, Chatterjee K, et al. 2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2008; 118:e523–e661.17. Vahanian A, Alfieri O, Andreotti F, et al. Guidelines on the management of valvular heart disease (version 2012): the Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardiothorac Surg. 2012; 42:S1–S44.18. Nagueh SF, Appleton CP, Gillebert TC, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009; 22:107–133.19. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.20. TTE/TEE Appropriateness Criteria Writing Group. Douglas PS, Khandheria B, et al. ACCF/ASE/ACEP/ASNC/SCAI/SCCT/SCMR 2007 appropriateness criteria for transthoracic and transesophageal echocardiography: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American Society of Echocardiography, American College of Emergency Physicians, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society for Cardiovascular Magnetic Resonance. Endorsed by the American College of Chest Physicians and the Society of Critical Care Medicine. J Am Soc Echocardiogr. 2007; 20:787–805.21. Hovda S, Rue H, Olstad B. New echocardiographic imaging method based on the bandwidth of the ultrasound Doppler signal with applications in blood/tissue segmentation in the left ventricle. Comput Methods Programs Biomed. 2008; 92:279–288.22. Bondarenko O, Beek AM, Hofman MB, et al. Standardizing the definition of hyperenhancement in the quantitative assessment of infarct size and myocardial viability using delayed contrast-enhanced CMR. J Cardiovasc Magn Reson. 2005; 7:481–485.23. Kim RJ, Wu E, Rafael A, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000; 343:1445–1453.24. Simonetti OP, Kim RJ, Fieno DS, et al. An improved MR imaging technique for the visualization of myocardial infarction. Radiology. 2001; 218:215–223.25. Wu E, Judd RM, Vargas JD, Klocke FJ, Bonow RO, Kim RJ. Visualisation of presence, location, and transmural extent of healed Q-wave and non-Q-wave myocardial infarction. Lancet. 2001; 357:21–28.26. Mahrholdt H, Wagner A, Judd RM, Sechtem U, Kim RJ. Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur Heart J. 2005; 26:1461–1474.27. Rochitte CE, Oliveira PF, Andrade JM, et al. Myocardial delayed enhancement by magnetic resonance imaging in patients with Chagas' disease: a marker of disease severity. J Am Coll Cardiol. 2005; 46:1553–1558.28. McCrohon JA, Moon JC, Prasad SK, et al. Differentiation of heart failure related to dilated cardiomyopathy and coronary artery disease using gadolinium-enhanced cardiovascular magnetic resonance. Circulation. 2003; 108:54–59.29. Moon JC, Reed E, Sheppard MN, et al. The histologic basis of late gadolinium enhancement cardiovascular magnetic resonance in hypertrophic cardiomyopathy. J Am Coll Cardiol. 2004; 43:2260–2264.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aortic Valve Replacement with Pulmonary Autograft in Patient with Congenital Aortic Stenosis : Ross Procedure without Homograft: one case report
- The Influence of the Left Ventricular Geometry on the Left Atrial Size and Left Ventricular Filling Pressure in Hypertensive Patients, as Assessed by Echocardiography
- Exercise Echocardiography in Asymptomatic Patients with Severe Aortic Stenosis and Preserved Left Ventricular Ejection Fraction
- Mass Reduction and Functional Improvement of the Left Ventricle after Aortic Valve Replacement for Degenerative Aortic Stenosis
- Angiographic analysis of congenital aortic stenosis: study in 20 patients excluding valvular stenosis