Clin Exp Otorhinolaryngol.
2011 Sep;4(3):137-141.
The Reconstruction of Nasal Septal Perforation with High Density Porous Polyethylene Covered with Fascia Lata: An Experimental Study on Rabbit Model
- Affiliations
-
- 1ENT Department, Okmeydani Education and Research Hospital, Istanbul, Turkey. dr.gyildirim@yahoo.com.tr
- 2Anatomy Department, Istanbul University Faculty of Veterinary Medicine, Istanbul, Turkey.
- 3ENT Department, Bakirkoy Sadi Konuk Education and Research Hospital, Istanbul, Turkey.
- 4Radiology Department, Okmeydani Education and Research Hospital, Istanbul, Turkey.
- 5Pathology Department, Okmeydani Education and Research Hospital, Istanbul, Turkey.
Abstract
OBJECTIVES
Evaluation of a new material, high-density porous polyethylene (HDPP), which is covered with fascia lata, for experimental nasal septal perforation closure.
METHODS
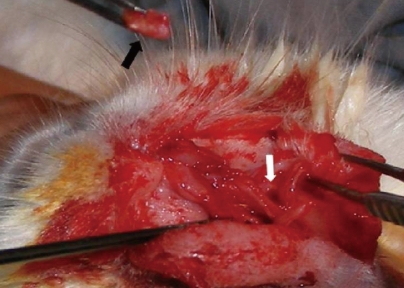
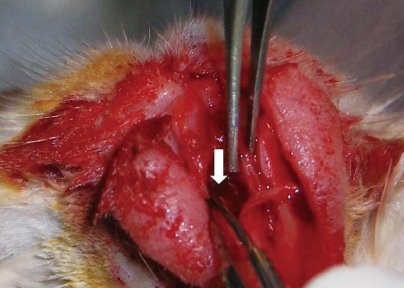
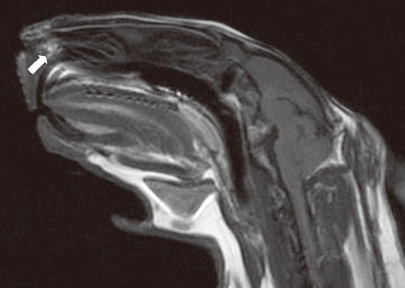
Twenty New Zealand albino rabbits were included and divided into study and control groups. A lateral incision was made from the lateral aspect of the left nares to the incisura nasomaxillaris. After exposure of the cavum nasi, the nasal mucoperichondrium was elevated bilaterally. A full-thickness 0.5x0.5-cm perforation was created over the septum nasi with a No. 11 surgical blade. A fascia lata graft was used for the study group. The HDPP was covered with fascia lata and placed under the elevated mucosa. HDPP without a fascial covering was used in the control group. Four months after the procedure, magnetic resonance imaging was performed to evaluate resorption of the material. The animals were sacrificed, and the nasal septum was completely removed. Macroscopic and histopathological examinations were performed on the nasal septum.
RESULTS
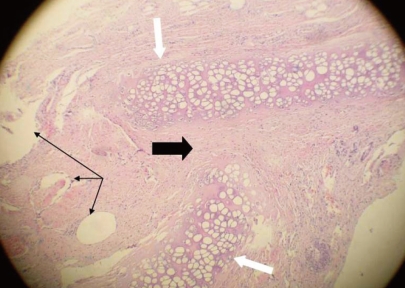
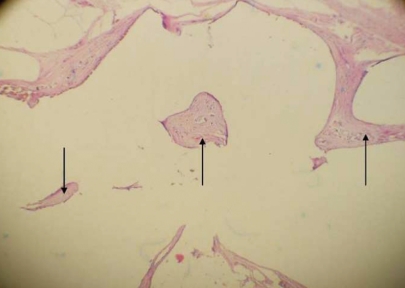
All rabbits had survived after the 4-month period. Macroscopically, nine of 10 (90%) perforations were closed in the fascia lata-covered HDPP group. Histopathological examination of these nine rabbits revealed that the continuity of cartilage was disturbed in the perforation areas. Granulation tissue was inverted in areas in which the cartilage continuity was disturbed. The HDPP had remained intact at the edge of the perforation. In the HDPP group, six of 10 implants were still perforated (60%) and four (40%) were closed. The fascia lata-covered HDPP implant had a significantly higher perforation closure rate than that of the HDPP implant alone (P<0.05).
CONCLUSION
In cases of septal perforation, it is better to cover the HDPP implant with fascia lata. This covered implant can be used for the repair of nasal septal perforations. HDPP implants are easy to work with and avoid the increased operative time and morbidity associated with harvesting autografts.
MeSH Terms
Figure
Reference
-
1. Seyhan T, Kircelli BH, Caglar B. Correction of septal and midface hypoplasia in maxillonasal dysplasia (Binder's syndrome) using high-density porous polyethylene. Aesthetic Plast Surg. 2009; 7. 33(4):661–665. PMID: 19205792.
Article2. Re M, Paolucci L, Romeo R, Mallardi V. Surgical treatment of nasal septal perforations: our experience. Acta Otorhinolaryngol Ital. 2006; 4. 26(2):102–109. PMID: 16886852.3. Pedroza F, Patrocinio LG, Arevalo O. A review of 25-year experience of nasal septal perforation repair. Arch Facial Plast Surg. 2007; Jan-Feb. 9(1):12–18. PMID: 17224482.
Article4. Dosen LK, Haye R. Nasal septal perforation 1981-2005: changes in etiology, gender and size. BMC Ear Nose Throat Disord. 2007; 3. 07. 7:1. PMID: 17343747.
Article5. Kogan L, Gilbey P, Samet A, Talmon Y. Nasal septal perforation repair using oral mucosal flaps. Isr Med Assoc J. 2007; 5. 9(5):373–375. PMID: 17591376.6. Goh AY, Hussain SS. Different surgical treatments for nasal septal perforation and their outcomes. J Laryngol Otol. 2007; 5. 121(5):419–426. PMID: 17250780.
Article7. Ambro BT, Zimmerman J, Rosenthal M, Pribitkin EA. Nasal septal perforation repair with porcine small intestinal submucosa. Arch Facial Plast Surg. 2003; Nov-Dec. 5(6):528–529. PMID: 14623693.
Article8. Ceylan A, Ileri F, Celenk F, Yilmaz M, Uslu S. Upper lateral cartilage inner mucoperichondrial flap technique for the repair of nasal septal perforation. ORL J Otorhinolaryngol Relat Spec. 2007; 69(4):245–250. PMID: 17409784.
Article9. Baj A, Spotti S, Marelli S, Beltramini GA, Gianni AB. Use of porous polyethylene for correcting defects of temporal region following transposition of temporalis myofascial flap. Acta Otorhinolaryngol Ital. 2009; 10. 29(5):265–269. PMID: 20162028.10. Keefe MS, Keefe MA. An evaluation of the effectiveness of different techniques for intraoperative infiltration of antibiotics into alloplastic implants for use in facial reconstruction. Arch Facial Plast Surg. 2009; Jul-Aug. 11(4):246–251. PMID: 19620530.
Article11. Oliveira RV, de Souza Nunes LS, Filho HN, de Andrade Holgado L, Ribeiro DA, Matsumoto MA. Fibrovascularization and osteogenesis in high-density porous polyethylene implants. J Craniofac Surg. 2009; 7. 20(4):1120–1124. PMID: 19553849.
Article12. Yildirim G, Haliloglu T, Sapci T, Kahvecioglu O, Onar V, Savci N, et al. Tracheal reconstruction with porous high-density polyethylene tracheal prosthesis. Ann Otol Rhinol Laryngol. 2000; 10. 109(10 Pt 1):981–987. PMID: 11051440.
Article13. Ribeiro JS, da Silva GS. Technical advances in the correction of septal perforation associated with closed rhinoplasty. Arch Facial Plast Surg. 2007; Sep-Oct. 9(5):321–327. PMID: 17875824.
Article14. Godin MS, Waldman SR, Johnson CM Jr. Nasal augmentation using Gore-Tex: a 10-year experience. Arch Facial Plast Surg. 1999; Apr-Jun. 1(2):118–121. PMID: 10937089.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Excision of a Nasal Dermoid Sinus Cyst via Open Rhinoplasty Approach and Primary Reconstruction Using Tutoplast-Processed Fascia Lata
- Repair of Nasal Septal Perforation Using Polycaprolactone Plate and Temporalis Fascia Graft
- Complete Septal Extension Graft using Porous High-Density Polyethylene Sheet or Septal Cartilage in Unilateral Cleft Lip Nasal Deformities: Photogrammetric Analysis
- Surgical repair of nasal septal perforation using temporalis fascia and homologous rib cartilage grafts: a case report
- Extensional midline framework built with porous polyethylene implant (Medpor) in rhinoplasty