Ann Dermatol.
2009 May;21(2):136-141. 10.5021/ad.2009.21.2.136.
Comparative Study of the Gross Interpretation of Phototesting and Objective Measurement with Using a Spectrophotometer for Patients with Psoriasis and Vitiligo Treated with Narrow-band UVB
- Affiliations
-
- 1Department of Dermatology, College of Medicine, Dong-A University, Busan, Korea. mucca@dau.ac.kr
- KMID: 2219381
- DOI: http://doi.org/10.5021/ad.2009.21.2.136
Abstract
- BACKGROUND
Determination of the minimal erythema dose (MED) is important for developing a phototherapy protocol and to diagnosis photosensitivity disorders. But obtaining a precise and reproducible MED is quite difficult because a phototest for erythema is based on subjective assessment.
OBJECTIVE
The objective of our study was to compare the gross interpretation of a phototest and the objective measurement using a spectrophotometer for determining the parameters of cutaneous narrow-band UVB (NBUVB) therapy.
METHODS
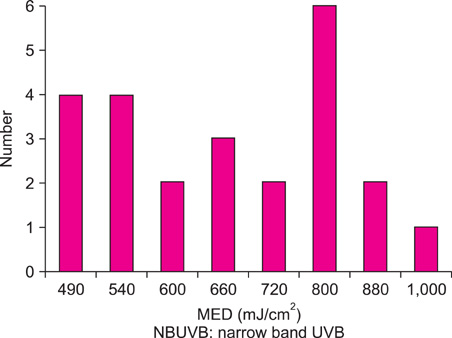
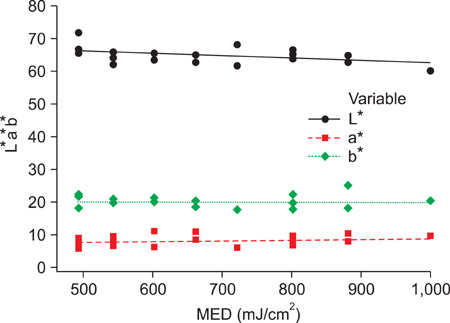
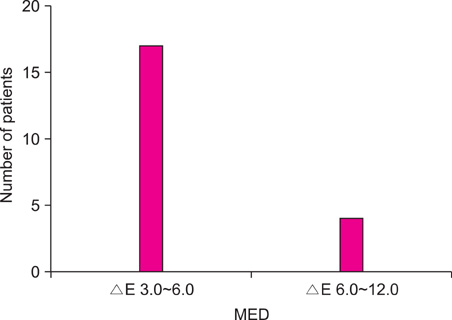
A total of 14 psoriasis and 10 vitiligo patients who receiving NBUVB phototherapy with skin types III and IV were selected for this study. To perform phototesting, ten sites on the skin of the back were vertically exposed to a series of 10 NBUVB doses among 14 doses between 340 and 1,400 mJ/cm2. We interpreted the gross findings of erythema and measured the L*a*b* values with using a spectrophotometer at each phototest spot and at the control skin. Also, we evaluate the relationship between the gross presentation and the spectrophotometric analysis by delta E for the assessment of the minimal perceptible erythema (MPE) and MED.
RESULTS
For all the subjects, the MEDs were measured in the 490~1,000 mJ/cm2 range. The average of the colorimetric values for the control skin were L*: 64.8, a*: 7.9 and b*: 19.8. Among them, the L* value and MED value were shown to be inversely correlated, and as the L* value was decreased, the MED was increased. For the MPE, the delta E, which was the color difference of the normal skin and the phototest area, was within the range of 1.5~3.0 in 17 of the 21 patients, and 4 patients were within the range of 1.0~1.5. For the MED, among the 21 patients, the delta E of 17 patients was within the range of 3.0~6.0, and 4 patients were within the range of 6.0~12.0.
CONCLUSION
A spectrophotometer enables UV erythema to be assessed objectively and quantitatively, and this can compensate for the disadvantages of subjective gross interpretation when determining the MED. Delta E is a good novel and objective indicator for determining the MPE and MED. So, a spectrophotometer is a very useful instrument for developing a phototherapy protocol for psoriasis and other dermatoses and for making the diagnosis of photosensitivity disorders.
Keyword
Figure
Cited by 1 articles
-
Spectrophotometric Measurement of Minimal Erythema Dose Sites after Narrowband Ultraviolet B Phototesting: Clinical Implication of Spetrophotometric Values in Phototherapy
Su-Young Jeon, Chae-Young Lee, Ki-Hoon Song, Ki-Ho Kim
Ann Dermatol. 2014;26(1):17-25. doi: 10.5021/ad.2014.26.1.17.
Reference
-
1. Choe YB, Park SB, Yoon JI. Narrow-band UVB phototherapy in Korean psoriasis patients. Korean J Dermatol. 2000. 38:358–362.2. Rim JH, Choe YB, Youn JI. Minimal erythema dose of narrow band UVB in Korean psoriasis patients. Korean J Dermatol. 2001. 39:883–886.3. Park SB, Huh CH, Choe YB, Youn JI. Time course of ultraviolet-induced skin reactions evaluated by two different reflectance spectrophotometers: DermaSpectrophotometer and Minolta spectrophotometer CM-2002. Photodermatol Photoimmunol Photomed. 2002. 18:23–28.
Article4. Youn JI, Park JY, Jo SJ, Rim JH, Choe YB. Assessment of the usefulness of skin phototype and skin color as the parameter of cutaneous narrow band UVB sensitivity in psoriasis patients. Photodermatol Photoimmunol Photomed. 2003. 19:261–264.
Article5. Österberg F. The visual impact of lamination [Internet]. 2005. 02. 08. cited 2007 Nov 6. Sweden: Linköpings universitet, Department of Science and Technology;Available from: http://www.t2f.nu/t2frapp_f_144.pdf.6. Farr PM, Diffey BL. Quantitative studies on cutaneous erythema induced by ultraviolet radiation. Br J Dermatol. 1984. 111:673–682.
Article7. Picot E, Meunier L, Picot-Debeze MC, Peyron JL, Meynadier J. Treatment of psoriasis with a 311-nm UVB lamp. Br J Dermatol. 1992. 127:509–512.
Article8. Karvonen J, Kokkonen EL, Ruotsalainen E. 311 nm UVB lamps in the treatment of psoriasis with the Ingram regimen. Acta Derm Venereol. 1989. 69:82–85.9. Picot E, Picot-Debeze MC, Meunier L, Peyron JL, Meynadier J. Narrow-band UVB phototherapy (Philips TL01 lamps) in psoriasis. Ann Dermatol Venereol. 1992. 119:639–642.10. Taylor S, Westerhof W, Im S, Lim J. Noninvasive techniques for the evaluation of skin color. J Am Acad Dermatol. 2006. 54:S282–S290.
Article11. Andersen PH, Abrams K, Maibach H. Ultraviolet B dose-dependent inflammation in humans: a reflectance spectroscopic and laser Doppler flowmetric study using topical pharmacologic antagonists on irradiated skin. Photodermatol Photoimmunol Photomed. 1992. 9:17–23.12. Zachariae R, Oster H, Bjerring P. Effects of hypnotic suggestions on ultraviolet B radiation-induced erythema and skin blood flow. Photodermatol Photoimmunol Photomed. 1994. 10:154–160.13. Kawana S, Ochiai H, Tachihara R. Objective evaluation of the effect of intense pulsed light on rosacea and solar lentigines by spectrophotometric analysis of skin color. Dermatol Surg. 2007. 33:449–454.
Article14. Yap AU, Sim CP, Loh WL, Teo JH. Human-eye versus computerized color matching. Oper Dent. 1999. 24:358–363.15. Jorgenson MW, Goodkind RJ. Spectrophotometric study of five porcelain shades relative to the dimensions of color, porcelain thickness, and repeated firings. J Prosthet Dent. 1979. 42:96–105.
Article16. Kuehni RG. Color-tolerance data and the tentative CIE 1976 L a b formula. J Opt Soc Am. 1976. 66:497–500.17. Barath VS, Faber FJ, Westland S, Niedermeier W. Spectrophotometric analysis of all-ceramic materials and their interaction with luting agents and different backgrounds. Adv Dent Res. 2003. 17:55–60.
Article18. Horn DJ, Bulan-Brady J, Hicks ML. Sphere spectrophotometer versus human evaluation of tooth shade. J Endod. 1998. 24:786–790.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Narrow-Band UVB Phototherapy in Vitiligo Patients
- Narrow-Band UVB Phototherapy in Korean Psoriasis Patients
- Narrow-band UVB as a Tool of Vitiligo Treatment
- Minimal Erythema Dose of Narrow Band UVB in Korean Psoriasis Patients
- The Study of Dose Incremental Regimen for Narrow-Band UVB Phototherapy in Psoriatic patients