J Korean Ophthalmol Soc.
2014 Mar;55(3):426-431. 10.3341/jkos.2014.55.3.426.
A Case of Optic Neuropathy Caused by Fungal Ball in an Onodi Cell
- Affiliations
-
- 1Department of Ophthalmology, KyungHee University Hospital, Kyung Hee University School of Medicine, Seoul, Korea. ikpark@medigate.net
- 2Department of Ophthalmology, KyungHee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea.
- KMID: 2218274
- DOI: http://doi.org/10.3341/jkos.2014.55.3.426
Abstract
- PURPOSE
To report a rare case of optic neuropathy caused by a fungal ball in an Onodi cell.
CASE SUMMARY
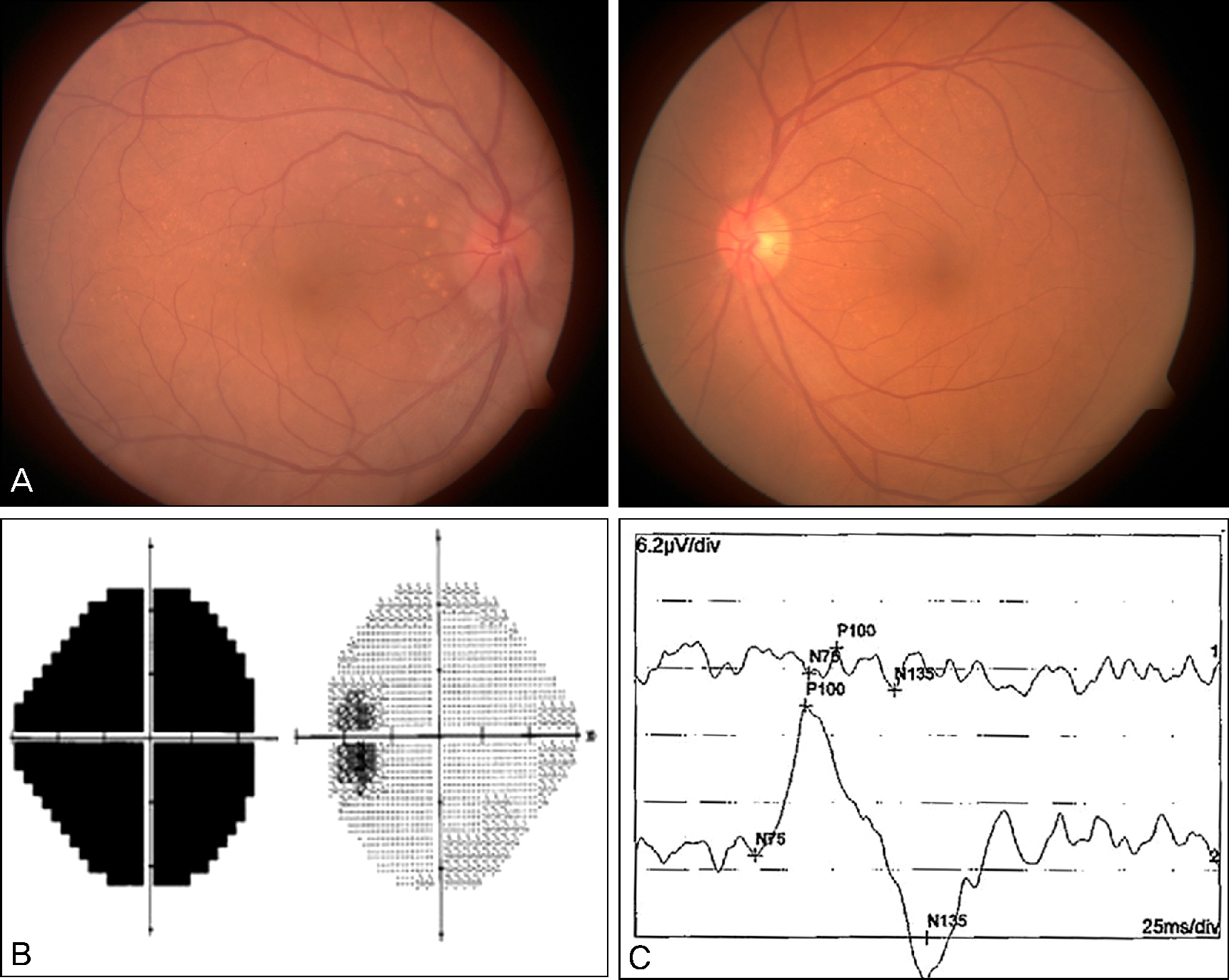
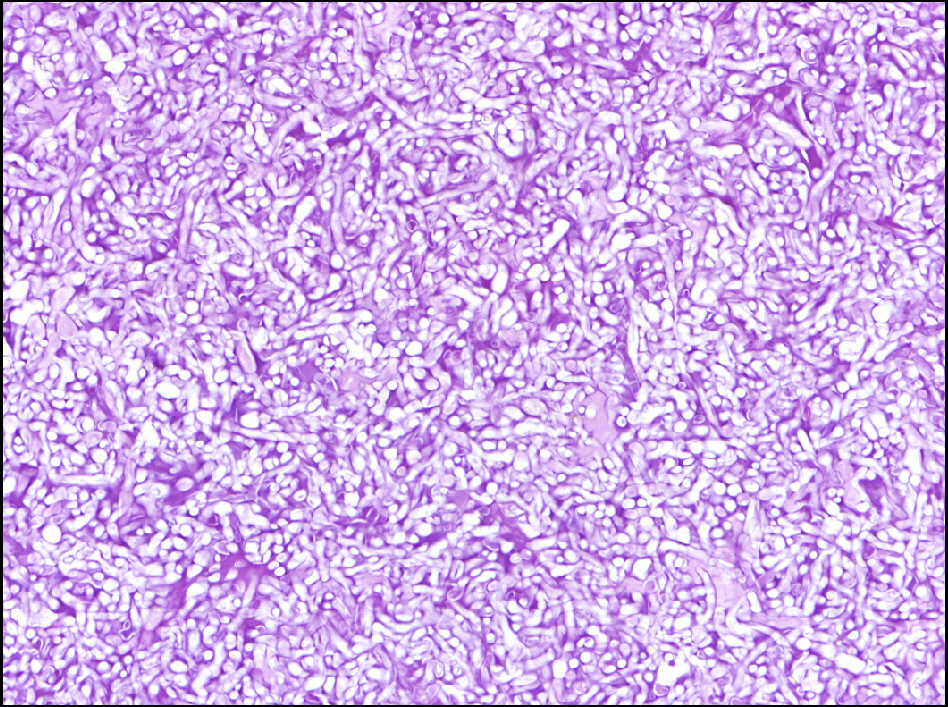
A 63-year-old female was referred to our clinic with relapsed visual loss and ocular pain in the right eye. She had been diagnosed as optic neuritis 14 days before and given pulse steroid therapy. She recovered to normal but relapsed 7 days before. In medical referral there was no suspected multiple sclerosis but only a few inflammation in the paranasal sinuses. On our initial examination, best corrected visual acuity was counting finger at 10 cm in the right eye, and 1.0 in the left eye, along with relative afferent pupillary defect in the right eye. The fundoscopic examinations disclosed disc swelling; nearly total visual field defect was observed on visual field examination and visual evoked potential test revealed decreased amplitude at P100 wave in the right eye. Clinical impression was relapsed optic neuritis. After the administration of pulse steroid therapy, her disc swelling was decreased and visual acuity was recovered to 0.6, however, visual acuity was exacerbated to 0.4 in 2 weeks. We checked outside brain magnetic resonance imaging (MRI) and the result showed optic neuropathy caused by a fungal ball in an Onodi cell. The patient was referred to otorhinolaryngologist and fungal ball was removed by endoscopic sinus surgery. 3 weeks after surgery the patient's visual acuity was 0.9, no disc swelling was found and visual evoked potential was recovered to normal.
CONCLUSIONS
An Onodi cell lesion should be considered in the differential diagnosis of optic neuritis, identified by imaging studies and promptly removed by surgery for visual recovery.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A Case of Visual Loss Caused by Invasive Fungal Sinusitis of the Onodi Cell
Tae Woo Gim, Seok Chan Yoo, Seok Yoon Lee, Jong In Jeong
Korean J Otorhinolaryngol-Head Neck Surg. 2021;64(4):273-276. doi: 10.3342/kjorl-hns.2020.00458.
Reference
-
References
1. Fukuda Y, Chikamatsu K, Ninomiya H, et al. Mucocele in an Onodi cell with simultaneous bilateral visual disturbance. Auris Nasus Larynx. 2006; 33:199–202.
Article2. Kitagawa K, Hayasaka S, Shimizu K, Nagaki Y. Optic neuropathy produced by a compressed mucocele in an Onodi cell. Am J Ophthalmol. 2003; 135:253–4.
Article3. Tomovic S, Esmaeili A, Chan NJ, et al. High-resolution computed tomography analysis of the prevalence of Onodi cells. Laryngoscope. 2012; 122:1470–3.
Article4. Nickerson JP, Lane AP, Subramanian PS, Izbudak I. Onodi cell mucocele causing acute vision loss: radiological and surgical correlation. Clin Neuroradiol. 2011; 21:245–8.5. Vaphiades MS, Yunker JJ, Roberson GH, et al. Optic neuritis is nothing to sneeze at. Surv Ophthalmol. 2007; 52:106–10.
Article6. Nicolai P, Lombardi D, Tomenzoli D, et al. Fungus ball of the paranasal sinuses: experience in 160 patients treated with endoscopic surgery. Laryngoscope. 2009; 119:2275–9.
Article7. Oh DE, Kim YD. Visual loss due to inflammatory sinus diseases. J Korean Ophthalmol Soc. 2006; 47:1879–86.8. Dufour X, Kauffmann-Lacroix C, Ferrie JC, et al. Paranasal sinus fungus ball and surgery: a review of 175 cases. Rhinology. 2005; 43:34–9.9. Pagella F, Matti E, De Bernardi F, et al. Paranasal sinus fungus ball: diagnosis and management. Mycoses. 2007; 50:451–6.
Article10. Aribandi M, McCoy VA, Bazan C 3rd. Imaging features of in-vasive and noninvasive fungal sinusitis: a review. Radiographics. 2007; 27:1283–96.
Article11. Nonaka M, Fukumoto A, Nonaka R, et al. A case of a mucocele in an Onodi cell. J Nippon Med Sch. 2007; 74:325–8.
Article12. Loo JL, Looi AL, Seah LL. Visual outcomes in patients with paranasal mucoceles. Ophthal Plast Reconstr Surg. 2009; 25:126–9.
Article13. Toh ST, Lee JC. Onodi cell mucocele: rare cause of optic compressive neuropathy. Arch Otolaryngol Head Neck Surg. 2007; 133:1153–6.14. Wu W, Sun MT, Cannon PS, et al. Recovery of visual function in a patient with an Onodi cell mucocele compressive optic neuropathy who had a 5-week interval between onset and surgical intervention: a case report. J Ophthalmol. 2010; 2010:483056.
Article15. Lee JH, Hong YH, Mun SK. A case of fungal sphenoid sinusitis with visual loss. Korean J Med Mycol. 2011; 16:109–12.16. Cho SH, Jin BJ, Lee YS, et al. Orbital apex syndrome in a patient with sphenoid fungal balls. Clin Exp Otorhinolaryngol. 2009; 2:52–4.
Article17. Choo IS, Choi JY, Kim DH, et al. Acute optic neuropathy due to compression by posterior ethomoidal cell (an Onodi cell) mucocele. J Korean Neurol Assoc. 2009; 27:421–3.18. deShazo RD, Chapin K, Swain RE. Fungal sinusitis. N Engl J Med. 1997; 337:254–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Fungal Infection in the Onodi Cell with Diplopia
- A Case of Fungal Infection in Onodi Cell with Visual Loss
- A Case of Visual Loss Caused by Invasive Fungal Sinusitis of the Onodi Cell
- Acute Optic Neuropathy due to Compression by Posterior Ethomoidal Cell (an Onodi cell) Mucocele
- Acute Visual Loss Caused by Onodi Cell Mucopyocele