J Korean Ophthalmol Soc.
2014 Mar;55(3):408-415. 10.3341/jkos.2014.55.3.408.
Fixation of the Eyeball to the Periosteum Over the Posterior Lacrimal Crest in Inveterate Exotropia
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. ophjun@gmail.com
- 2Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea.
- KMID: 2218271
- DOI: http://doi.org/10.3341/jkos.2014.55.3.408
Abstract
- PURPOSE
To report the results obtained after fixation of the eyeball to the periosteum over the posterior lacrimal crest in 5 cases of inveterate exotropia.
METHODS
From September 2011 to January 2013, 5 patients with inveterate exotropia and a history of surgery for exotropia underwent fixation of the eyeball to the periosteum over the posterior lacrimal crest.
RESULTS
The mean preoperative exotropia of 35 +/- 10.61 PD changed to esotropia of 5.8 +/- 17.28 PD at the one week postoperative visit and exotropia of 13.2 +/- 11.34 PD at the final postoperative visit (mean, 6.05 months after surgery). At the final postoperative visit, 2 patients who had ocular adhesion due to trauma showed 25 PD exotropia. None of the patients showed injuries to the lacrimal system, but 2 patients showed conjunctival granuloma.
CONCLUSIONS
Fixation of the eyeball to the periosteum over the posterior lacrimal crest is an effective approach for the management of inveterate exotropia, except in cases of exotropia combined with ocular adhesion.
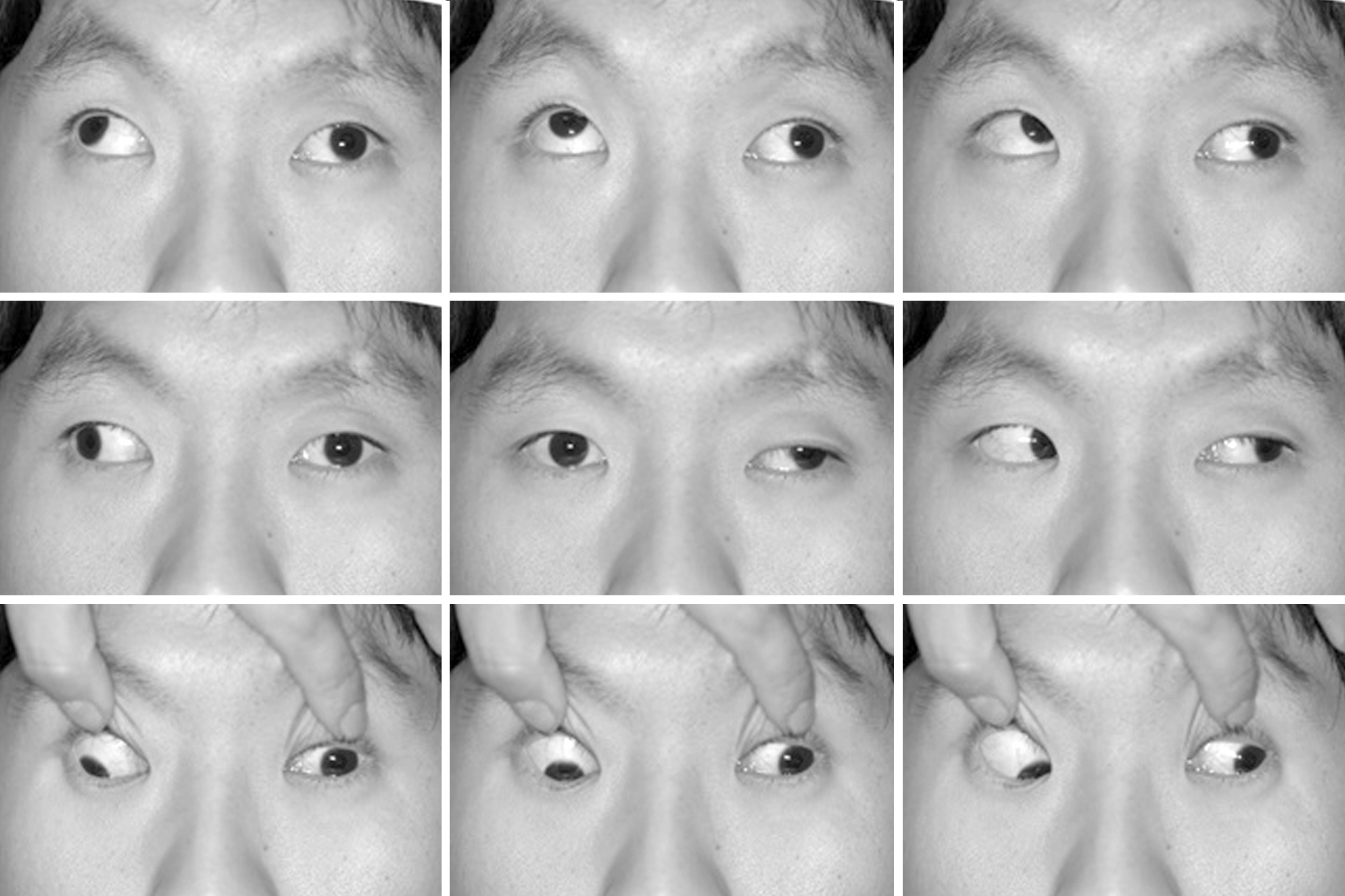
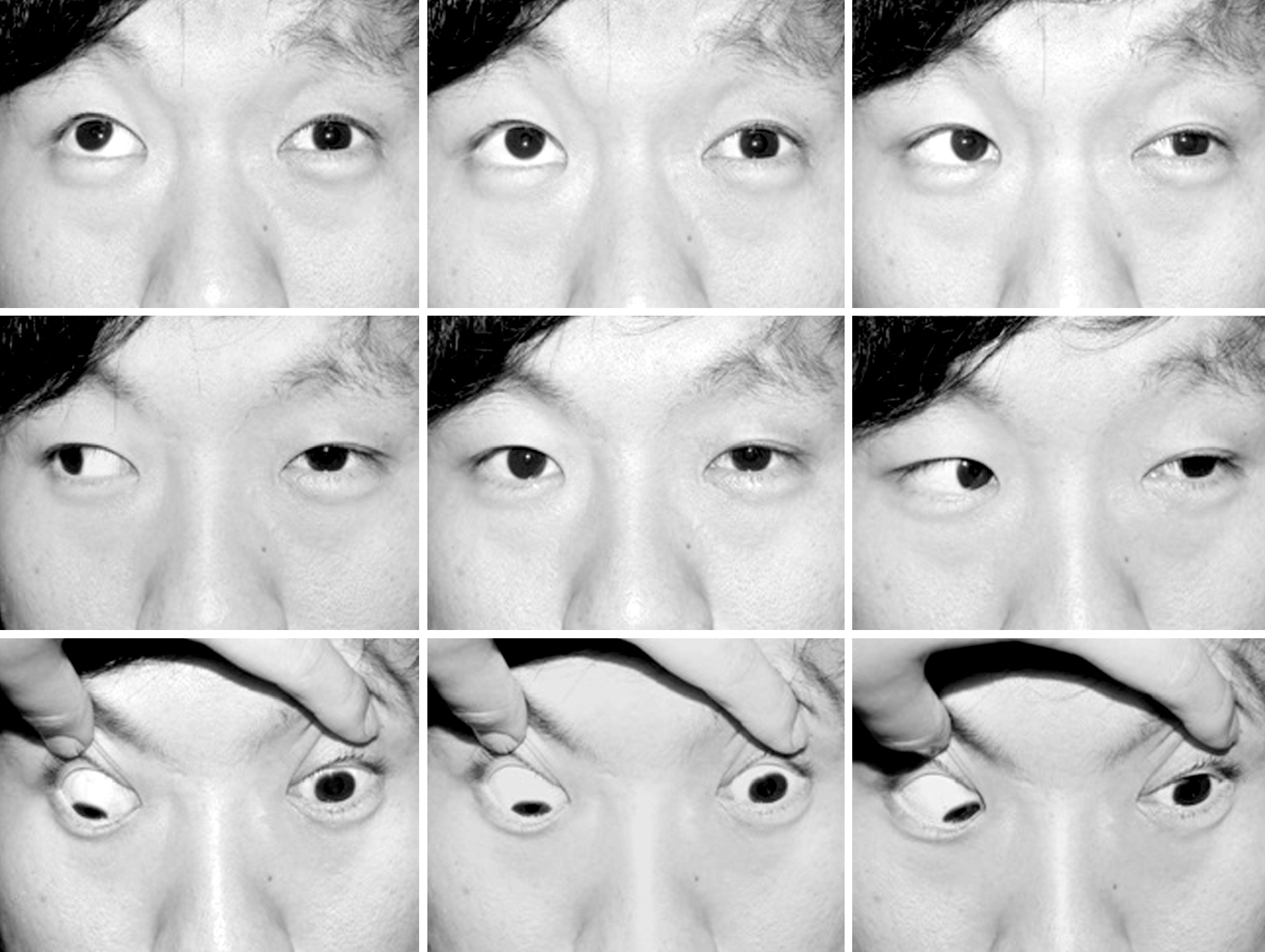
Figure
Cited by 1 articles
-
Periosteal Fixation Applied to Patients with Large-angle Paralytic Strabismus
Hee Dong Eom, Young Ki Kwon, Byeong Jae Son, Bo Young Chun
J Korean Ophthalmol Soc. 2018;59(3):268-275. doi: 10.3341/jkos.2018.59.3.268.
Reference
-
References
1. Von Noorden GK. Binocular vision and ocular motility. 3rd ed.St. Louis: CV Mosby;1985. p. 369.2. Cho YA, Rah SH, Kim MM, Lee JY. Vertical rectus muscles transposition in large exotropia with medial rectus muscle transection following endoscopic sinus surgery. Korean J Ophthalmol. 2008; 22:104–10.
Article3. Thacker NM, Velez FG, Demer JL, Rosenbaum AL. Strabismic complications following endoscopic sinus surgery: diagnosis and surgical management. J AAPOS. 2004; 8:488–94.
Article4. Rosenbaum AI, Santiago AP. Clinical strabismus management principles and surgical technique. Philadelphia: WB Saunders;1999. p. 252.5. Helveston EM. Muscle transposition procedures. Surv Ophthalmol. 1972; 16:92–7.6. Helveston EM. Atlas of Strabismus Surgery. 3rd ed.St. Louis: CV Mosby;1985. p. 254–9.7. Von Noorden GK. Binocular vision and ocular motility. 5th ed.St. Louis: CV Mosby;1996. p. 422.8. Peter LC. The use of the superior oblique as an internal rotator in third nerve paralysis. Trans Am Ophthalmol. 1933; 31:232–7.9. Jackson E. Surgery of the eye. 3rd ed.Vol. 1. New York: Grune & Stratton;1952. p. 405.10. Scott AB. Transposition of the superior oblique. Am Orthopt J. 1977; 27:11–4.
Article11. Morad Y, Kowal L, Scott AB. Lateral rectus muscle disinsertion and reattachment to the lateral orbital wall. Br J Ophthalmol. 2005; 89:983–5.
Article12. Saunders RA, Rogers GL. Superior oblique transposition for third nerve palsy. Ophthalmology. 1982; 89:310–6.
Article13. Salazar-León JA, Ramírez-Ortíz MA, Salas-Vargas M. The surgical correction of paralytic strabismus using fascia lata. J Pediatr Ophthalmol Strabismus. 1998; 35:27–32.
Article14. Srivastava KK, Sundaresh K, Vijayalakshmi P. A new surgical technique for ocular fixation in congenital third nerve palsy. J AAPOS. 2004; 8:371–7.
Article15. Sharma P, Gogoi M, Kedar S, Bhola R. Periosteal fixation in third-nerve palsy. J AAPOS. 2006; 10:324–7.
Article16. Goldberg RA, Rosenbaum AL, Tong JT. Use of apically based periosteal flaps as globe tethers in severe paralytic strabismus. Arch Ophthalmol. 2000; 118:431–7.17. Moe KS. The precaruncular approach to the medial orbit. Arch Facial Plast Surg. 2003; 5:483–7.
Article18. Saxena R, Sinha A, Sharma P, et al. Precaruncular approach for medial orbital wall periosteal anchoring of the globe in oculomotor nerve palsy. J AAPOS. 2009; 13:578–82.
Article19. Suk KW, Park JM, Kim SS, Lee SJ. Periosteal fixation in bilateral total third nerve palsy. J Korean Ophthalmol Soc. 2008; 49:1203–8.
Article20. Parks MM. Causes of the adhesive syndrome. Symposium on Strabismus. Transactions of the New Orleans Academy of Ophthalmology. St. Louis: CV Mosby;1978. p. 269–79.21. Wright KW. The fat adherence syndrome and strabismus after retina surgery. Ophthalmology. 1986; 93:411–5.
Article22. Johnson LV. Adherence syndrome; pseudoparalysis of the lateral or superior rectus muscles. AMA Arch Ophthalmol. 1950; 44:870–8.23. Dunlap EA. Plastic implants in muscle surgery: a study of the possible use of plastic materials in the management of extraocular motility restrictions. Trans Am Ophthalmol Soc. 1967; 65:393–470.24. Robinson MR, Lee SS, Rubin BI, et al. Topical corticosteroid therapy for cicatricial conjunctivitis associated with chronic graft-ver-sus-host disease. Bone Marrow Transplant. 2004; 33:1031–5.
Article25. Cruz OA. Evaluation of mitomycin to limit postoperative adhesions in strabismus surgery. J Pediatr Ophthalmol Strabismus. 1996; 33:89–92.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anatomical Study of Medial Orbit in Human Cadavers
- Periosteal Fixation in Bilateral Total Third Nerve Palsy
- A Case of Esotropia at Near and A Type Exotropia at Distance
- Surgical Results in Constant Exotropia According to Fixation Patterns
- Surgical Results in Constant Exotropia According to Fixation Patterns