J Korean Ophthalmol Soc.
2014 May;55(5):740-745. 10.3341/jkos.2014.55.5.740.
Risk Factors and Prognosis of Isolated Ischemic 3rd, 4th, 6th Cranial Nerve Palsy
- Affiliations
-
- 1Department of Ophthalmology, Chosun University School of Medicine, Gwangju, Korea. eyelovehyun@hanmail.net
- KMID: 2218096
- DOI: http://doi.org/10.3341/jkos.2014.55.5.740
Abstract
- PURPOSE
To investigate the clinical features and risk factors of ischemic third, fourth, sixth cranial nerve palsy.
METHODS
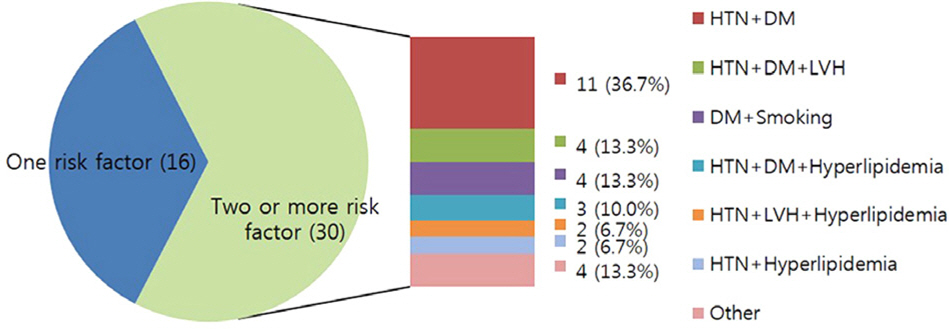
Retrospectively, we reviewed the medical records of 46 eyes of 46 patients who were diagnosed with ischemic third, fourth, sixth nerve palsy alone such as age of onset, risk factors, recovery rate and recovery time.
RESULTS
The mean age of onset was 64.9 years. Of the 46 patients, 15 patients (32.6%) in third cranial nerve palsy group, 15 patients (32.6%) in fourth cranial nerve palsy group, 16 patients (34.8%) in sixth cranial nerve palsy group. The risk factor of hypertension in 30 patients (65.2%) was the most common than other risk factors such as diabetes, hyperlipidemia, elevated blood hematocrit, ischemic heart disease, left ventricular hypertrophy, smoking. The mean number of risk factors was 2.3 +/- 0.5 in third cranial nerve palsy group, 1.6 +/- 1.1 in sixth cranial nerve palsy group, 1.4 +/- 1.1 in fourth cranial nerve palsy group. Of the 46 patients, 42 patients (91.3%) were recovered. There was no significant difference in recovery rate by cranial nerve palsy. Recovery time of intracranial abnormalities group (10.5 +/- 2.9 weeks) in brain imaging study was late as compared with that of no intracranial abnormalities group (7.5 +/- 5.1 weeks).
CONCLUSIONS
The overall recovery rate of isolated ischemic third, fourth, sixth cranial nerve was high. But if there are intracranial abnormalities in imaging study, it took a long time to recover. Also ischemic third cranial nerve palsy had multiple risk factors characteristically.
Keyword
MeSH Terms
-
Abducens Nerve
Abducens Nerve Diseases
Age of Onset
Cranial Nerve Diseases*
Hematocrit
Humans
Hyperlipidemias
Hypertension
Hypertrophy, Left Ventricular
Medical Records
Myocardial Ischemia
Neuroimaging
Oculomotor Nerve
Paralysis
Prognosis*
Retrospective Studies
Risk Factors*
Smoke
Smoking
Trochlear Nerve Diseases
Smoke
Figure
Reference
-
References
1. Rucker CW. Paralysis of the third, fourth and sixth cranial nerves. Am J Ophthalmol. 1958; 46:787–94.
Article2. Rucker CW. The causes of paralysis of the third, fourth and sixth cranial nerves. Am J Ophthalmol. 1966; 61:1293–8.
Article3. Rush JA, Younge BR. Paralysis of cranial nerves III, IV, and VI: Cause and prognosis in 1,000 cases. Arch Ophthalmol. 1981; 99:76–9.4. Richards BW, Jones FR Jr, Younge BR. Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am J Ophthalmol. 1992; 113:489–96.
Article5. Teuscher AU, Meienberg O. Ischaemic oculomotor nerve palsy. Clinical features and vascular risk factors in 23 patients. J Neurol. 1985; 232:144–9.6. Jacobson DM, McCanna TD, Layde PM. Risk factors for ischemic ocular motor nerve palsies. Arch Ophthalmol. 1994; 112:961–6.
Article7. Kobashi R, Ohtsuki H, Hasebe S. Clinical studies of ocular mo-tility disturbances: Part 2. Risk factors for ischemic ocular motor nerve palsy [corrected]. Jpn J Ophthalmol. 1997; 41:115–9.8. Park UC, Kim SJ, Hwang JM, Yu YS. Clinical features and natural history of acquired third, fourth, and sixth cranial nerve palsy. Eye (Lond). 2008; 22:691–6.
Article9. Kim HS, Lee JB, Han SH. Nontraumaticacquired paralytic strabismus. J Korean Ophthalmic Soc. 1994; 35:121–5.10. Choung HK, Chang BL. Clinical features of ischemic ophthalmoplegia caused by diabetes mellitus or hypertension. J Korean Ophthalmol Soc. 2002; 43:131–5.11. Berlit P. Isolated and combined pareses of cranial nerves III, IV, and VI: a retrospective study of 412 patients. J Neurol Sci. 1991; 103:10–5.
Article12. Green WR, Hackett ER, Schlezinger NS. Neuro-ophthalmologic evaluation of oculomotor nerve paralysis. Arch Ophthalmol. 1964; 72:154–67.
Article13. Kaplan NM. Systemic hypertension: mechanisms and diagnosis. In : Braun-wald E, editor. Heart Disease: A Textbook of Cardiovascular Medicine. 4th ed.Philadelphia, Pa: WB Saunders Co;1992. p. 822–3.14. Murchison AP, Gilbert ME, Savino PJ. Neuroimaging and acute ocular motor mononeuropathies: a prospective study. Arch Oph-thalmol. 2011; 129:301–5.15. Dormandy JA. Clinical significance of blood viscosity. Ann R Coll Surg Engl. 1970; 47:211–28.16. Dintenfass L. Blood viscosity, internal fluidity of the red cell, dy-namic coagulation and the critical capillary fadius as factors in the physiology and pathology of circulation and microcirculation. Med J Aust. 1968; 1:688–96.17. Rand PW, Lacombe E, Hunt HE, Austin WH. Viscosity of normal human blood under normothermic and hypothermic conditions. J Appl Physiol. 1964; 16:117–22.
Article18. Eckmann DM, Bowers S, Stecker M, Cheung AT. Hematocrit, vol-ume expander, temperature, and shear rate effects on blood viscosity. Anesth Analg. 2000; 91:539–45.
Article19. Baskurt OK, Meiselman HJ. Blood rheology and hemodynamics. Semin Thromb Hemost. 2003; 29:435–50.
Article20. Asbury AK, Aldrege H, Hershberg H, Fishcer CM. Oculomotor palsy in diabetes mellitus: a clinico-pathological study. Brain. 1970; 93:555–66.
Article21. Weber RB, Daroff RB, Mackey EA. Pathology of oculomotor nerve palsy in diabetics. Neurology. 1970; 20:835–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Associated Injuries and Prognosis in Traumatic Isolated 3rd, 4th, and 6th Cranial Nerve Palsies
- Analysis of Early Neuroimaging Results in Patients with Acute Isolated Ocular Motor Nerve Palsy
- The Etiology and Clinical Feature of the Third, Fourth, and Sixth Cranial Nerve Palsy
- A Case of Guillain-Barr Syndrome with 6th Cranial Nerve Palsy Complicated by Chronic Active Hepatitis B
- Isolated Unilateral Hypoglossal Nerve Palsy Following Transoral Endotracheal Intubation for Endoscopic Sinus Surgery