J Korean Ophthalmol Soc.
2013 Jun;54(6):932-937. 10.3341/jkos.2013.54.6.932.
Perception of 3-Dimensional (3D) Image after Successful Exotropia Surgery
- Affiliations
-
- 1The Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. shhan222@yuhs.ac
- 2Department of Radiology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2217270
- DOI: http://doi.org/10.3341/jkos.2013.54.6.932
Abstract
- PURPOSE
To investigate the perception of 3-dimensional (3D) image after successful exotropia surgery and compare with Titmus stereo test.
METHODS
A total of 23 children who underwent surgery for intermittent exotropia and 28 normal children were evaluated with a 3D laptop computer and Titmus stereo test.
RESULTS
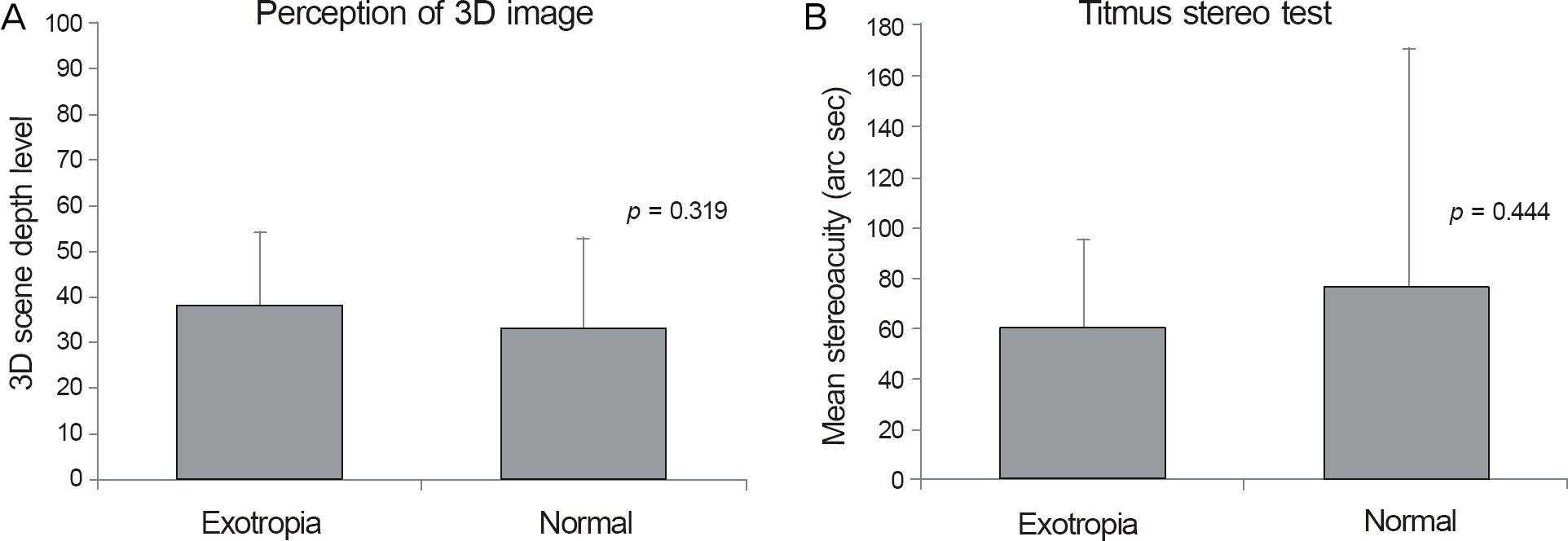
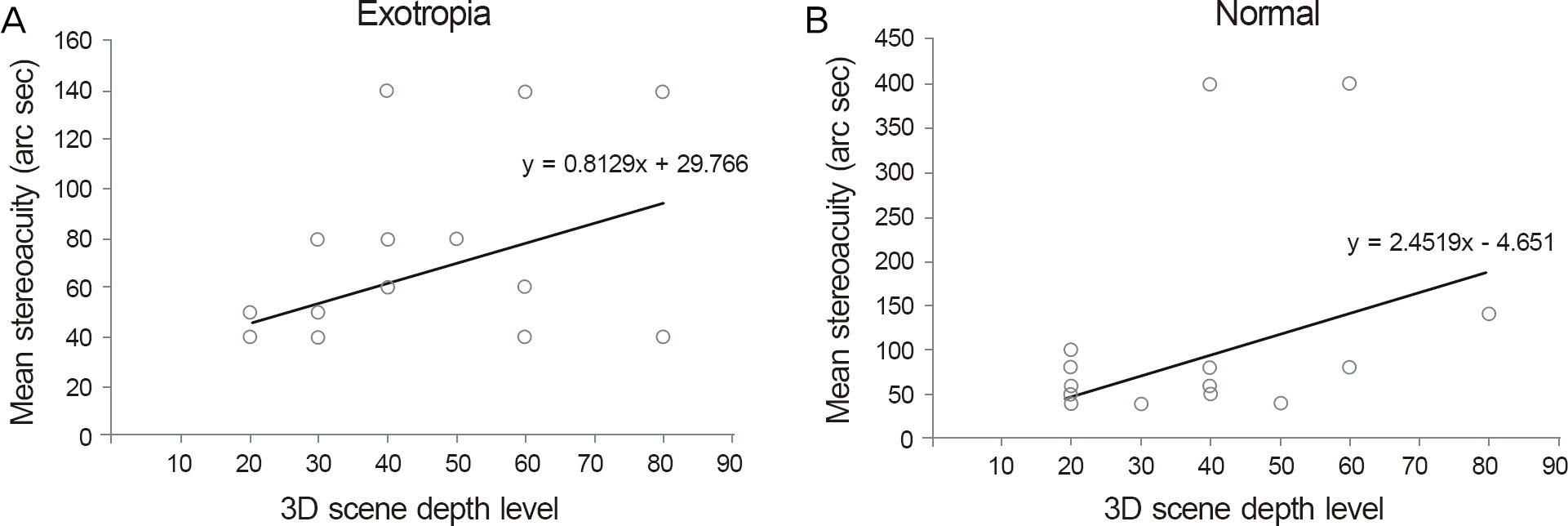
The mean minimal 3D scene depth level was 38.26 +/- 19.69 in the exotropia group and 33.21 +/- 16.11 in the normal group with no significant difference (p = 0.319). The mean stereoacuity was 60.97 +/- 34.23 arc sec in the exotropia group and 76.69 +/- 93.81 arc sec in the normal group with no significant difference (p = 0.444). The mean minimal 3D scene depth and mean stereoacuity showed statistically significant positive correlation in both the exotropia group (p = 0.024) and normal group (p = 0.026).
CONCLUSIONS
After a successful exotropia surgery, patients can normally perceive 3D images. Better 3D image perception can be predicted if a previously established stereo test shows good results.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Morrison D, McSwain W, Donahue S. Comparison of sensory outcomes in patients with monofixation versus bifoveal fusion after surgery for intermittent exotropia. J AAPOS. 2010; 14:47–51.
Article2. Stathacopoulos RA, Rosenbaum AL, Zanoni D. . Distance stereoacuity. Assessing control in intermittent exotropia. Ophthalmology. 1993; 100:495–500.
Article3. Adams WE, Leske DA, Hatt SR. . Improvement in distance stereoacuity following surgery for intermittent exotropia. J AAPOS. 2008; 12:141–4.
Article4. O'Connor AR, Birch EE, Anderson S, Draper H. FSOS Research Group. The functional significance of stereopsis. Invest Ophthalmol Vis Sci. 2010; 51:2019–23.5. Park DC. Quality assessment and analysis of stereoscopic 3D tele-vision pictures. J Institute of Signal Processing and Systems. 2010; 11:278–88.6. Fawcett SL. An evaluation of the agreement between con-tour-based circles and random dot-based near stereoacuity tests. J AAPOS. 2005; 9:572–8.
Article7. Romano PE, Romano JA, Puklin JE. Stereoacuity development in children with normal binocular single vision. Am J Ophthalmol. 1975; 79:966–71.
Article8. Takai Y, Sato M, Tan R, Hirai T. Development of stereoscopic acui-ty: longitudinal study using a computer-based random-dot stereo test. Jpn J Ophthalmol. 2005; 49:1–5.
Article9. Fox R, Patterson R, Francis EL. Stereoacuity in young children. Invest Ophthalmol Vis Sci. 1986; 27:598–600.10. Hong SW, Park SC. Development of distant stereoacuity in visu-ally normal children as measured by the Frisby-Davis distance stereotest. Br J Ophthalmol. 2008; 92:1186–9.
Article11. Chung YR, Yang H, Lew HM. . The assessment of stereoacuity in patients with strabismus. J Korean Ophthalmol Soc. 2008; 49:1309–16.
Article12. Cho YA, Cho SW, Roh GH. Evaluation of criteria of stereoacuity for Titmus, Randot & TNO stereotests. J Korean Ophthalmol Soc. 1999; 40:532–7.13. Park DJ, Kwak SH, Kim CM, Kim TG. Low-power discrete-event SoC for 3DTV active shutter glasses. J Institute of Electronics Engineers of Korea. 2011; 48:18–26.14. Yu CB, Fan DS, Wong VW. . Changing patterns of strabismus: a decade of experience in Hong Kong. Br J Ophthalmol. 2002; 86:854–6.
Article15. Rah SH, Jun HS, Kim SH. An epidemiologic survey of strabismus among school-children in Korea. J Korean Ophthalmol Soc. 1997; 38:2195–9.16. Yildirim C, Mutlu FM, Chen Y, Altinsoy HI. Assessment of central and peripheral fusion and near and distance stereoacuity in inter-mittent exotropic patients before and after strabismus surgery. Am J Ophthalmol. 1999; 128:222–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Comparison of 3D Endoscopic Sinonasal Surgery Between ‘Insect Eye’ 3D and ‘Twin Lens’ 3D Endoscopes
- Novel Three-Dimensional Image-Guided Surgery: Application of a Computed Tomography-Based Three-Dimensional Model Using a Tablet Device
- Clinical Applications of Three-Dimensional Printing in Cardiovascular Disease
- 3D-Printed Disease Models for Neurosurgical Planning, Simulation, and Training
- Three-dimensional image and virtual dissection program of the brain made of Korean cadaver