J Korean Ophthalmol Soc.
2013 May;54(5):798-802. 10.3341/jkos.2013.54.5.798.
A Case of Pott's Puffy Tumor from Recurrent Upper Eyelid Abscess
- Affiliations
-
- 1Department of Ophthalmology, Maryknoll Medical Center, Busan, Korea. eyerheu@hanafos.com
- KMID: 2217049
- DOI: http://doi.org/10.3341/jkos.2013.54.5.798
Abstract
- PURPOSE
To report a case of Pott's puffy tumor from a recurrent upper eyelid abscess.
CASE SUMMARY
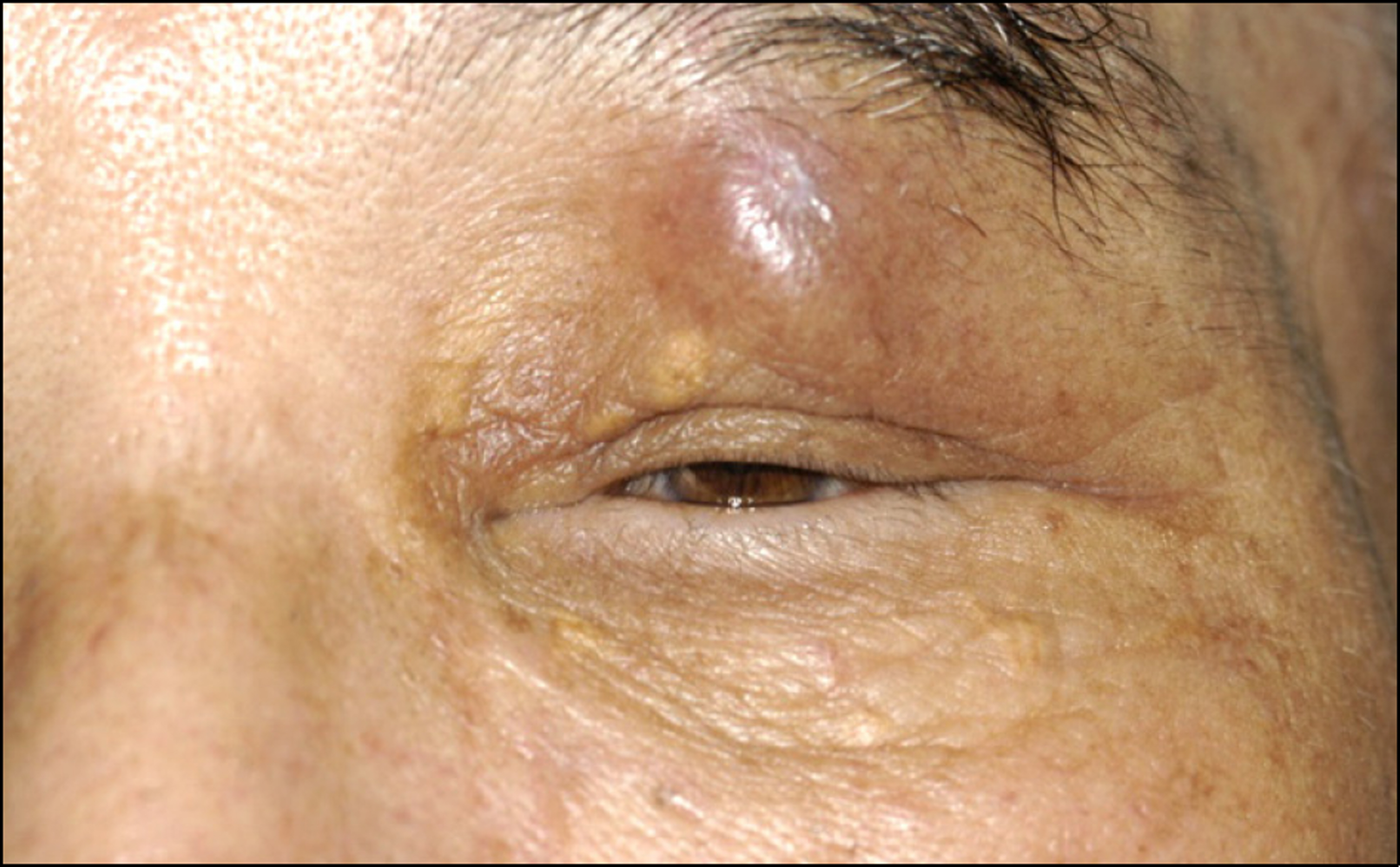
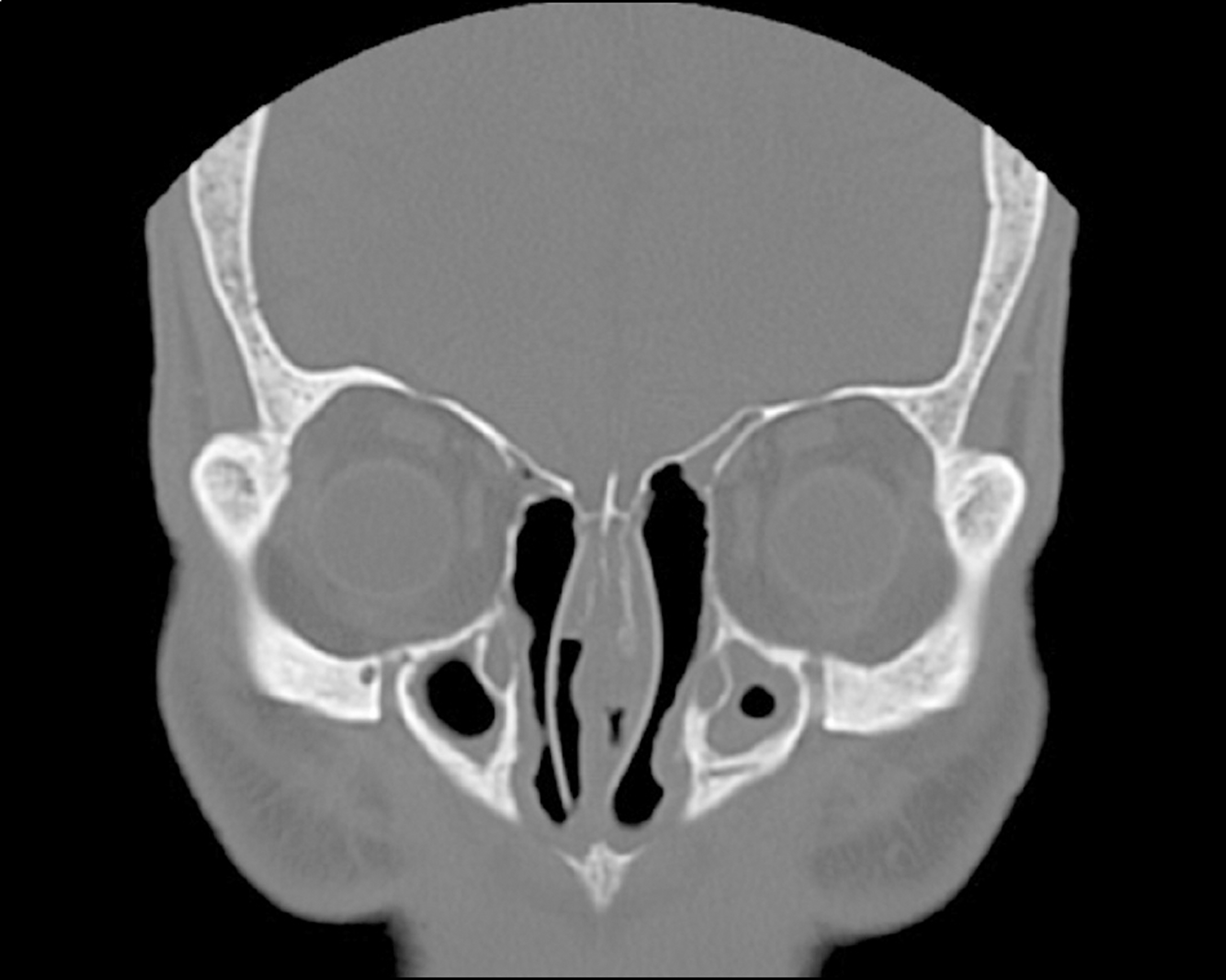
A 73-year-old male visited our clinic with recurrent upper eyelid abscess over the previous 3 months. The patient did not have any evidence of external injuries, systemic inflammations, or any other specific findings. The best corrected visual acuity was 0.9 in the right and 0.5 in the left eye with normal IOP. Enhanced CT revealed a focal low density mass (11.3 x 12.6 x 10 mm) with peripheral enhancement. An excisional biopsy was performed. Histopathologic examination revealed chronic inflammation and granulation tissue formation and the patient was diagnosed with Pott's puffy tumor. The patient experienced no discomfort after the excision biopsy. At the 14-month follow-up, there were no signs of recurrence.
CONCLUSIONS
Although rare, Pott' puffy tumor should be considered in the differential diagnosis of upper eyelid mass.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Tattersall R. Pott's puffy tumour. Lancet. 2002; 359:1060–3.
Article2. Kombogiorgas D, Solanki GA. The Pott puffy tumor revisited: neurosurgical implications of this unforgotten entity. Case report and review of the literature. J Neurosurg. 2006; 105:143–9.
Article3. Lee KW, Han KS. A case of orbital cellulitis subdural subdural abscess. J Korean Ophthalmol Soc. 1981; 22:475–8.4. Tsai BY, Lin KL, Lin TY, et al. Pott’s puffy tumor in children. Childs Nerv Syst. 2010; 26:53–60.
Article5. Moser R, Schweintzger G, Uggowitzer M, et al. Recurrent Pott’s puffy tumor - atypical presentation of a rare disorder. Wien Klin Wochenschr. 2009; 121:719–22.
Article6. Goldfarb A, Hocwald E, Gross M, Eliashar R. Frontal sinus cuta-neous fistula: a complication of Pott’s puffy tumor. Otolaryngol Head Neck Surg. 2004; 130:490–1.
Article7. Marshall AH, Jones NS. Osteomyelitis of the frontal bone secon-dary to frontal sinusitis. J Laryngol Otol. 2000; 114:944–6.
Article8. Lang EE, Curran AJ, Patil N, et al. Intracranial complications of acute frontal sinusitis. Clin Otolaryngol Allied Sci. 2001; 26:452–7.
Article9. Bağ datoğ lu C, Güleryüz A, Ersöz G, et al. A rare clinical entity: Pott’s puffy tumor. A case report. Pediatr Neurosurg. 2001; 34:156–8.10. Bambakidis NC, Cohen AR. Intracranial complications of frontal sinusitis in children: Pott's puffy tumor revisited. Pediatr Neurosurg. 2001; 35:82–9.
Article11. Lang EE, Curran AJ, Patil N, et al. Intracranial complications of acute frontal sinusitis. Clin Otolaryngol Allied Sci. 2001; 26:452–7.
Article12. Bannon PD, McCormack RF. Pott’s puffy tumor and epidural ab-scess arising from pansinusitis. J Emerg Med. 2011; 41:616–22.
Article13. Lamoreau KP, Fanciullo LM. Pott’s puffy tumour mimicking pre-septal cellulitis. Clin Exp Optom. 2008; 91:400–2.
Article14. Verbon A, Husni RN, Gordon SM, et al. Pott’s puffy tumor due to Haemophilus influenzae: case report and review. Clin Infect Dis. 1996; 23:1305–7.15. Im CS, Lee CY, Lew HM. A case of acute exophthalmos due to spreading of chronic frontal sinusitis. J Korean Ophthalmol Soc. 1996; 37:549–53.16. Ketenci I, Unlü Y, Tucer B, Vural A. The Pott's puffy tumor: a dan-gerous sign for intracranial complications. Eur Arch Otorhinolaryngol. 2011; 268:1755–63.
Article17. Younis RT, Anand VK, Davidson B. The role of computed tomog-raphy and magnetic resonance imaging in patients with sinusitis with complications. Laryngoscope. 2002; 112:224–9.
Article18. Goldberg AN, Oroszlan G, Anderson TD. Complications of frontal sinusitis and their management. Otolaryngol Clin North Am. 2001; 34:211–25.
Article19. Kuhn FA. Chronic frontal sinusitis: the endoscopic frontal recess approach. Oper Tech Otolaryngol Head Neck Surg. 1996; 7:222–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pott’s puffy tumor of the upper eyelid misdiagnosed as simple abscess: a case report and literature review
- A Case of External Approach Treatment of Pott's Puffy Tumor
- A case of Pott's puffy tumor with epidural abscess
- A Case of Pott's Puffy Tumor as a Complication of Contralateral Frontal Sinusitis
- Endoscopic Endonasal Treatment of a Pott's Puffy Tumor