J Korean Ophthalmol Soc.
2012 Jul;53(7):1057-1061. 10.3341/jkos.2012.53.7.1057.
Ocular Myasthenia Gravis in Conjunction with Thyroid-Associated Ophthalmopathy: A Case Report
- Affiliations
-
- 1Department of Ophthalmology, Soonchunhyang University College of Medicine, Cheonan, Korea. ophdrkim@schch.ac.kr
- KMID: 2215877
- DOI: http://doi.org/10.3341/jkos.2012.53.7.1057
Abstract
- PURPOSE
To report a case of ocular myasthenia gravis in conjunction with thyroid-associated ophthalmopathy in a patient who showed incomitant strabismus and blepharoptosis as well as to discuss the clinical features and tests that may help distinguish these 2 diseases.
CASE SUMMARY
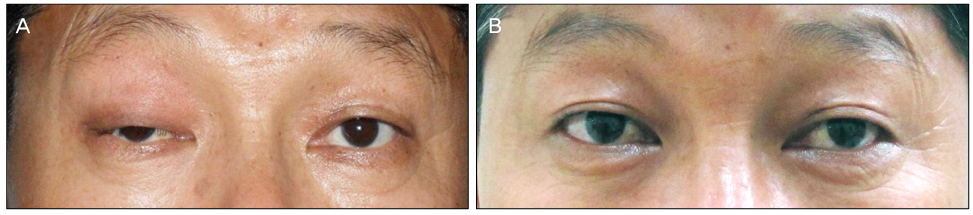
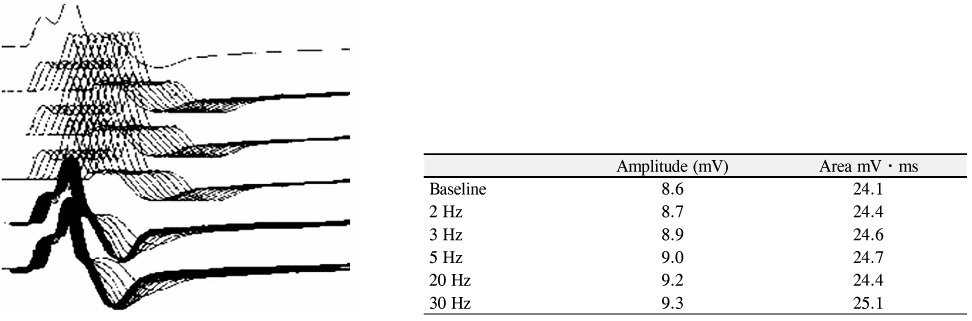
A 46-year-old man without any previous history of systemic and ophthalmic disease presented with binocular diplopia that occured a month earlier. The patient had no other systemic symptoms except a 7 kg weight loss within the last month. The patient was referred to the department of internal medicine and brain magnetic resonance imaging was performed to ascertain the cause of suspected left superior oblique muscle palsy. The patient was diagnosed with Graves' disease and underwent medical treatment. One month later, the patient presented with consistent diplopia and exophthalmos and showed a swelling of eyelid and ptosis in the right eye. Intravenous high-dose steroid therapy was administered to the patient. After the treatment, symptoms of diplopia and lid swelling were improved, however ptosis persisted. Ocular myasthenia gravis was suspected and various tests were conducted. Anti-acetylcholine receptor antibodies were detected in large amounts and ptosis was improved dramatically by an administration of an anticholinesterase agent. The patient was diagnosed with ocular myasthenia gravis in conjunction with thyroid-associated ophthalmopathy.
CONCLUSIONS
Ocular myasthenia gravis should be suspected in patients with thyroid-associated ophthalmopathy who have signs or symptoms of ptosis.
MeSH Terms
Figure
Reference
-
1. Coats DK, Paysse EA, Plager DA, Wallace DK. Early strabismus surgery for thyroid ophthalmopathy. Ophthalmology. 1999. 106:324–329.2. Weinberg DH, Rizzo JF 3rd, Hayes MT, et al. Ocular myasthenia gravis: predictive value of single-fiber electromyography. Muscle Nerve. 1999. 22:1222–1227.3. Padua L, Stalberg E, LoMonaco M, et al. SFEMG in ocular myasthenia gravis diagnosis. Clin Neurophysiol. 2000. 111:1203–1207.4. Peacey SR, Belchetz PE. Graves' disease: associated ocular myasthenia gravis and a thymic cyst. J R Soc Med. 1993. 86:297–298.5. Hong YH, Kwon SB, Kim BJ, et al. Prognosis of ocular myasthenia in Korea: a retrospective multicenter analysis of 202 patients. J Neurol Sci. 2008. 273:10–14.6. Vincent A, Newsom-Davis J. Acetylcholine receptor antibody as a diagnostic test for myasthenia gravis: results in 153 validated cases and 2967 diagnostic assays. J Neurol Neurosurg Psychiatry. 1985. 48:1246–1252.7. Marinó M, Ricciardi R, Pinchera A, et al. Mild clinical expression of myasthenia gravis associated with autoimmune thyroid disease. J Clin Endocrinol Metab. 1997. 82:438–443.8. Oosterhuis HJ. The ocular signs and symptoms of myasthenia gravis. Doc Ophthalmol. 1982. 52:363–378.9. Evoli A, Tonali P, Bartoccioni E, Lo Monaco M. Ocular myasthenia: diagnostic and therapeutic problems. Acta Neurol Scand. 1988. 77:31–35.10. Puvanendran K, Cheah JS, Naganathan N, et al. Neuromuscular transmission in thyrotoxicosis. J Neurol Sci. 1979. 43:47–57.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Graves' disease associated with ocular myasthenia gravis
- The Clinical Characteristics of Hyperthyroidism Combined with Ocular Myasthenia Gravis: Report of Six cases
- The Clinical Features of Ocular Myasthenia Gravis in Thyroid-Associated Ophthalmopathy
- A Case of Severe Ocular Myasthenia Gravis that Developed Total External Ophthalmoplegia
- Fecal Incontinence as a Symptom of Myasthenia Gravis