J Korean Ophthalmol Soc.
2012 Jan;53(1):175-179. 10.3341/jkos.2012.53.1.175.
Surgical Removal of Sub-Tenon Triamcinolone Acetonide in Cases of Increased Intraocular Pressure after Sub-Tenon Injection
- Affiliations
-
- 1Department of Ophthalmology, School of Medicine, Kyungpook National University, Daegu, Korea. jps11@hanmail.net
- KMID: 2215262
- DOI: http://doi.org/10.3341/jkos.2012.53.1.175
Abstract
- PURPOSE
To report cases of the surgical removal of sub-Tenon triamcinolone acetonide to control increased intraocular pressure after sub-Tenon triamcinolone acetonide injection.
CASE SUMMARY
Three patients had no response to maximal medical treatment to control suddenly increased intraocular pressure after sub-Tenon triamcinolone acetonide (40 mg) injection to treat diabetic macular edema. The anterior chamber angle was open in all patients, and there was no neovascularization in the iris or anterior chamber angle. Slit lamp biomicroscopy showed deposition of triamcinolone acetonide in the inferior sub-Tenon area. Intraocular pressure was decreased within the normal range without any medication after removal of triamcinolone acetonide precipitates.
CONCLUSIONS
Surgical removal of sub-Tenon triamcinolone acetonide can be as a primary treatment option in cases of increased intraocular pressure which shows no response to maximal medical treatment after sub-Tenon triamcinolone acetonide injection.
MeSH Terms
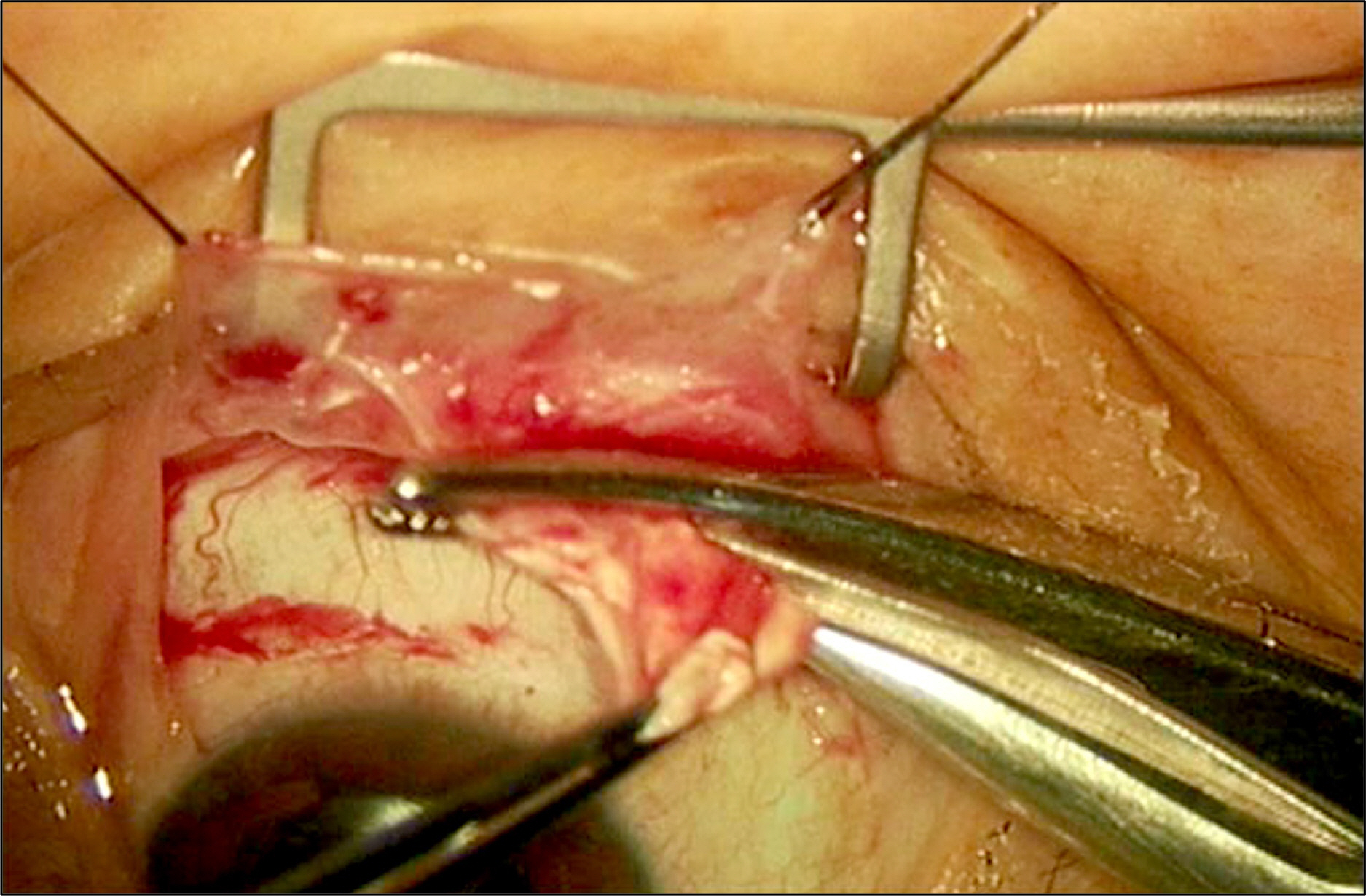
Figure
Reference
-
References
1. Choi YJ, Oh IK, Oh JR, Huh K. Intravitreal versus posterior sub-tenon injection of triamcinolone acetonide for diabetic macular edema. Korean J Ophthalmol. 2006; 20:205–9.
Article2. Ozdek S, Deren YT, Gurelik G, Hasanreisoglu B. Posterior sub-tenon triamcinolone, intravitreal triamcinolone and grid laser photocoagulation for the treatment of macular edema in branch retinal vein occlusion. Ophthalmic Res. 2008; 40:26–31.
Article3. Kim YJ, Kang SW, Ahn BH, Ham DI. The results of posterior sub-tenon steroid injection in uveitis patients. J Korean Ophthalmol Soc. 2003; 44:66–72.4. Jea SY, Byon IS, Oum BS. Triamcinolone-induced intraocular pressure elevation: intravitreal injection for macular edema and posterior subtenon injection for uveitis. Korean J Ophthalmol. 2006; 20:99–103.
Article5. Giles CL. Bulbar perforation during periocular injection of corticosteroids. Am J Ophthalmol. 1974; 77:438–41.
Article6. Ellis PP. Occlusion of the central retinal artery after retrobulbar corticosteroid injection. Am J Ophthalmol. 1978; 85:352–6.
Article7. Nozik RA. Orbital rim fat atrophy after repository periocular corticosteroid injection. Am J Ophthalmol. 1976; 82:928–30.
Article8. Kusaka S, Ikuno Y, Ohguro N, et al. Orbital infection following posterior subtenon triamcinolone injection. Acta Ophthalmol Scand. 2007; 85:692–3.
Article9. Oh IK, Baek S, Huh K, Oh J. Periocular abscess caused by Pseudallescheria boydii after a posterior subtenon injection of triamcinolone acetonide. Graefes Arch Clin Exp Ophthalmol. 2007; 245:164–6.
Article10. Kuo HK, Lai IC, Fang PC, Teng MC. Ocular complications after a sub-tenon injection of triamcinolone acetonide for uveitis. Chang Gung Med J. 2005; 28:85–9.11. Lafranco Dafflon ML, Tran VT, Guex-Crosier Y, Herbort CP. Posterior sub-Tenon's steroid injections for the treatment of posterior ocular inflammation: indications, efficacy and side effects. Graefe's Arch Clin Exp Ophthalmol. 1999; 237:289–95.
Article12. Bui Quoc E, Bodaghi B, Adam R, et al. Intraocular pressure elevation after subtenon injection of triamcinolone acetonide during uveitis. J Fr Ophtalmol. 2002; 25:1048–56.13. Mueller AJ, Jian G, Banker AS, et al. The effect of deep posterior subtenon injection of corticosteroids on intraocular pressure. Am J Ophthalmol. 1998; 125:158–63.
Article14. Helm CJ, Holland GN. The effect of posterior subtenon injection of triamcinolone acetonide in patients with intermediate uveitis. Am J Ophthalmol. 1995; 120:55–64.15. Yamamoto Y, Komatsu T, Koura Y, et al. Intraocular pressure elevation after intravitreal or posterior sub-Tenon triamcinolone acetonide injection. Can J Ophthalmol. 2008; 43:42–7.
Article16. Iwao K, Inatani M, Kawaji T, et al. Frequency and risk factors for intraocular pressure elevation after posterior sub-Tenon capsule triamcinolone acetonide injection. J Glaucoma. 2007; 16:251–6.
Article17. Hirooka K, Shiraga F, Tanaka S, et al. Risk factors for elevated intraocular pressure after trans-tenon retrobulbar injections of triamcinolone. Jpn J Ophthalmol. 2006; 50:235–8.
Article18. Shimura M, Yasuda K, Nakazawa T, et al. Drug reflux during posterior subtenon infusion of triamcinolone acetonide in diffuse diabetic macular edema not only brings insufficient reduction but also causes elevation of intraocular pressure. Graefes Arch Clin Exp Ophthalmol. 2009; 247:907–12.
Article19. Inatani M, Iwao K, Kawaji T, et al. Intraocular pressure elevation after injection of triamcinolone acetonide: a multicenter retro-spective case-control study. Am J Ophthalmol. 2008; 145:676–81.
Article20. Levin DS, Han DP, Dev S, et al. Subtenon's depot corticosteroid injections in patients with a history of corticosteroid-induced intraocular pressure elevation. Am J Ophthalmol. 2002; 133:196–202.
Article21. Kim WJ, Park YH. The intraocular pressure rise secondary to sub-tenon's injection of triamcinolone after intravitreal injection. J Korean Ophthalmol Soc. 2008; 49:91–7.
Article22. Wordinger RJ, Clark AF. Effects of glucocorticoids on the trabecular meshwork: towards a better understanding of glaucoma. Prog Retin Eye Res. 1999; 18:629–67.
Article23. Hernandez MR, Wenk EJ, Weinstein BI, et al. Glucocorticoid target cells in human outflow pathway: autopsy and surgical specimens. Invest Ophthalmol Vis Sci. 1983; 24:1612–6.24. Tawara A, Tou N, Kubota T, et al. Immunohistochemical evaluation of the extracellular matrix in trabecular meshwork in steroid-induced glaucoma. Graefes Arch Clin Exp Ophthalmol. 2008; 246:1021–8.
Article25. Clark AF, Wordinger RJ. The role of steroids in outflow resistance. Exp Eye Res. 2009; 88:752–9.
Article26. Hirano Y, Ito T, Nozaki M, et al. Intraocular pressure elevation following triamcinolone acetonide administration as related to administration routes. Jpn J Ophthalmol. 2009; 53:519–22.
Article27. Herschler J. Increased intraocular pressure induced by repository corticosteroids. Am J Ophthalmol. 1976; 82:90–3.
Article28. Okka M, Bozkurt B, Kerimoglu H, et al. Control of steroid-induced glaucoma with surgical excision of sub-Tenon triamcinolone acetonide deposits: a clinical and biochemical approach. Can J Ophthalmol. 2010; 45:621–6.
Article29. Yuki K, Inoue M, Shiba D, et al. Selective laser trabeculoplasty for elevated intraocular pressure following subtenon injection of triamcinolone acetonide. Clin Ophthalmol. 2010; 26:247–9.30. Mills DW, Siebert LF, Climenhaga DB. Depot triamcinolone-induced glaucoma. Can J Ophthalmol. 1986; 21:150–2.31. Aydin A, Akin T, Bilge AH. Management of persistent glaucoma secondary to depot methylprednisolone. Ophthalmic Surg Lasers Imaging. 2007; 38:399–401.
Article32. Akduman L, Kolker AE, Black DL, et al. Treatment of persistent glaucoma secondary to periocular corticosteroids. Am J Ophthalmol. 1996; 122:275–7.
Article33. Kalina PH, Erie JC, Rosenbaum L. Biochemical quantification of triamcinolone in subconjunctival depots. Arch Ophthalmol. 1995; 113:867–9.
Article34. Kalina RE. Increased intraocular pressure following subconjunctival corticosteroid administration. Arch Ophthalmol. 1969; 81:788–90.
Article35. Nakamura M, Kanamori A, Negi A. Diabetes mellitus as a risk factor for glaucomatous optic neuropathy. Ophthalmologica. 2005; 219:1–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Combined Effect of Subtenon Triamcinolone Injection and Panretinal Photocoagulation on Diabetic Retinopathy
- Posterior Sub-Tenon Triamcinolone Acetonide Injection for Recurrent Diabetic Macular Edema after Repeated Intravitreal Bevacizumab Injections
- Effect of Posterior Subtenon Triamcinolone Injection during Vitrectomy for Idiopathic Epiretinal Membrane
- Effect of Triamcinolone Acetonide on the Survival and Nitric Oxide Production in Cultured Human Tenon's Capsule Fibroblasts
- The Intraocular Pressure Rise Secondary to Subtenon's Injection of Triamcinolone After Intravitreal Injection