J Korean Ophthalmol Soc.
2011 Oct;52(10):1238-1243. 10.3341/jkos.2011.52.10.1238.
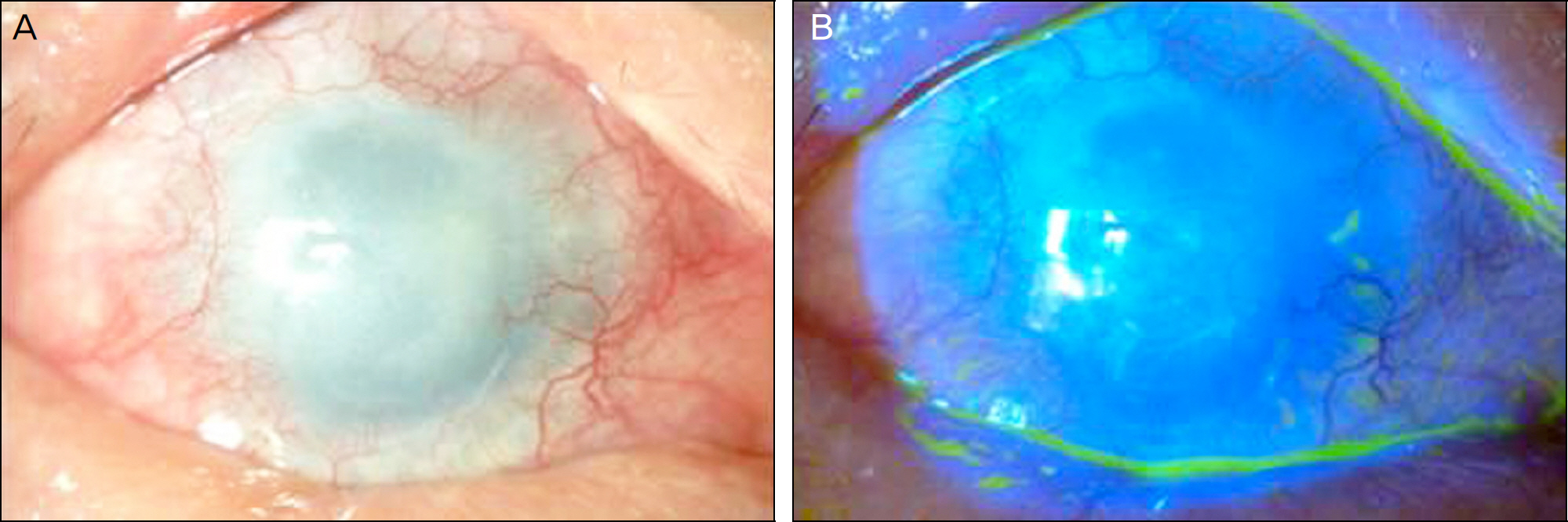
Two Cases of Whole Corneo-Limbal Transplantation
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Laboratory of Corneal Regenerative Medicine and Ocular Immunology, Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea. kmk9@
- KMID: 2215009
- DOI: http://doi.org/10.3341/jkos.2011.52.10.1238
Abstract
- PURPOSE
To report the clinical outcomes of total corneolimbal transplantation in two cases.
CASE SUMMARY
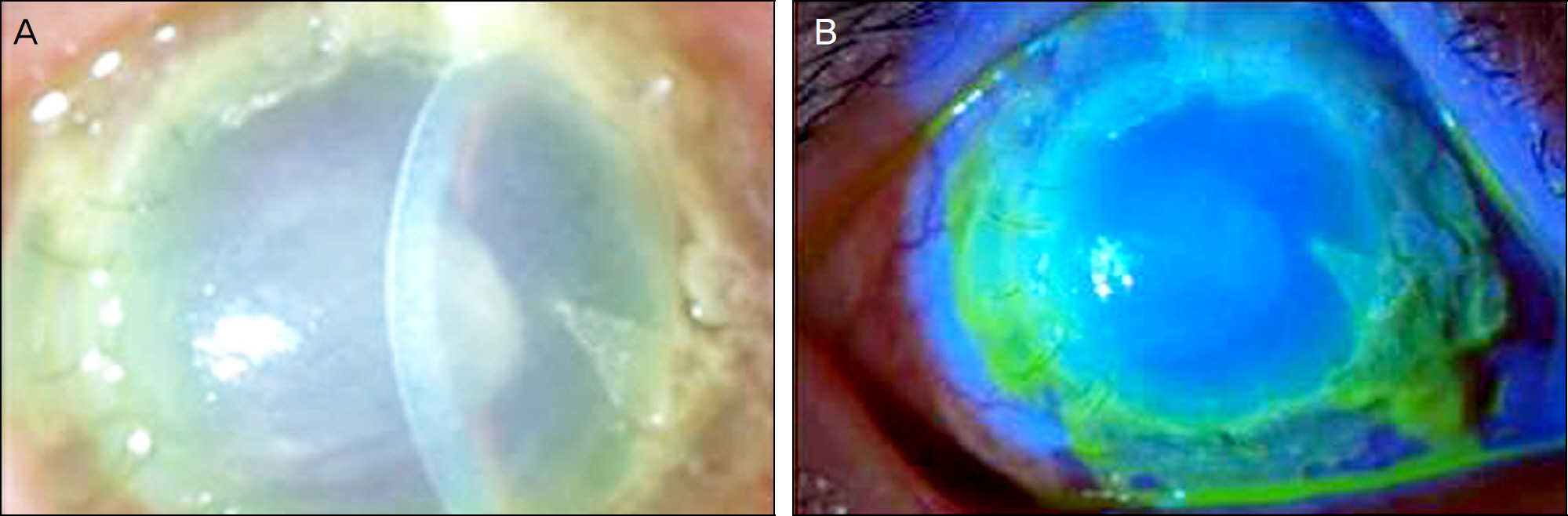
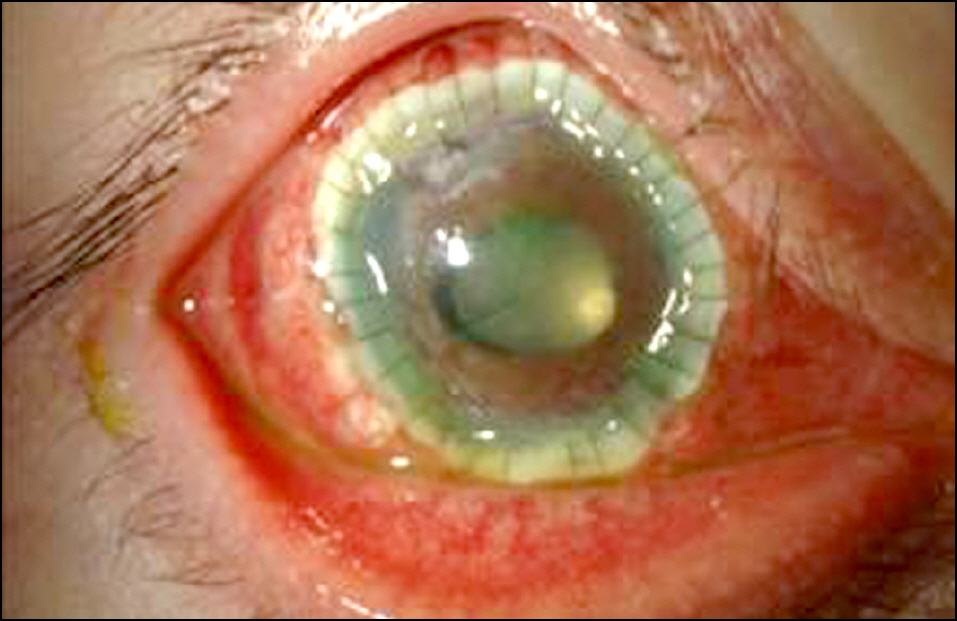
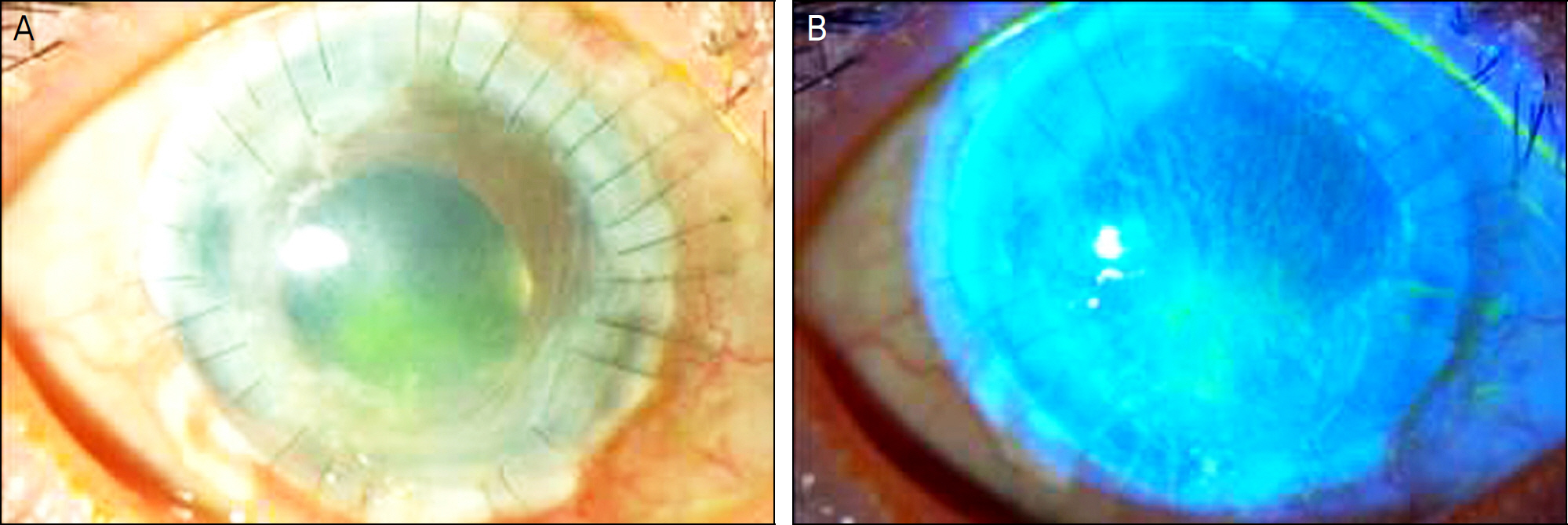
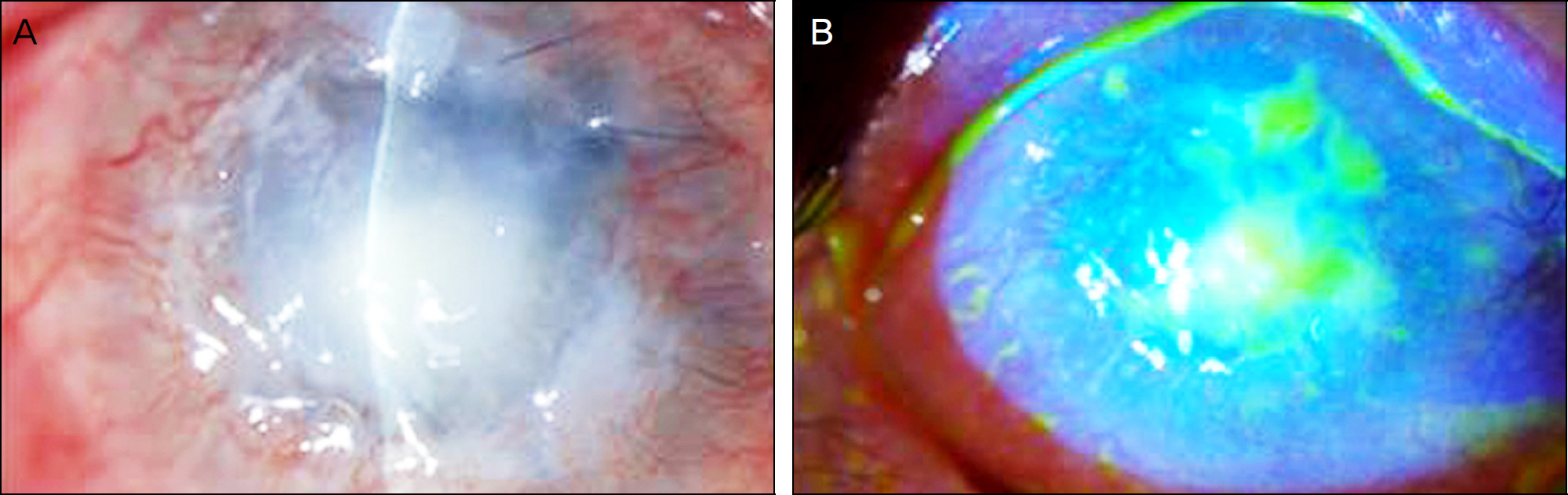
One patient, who previously underwent three rounds of penetrating keratoplasty and limbal transplantation for uncontrollable peripheral and central corneal melting, received total corneolimbal transplantation. The other patient who underwent penetrating keratoplasty with limbal transplanation for a chemical burn and who did not experience corneal perforation also received total corneolimbal transplantation. During the average 19 months of follow-up, cyclophotocoagulation was performed to control high intraocular pressure in both patients. Both eyes were tectonically maintained without further corneal destruction despite poor visual acuity and rejection.
CONCLUSIONS
Total corneolimbal transplantation may be an effective tectonic procedure for corneal melting. This procedure can be considered as another option for patients with corneal melting after failed limbal and corneal transplantation.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A Case of Autologous Tragal Perichondrium Graft in a Patient with Mooren's Ulcer
Dong Ik Lee, Kyoung Woo Kim, Jae Chan Kim
J Korean Ophthalmol Soc. 2014;55(3):437-442. doi: 10.3341/jkos.2014.55.3.437.
Reference
-
References
1. Castroviejo R. Total penetrating keratoplasty; a preliminary report. Am J Ophthalmol. 1951; 34:1697–706.2. Burke JW. Total keratoplasty. Trans Am Ophthalmol Soc. 1920; 18:440–7.3. Tsubota K, Satake Y, Kaido M, et al. Treatment of severe ocular-surface disorders with corneal epithelial stem-cell transplantation. N Engl J Med. 1999; 340:1697–703.
Article4. Tsai RJ, Tseng SC. Human allograft limbal transplantation for corneal surface reconstruction. Cornea. 1994; 13:389–400.
Article5. Kenyon KR, Tseng SC. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989; 96:709–22.
Article6. Lee S. Ophthalmic Plastic and Reconstructive Surgery. 1st ed.Seoul: Korean Society of Ophthalmic Plastic and Reconstructive Surgery;2004. p. 4.7. Kuckelkorn R, Redbrake C, Schrage NF, Reim M. Keratoplasty with 11–12 mm diameter for management of severely chem-ical-burned eyes. Ophthalmologe. 1993; 90:683–7.8. Vajpayee RB, Thomas S, Sharma N, et al. Large-diameter lamellar keratoplasty in severe ocular alkali burns: A technique of stem cell transplantation. Ophthalmology. 2000; 107:1765–8.9. Kwitko S, Marinho D, Barcaro S, et al. Allograft conjunctival transplantation for bilateral ocular surface disorders. Ophthalmology. 1995; 102:1020–5.
Article10. Jager M. Corneal Langerhans cells and ocular immunology. Regional Immunol. 1992; 4:186–95.11. Skeens HM, Holland EJ. Large-diameter penetrating keratoplasty: indications and outcomes. Cornea. 2010; 29:296–301.
Article12. Cobo M, Ortiz JR, Safran SG. Sclerokeratoplasty with maintenance of the angle. Am J Ophthalmol. 1992; 113:533–7.
Article13. Panda A, Sharma N, Angra SK, Singh R. Therapeutic sclerokeratoplasty versus therapeutic penetrating keratoplasty in refractory corneal ulcers. Aust N Z J Ophthalmol. 1999; 27:15–9.
Article14. Jonas JB, Rank RM, Budde WM. Tectonic sclerokeratoplasty and tectonic penetrating keratoplasty as treatment for perforated or pre-descemetal corneal ulcers. Am J Ophthalmol. 2001; 132:14–8.
Article15. Zerve BL, Belin MW, Ciolino JB. Boston Type 1 Keratoprosthesis study group. Results from the multicenter Boston type 1 keratoprosthesis study. Ophthalmology. 2006; 113:1779.
Article16. Greiner MA, Li J-Y, Mannis MJ. Longer term vision outcomes and complications with the Boston type 1 keratoprosthesis at the University of California, Davis. Ophthalmology. 2011; 118:1543–50.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 2 Cases of Limbal Autograft Transplantation after Chemical/Thermal Corneal Burns
- Early Effect of Autologous Limbal Transplantation Immediately following Total Limbal Injury in Rabbits
- Changes in Corneal Thickness in Congenital Glaucoma, Using Anterior Segment Optical Coherence Tomography
- Transplantation of in vivo Cultivated Limbal Corneal Epithelial Cells with Total Limbal Stem Cell Deficiency
- Combined Surgery of the Penetrating Keratoplasty and the Limbal Cell Transplantation