J Korean Ophthalmol Soc.
2011 Aug;52(8):984-989. 10.3341/jkos.2011.52.8.984.
Combined Mitomycin-C Assisted Photorefractive Keratectomy in the Treatment of Epithelial Ingrowth after LASIK
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, The Catholic University College of Medicine, Seoul, Korea. mskim@catholic.ac.kr
- KMID: 2214778
- DOI: http://doi.org/10.3341/jkos.2011.52.8.984
Abstract
- PURPOSE
To report 2 cases of thick, late-onset and long-standing epithelial ingrowth after laser-assisted in situ keratomilusis (LASIK) using mitomycin C-assisted photorefractive keratectomy and flap suturing.
CASE SUMMARY
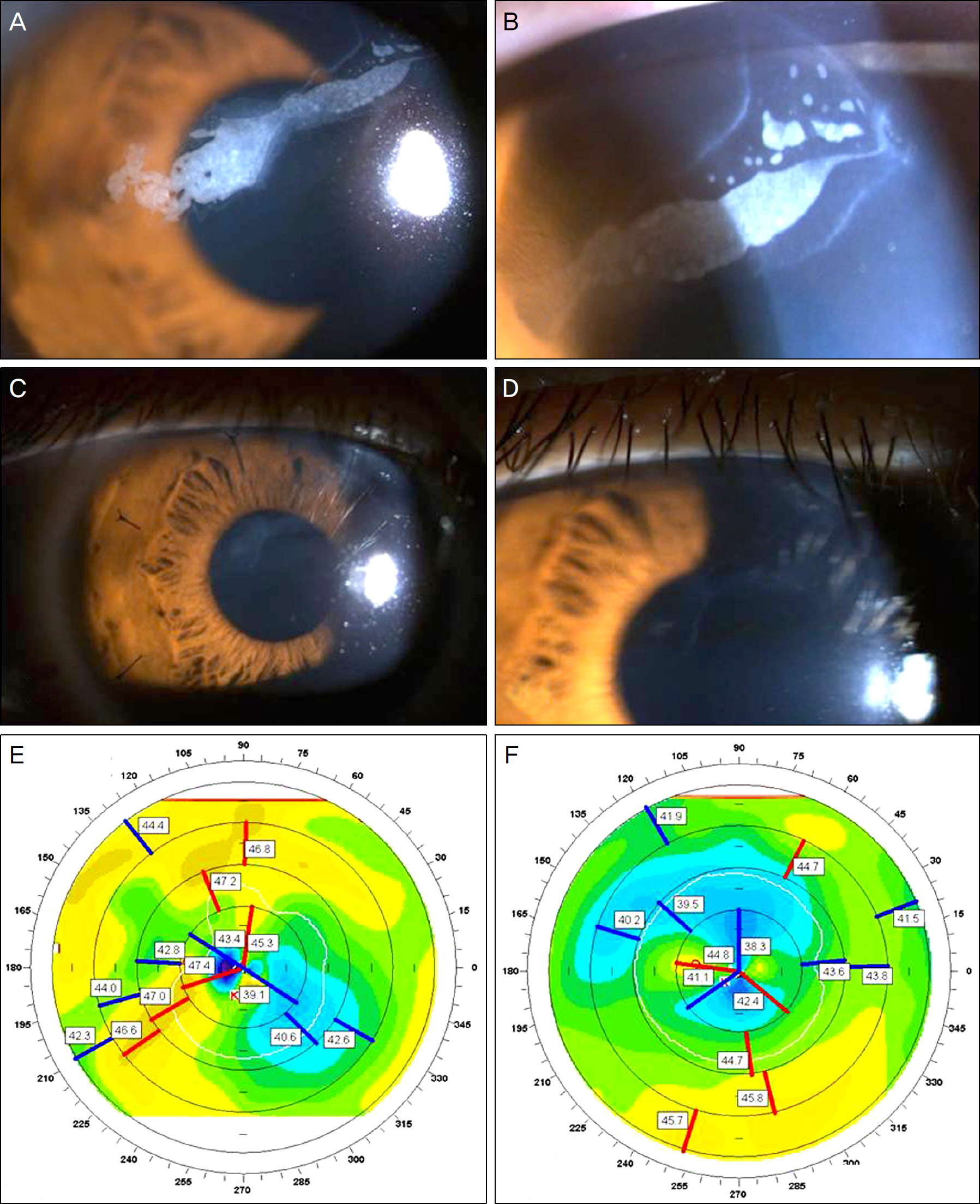
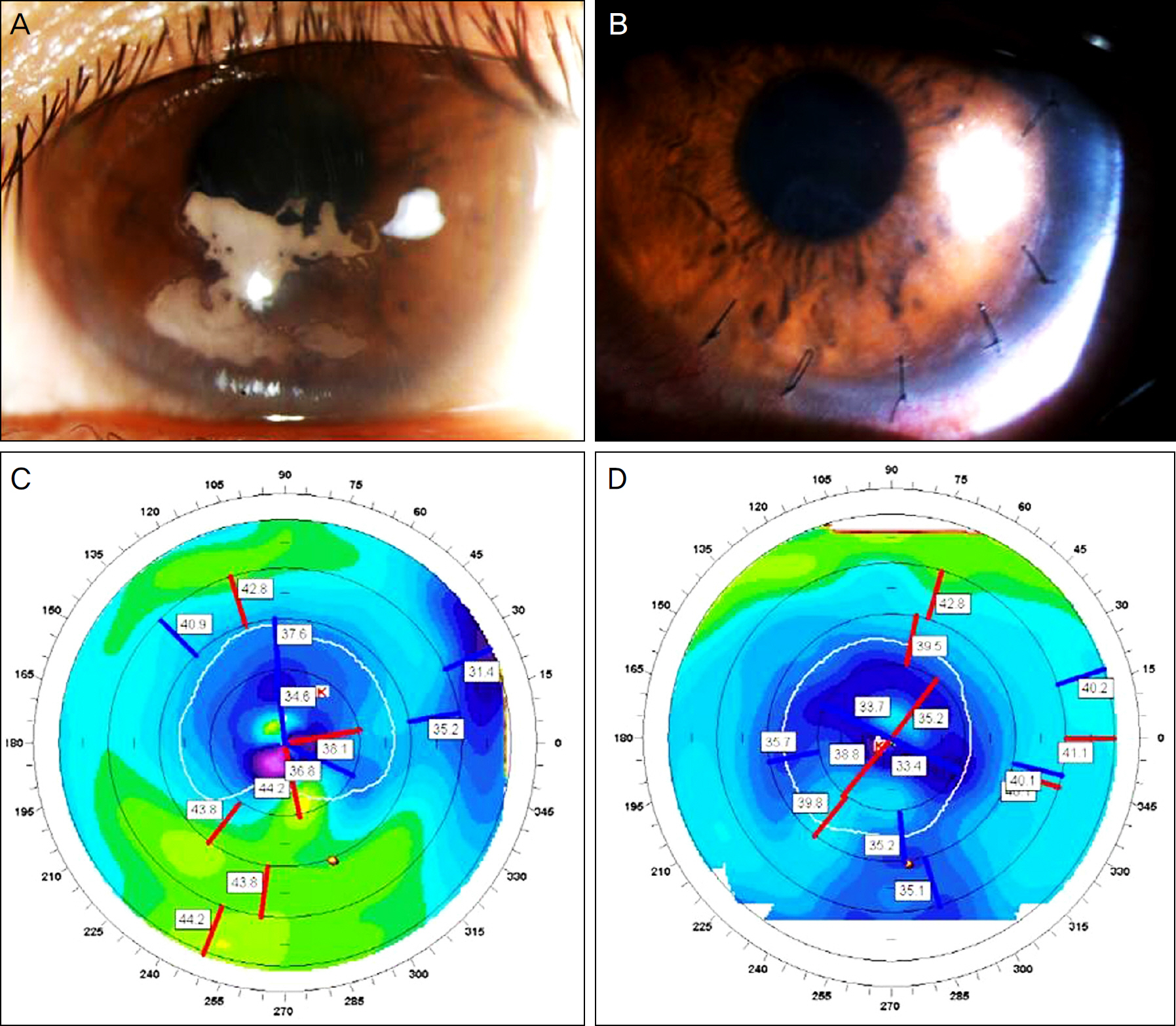
The first case involved a 29-year-old woman who had LASIK in both eyes in 2002. She was diagnosed with epithelial ingrowth OD after blunt ocular trauma in 2007. The second case involved a 30-year-old man who had LASIK in both eyes in 1999 followed by enhancements in 2004. Slit lamp examination showed dense epithelial ingrowth OS in a geographic pattern. Two eyes of the 2 patients with epithelial ingrowth had flap lifting followed by debridement of interface epithelial cells, photorefractive keratectomy, interface application of mitomycin C, and the placement of interrupted 10-0 nylon sutures. Two eyes regained better uncorrected visual acuity and showed reduced corneal astigmatism postoperatively. There was no evidence of residual or recurrent ingrowth throughout the follow-up period (case 1: 11 months, case 2: 1 month).
CONCLUSIONS
Combined mitomycin C-assisted photorefractive keratectomy and flap suturing can be an effective and safe method for treating and preventing the recurrence of thick, late-onset and long-standing epithelial ingrowth involving the visual axis.
MeSH Terms
Figure
Reference
-
References
1. Rapuano CJ. Management of epithelial ingrowth after laser in situ keratomileusis on a tertiary care cornea service. Cornea. 2010; 29:307–13.
Article2. Domniz Y, Comaish IF, Lawless MA, et al. Epithelial ingrowth: causes, prevention, and treatment in 5 cases. J Cataract Refract Surg. 2001; 27:1803–11.
Article3. Naoumidi I, Papadaki T, Zacharopoulos I, et al. Epithelial ingrowth after laser in situ keratomileusis: a histopathologic study in human corneas. Arch Ophthalmol. 2003; 121:950–5.4. Anderson NJ, Hardten DR. Fibrin glue for the prevention of epithelial ingrowth after laser in situ keratomileusis. J Cataract Refract Surg. 2003; 29:1425–9.
Article5. Spanggord HM, Epstein RJ, Lane HA, et al. Flap suturing with proparacaine for recurrent epithelial ingrowth following laser in situ keratomileusis surgery. J Cataract Refract Surg. 2005; 31:916–21.
Article6. Fagerholm P, Molander N, Podskochy A, Sundelin S. Epithelial ingrowth after LASIK treatment with scraping and phototherapeutic keratectomy. Acta Ophthalmol Scand. 2004; 82:707–13.
Article7. Taneri S, Koch JM, Melki SA, Azar DT. Mitomycin-C assisted photorefractive keratectomy in the treatment of buttonholed laser in situ keratomileusis flaps associated with epithelial ingrowth. J Cataract Refract Surg. 2005; 31:2026–30.
Article8. Ambrósio R Jr, Wilson SE. Complications of laser in situ keratomileusis: etiology, prevention, and treatment. J Refract Surg. 2001; 17:350–79.
Article9. Leung AT, Rao SK, Cheng AC, et al. Pathogenesis and management of laser in situ keratomileusis flap buttonhole. J Cataract Refract Surg. 2000; 26:358–62.
Article10. Asano-Kato N, Toda I, Hori-Komai Y, et al. Epithelial ingrowth after laser in situ keratomileusis: clinical features and possible mechanisms. Am J Ophthalmol. 2002; 134:801–7.
Article11. Kamburoğ lu G, Ertan A. Epithelial ingrowth after femtosecond laser-assisted in situ keratomileusis. Cornea. 2008; 27:1122–5.12. Wang MY, Maloney RK. Epithelial ingrowth after laser in situ keratomileusis. Am J Am J Ophthalmol. 2000; 129:746–51.
Article13. Kim SW, Byun YJ, Kim EK, Kim TI. Treatment of epithelial ingrowth after laser in situ keratomileusis using amniotic membrane patch. J Korean Ophthalmol Soc. 2007; 48:230–7.14. Zhao LQ, Wei RL, Ma XY, Zhu H. Effect of intraoperative mitomycin-C on healthy corneal endothelium after laser-assisted subepithelial keratectomy. J Cataract Refract Surg. 2008; 34:1715–9.
Article15. Kim ES, Jin KH. Evaluation of the prophylactic use of mitomycin to inhibit haze formation after LASEK. J Korean Ophthalmol Soc. 2007; 48:623–9.16. Verweij J, Pinedo HM. Mitomycin C: mechanism of action, usefulness and limitations. Anticancer Drugs. 1990; 1:5–13.17. Xu H, Liu S, Xia X, et al. Mitomycin C reduces haze formation in rabbits after excimer laser photorefractive keratectomy. J Refract Surg. 2001; 17:342–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Clinical Results between Transepithelial Photorefractive Keratectomy and Brush Photorefractive Keratectomy
- The Analysis of Epithelial Ingrowth after LASIK Using a Femtosecond Laser
- Early Postoperative Pain and Visual Outcomes Following Epipolis-Laser In Situ Keratomileusis and Photorefractive Keratectomy
- The Effect of Anti-glaucoma Eyedrops and 0.1% Fluorometholone on Myopic Regression after LASIK or LASEK
- Effect of Mitomycin C to Inhibit Corneal Haze Formation after Photorefractive Keratectomy for High Myopia