J Korean Ophthalmol Soc.
2011 Aug;52(8):952-958. 10.3341/jkos.2011.52.8.952.
Comparison of the Natural Course and Intravitreal Triamcinolone Treatment for Macular Edema with Branch Retinal Vein Occlusion
- Affiliations
-
- 1Department of Ophthalmology, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea. piw@korea.com
- KMID: 2214772
- DOI: http://doi.org/10.3341/jkos.2011.52.8.952
Abstract
- PURPOSE
To evaluate the natural course of eyes with decreased visual acuity associated with macular edema secondary to branch retinal vein occlusion (BRVO) and to compare the visual outcome and macular thickness with those of eyes treated with intravitreal triamcinolone acetonide injection (IVTA).
METHODS
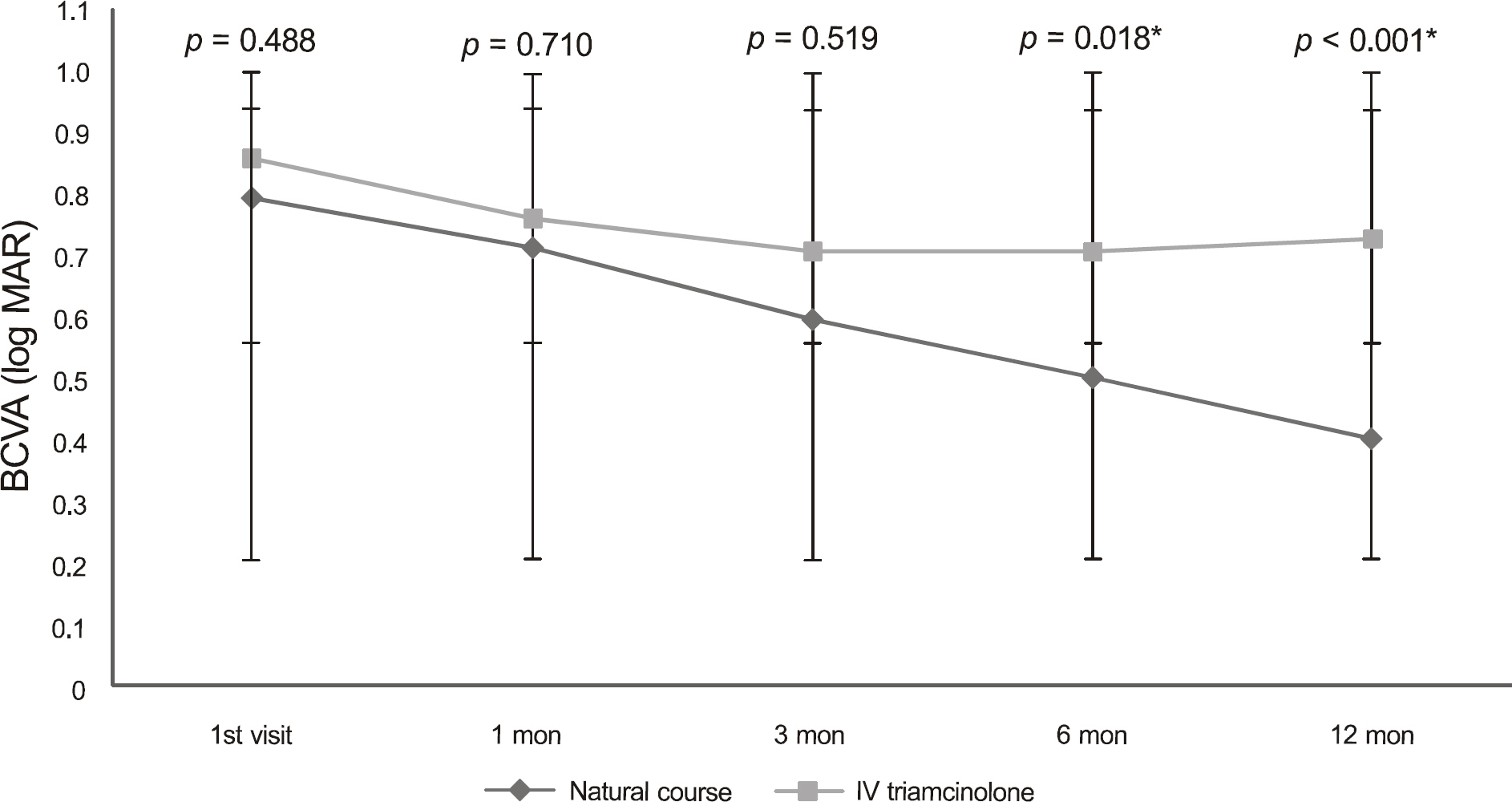
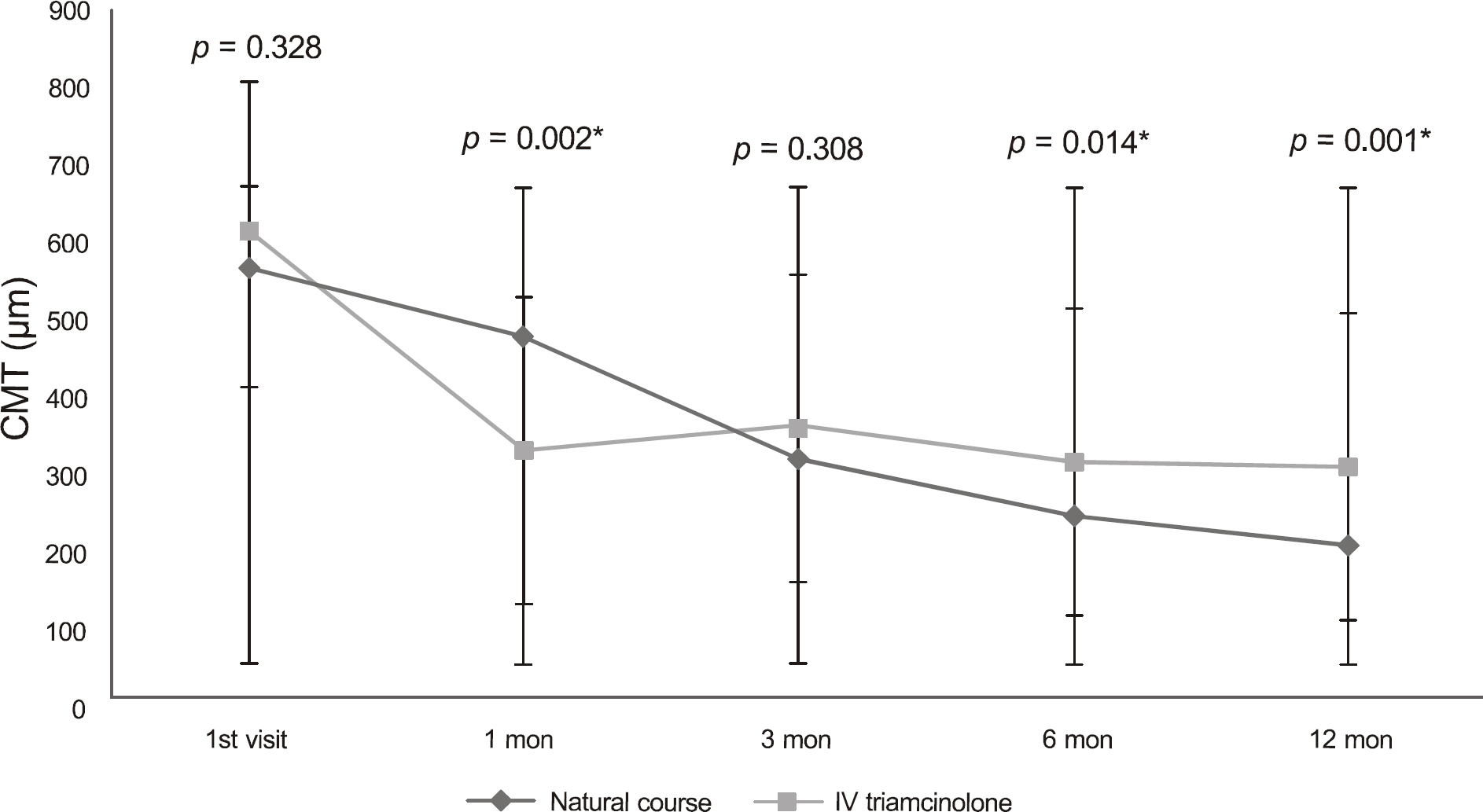
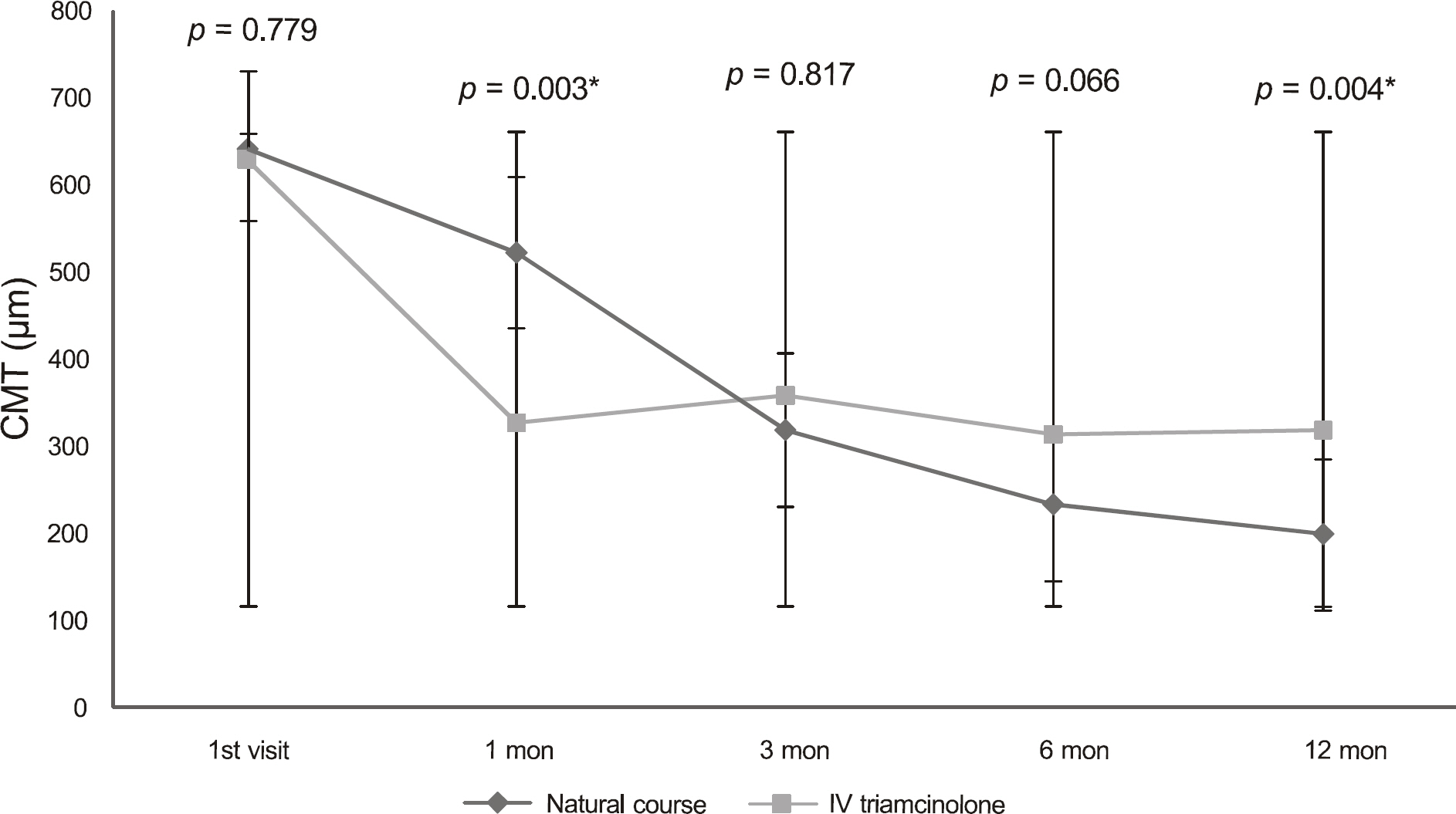
We reviewed the medical records of patients with macular edema secondary to BRVO who were followed-up for 12 months. We evaluated the best corrected visual acuity (BCVA) and macular thickness of the patients who had no treatment for macular edema (natural course group) and compared them with those of patients who had been treated with IVTA (treatment group).
RESULTS
A total of 29 eyes (29 patients) in the natural course group and 27 eyes (27 patients) in the treatment group were enrolled. The BCVA of the natural course group improved in a slow but steady manner and showed a statistically significant difference at 12 months. The treatment group did not show any improvement in BCVA throughout the follow-up period. Therefore, BCVA significantly improved in the natural course group after six months compared to that in the treatment group. Macular thickness showed a statistically significant reduction in three months in the natural course group and in one month in the treatment group.
CONCLUSIONS
Although IVTA was effective in reducing macular edema in branch retinal vein occlusion at one month after administration, the natural course group had a superior outcome and more improved macular thickness after six months.
MeSH Terms
Figure
Reference
-
References
1. Ennema MC, Zeeman WP. Venous occlusion of the retina. Ophthalmologica. 1953; 126:329–47.2. Mitchell P, Smith W, Chang A. Prevalence and associations of retinal vein occlusion in Australia. The Blue Mountains Eye Study. Arch Ophthalmol. 1996; 114:1243–7.3. Klein R, Moss SE, Meuer SM, Klein BE. The 15-year cumulative incidence of retinal vein occlusion: the Beaver Dam Eye Study. Arch Ophthalmol. 2008; 126:513–8.4. Gutman FA, Zegarra H. The natural course of temporal retinal branch vein occlusion. Trans Am Acad Ophthalmol Otolaryngol. 1974; 78:178–92.5. Hayreh SS, Rojas P, Podhajsky P, et al. Ocular neovascularization with retinal vascular occlusion-III. Incidence of ocular neovascularization with retinal vein occlusion. Ophthalmology. 1983; 90:488–506.6. Magargal LE, Kimmel AS, Sanborn GE, Annesley WH Jr. Temporal branch retinal vein obstruction: a review. Ophthalmic Surg. 1986; 17:240–6.
Article7. Gutman FA. Macular edema in branch retinal vein occlusion: prognosis and management. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1977; 83:488–95.8. Roseman RL, Olk RJ. Krypton red laser photocoagulation for branch retinal vein occlusion. Ophthalmology. 1987; 94:1120–5.
Article9. Argon laser photocoagulation for macular edema in branch vein occlusion. The Branch Vein Occlusion Study Group. Am J Ophthalmol. 1984; 98:271–82.10. Patel PJ, Zaheer I, Karia N. Intravitreal triamcinolone acetonide for macular oedema owing to retinal vein occlusion. Eye. 2008; 22:60–4.
Article11. Russo V, Barone A, Conte E, et al. Bevacizumab compared with macular laser grid photocoagulation for cystoid macular edema in branch retinal vein occlusion. Retina. 2009; 29:511–5.
Article12. Michels RG, Gass JDM. The natural course of retinal branch vein occlusion. Trans Am Acad Ophthalmol Otolaryngol. 1974; 78:166–77.13. Schatz H, Madeira D, McDonald HR, Johnson RN. Progressive enlargement of laser scars following grid laser photocoagulation for diffuse diabetic macular edema. Arch Ophthalmol. 1991; 109:1549–51.
Article14. Morgan CM, Schatz H. Atrophic creep of the retinal pigment epithelium after focal macular photocoagulation. Ophthalmology. 1989; 96:96–103.
Article15. Focal photocoagulation treatment of diabetic macular edema. Relationship of treatment effect to fluorescein angiographic and other retinal characteristics at baseline: ETDRS report no. 19. Early Treatment Diabetic Retinopathy Study Research Group. Arch Ophthalmol. 1995; 113:1144–55.16. Lewen RM. Subretinal neovascularization complicating laser photocoagulation of diabetic maculopathy. Ophthalmic Surg. 1988; 19:734–7.
Article17. Lewis H, Schachat AP, Haimann MH, et al. Choroidal neovascularization after laser photocoagulation for diabetic macular edema. Ophthalmology. 1990; 97:503–10. discussion. 510–1.
Article18. Guyer DR, D'Amico DJ, Smith CW. Subretinal fibrosis after laser photocoagulation for diabetic macular edema. Am J Ophthalmol. 1992; 113:652–6.19. Rutledge BK, Wallow IH, Poulsen GL. Sub-pigment epithelial membranes after photocoagulation for diabetic macular edema. Arch Ophthalmol. 1993; 111:608–13.
Article20. Fong DS, Segal PP, Myers F, et al. Subretinal fibrosis in diabetic macular edema. ETDRS report 23. Early Treatment Diabetic Retinopathy Study Research Group. Arch Ophthalmol. 1997; 115:873–7.21. Han DP, Mieler WF, Burton TC. Submacular fibrosis after photocoagulation for diabetic macular edema. Am J Ophthalmol. 1992; 113:513–21.
Article22. Striph GG, Hart WM Jr, Olk RJ. Modified grid laser photocoagulation for diabetic macular edema. The effect on the central visual field. Ophthalmology. 1988; 95:1673–9.23. Hudson C, Flanagan JG, Turner GS, et al. Influence of laser photocoagulation for clinically significant diabetic macular oedema (DMO) on short-wavelength and conventional automated perimetry. Diabetologia. 1998; 41:1283–92.
Article24. Ishiko S, Ogasawara H, Yoshida A, Hanada K. The use of scanning laser ophthalmoscope microperimetry to detect visual impairment caused by macular photocoagulation. Ophthalmic Surg Lasers. 1998; 29:95–8.
Article25. Okuyama M, Okisaka S. Automatic static threshold perimetry is useful for estimating the effects of laser photocoagulation on diabetic maculopathy. Ophthalmic Res. 1998; 30:207–15.
Article26. Ishibashi T, Miki K, Sorgente N, et al. Effects of intravitreal administration of steroids on experimental subretinal neovascularization in the subhuman primate. Arch Ophthalmol. 1985; 103:708–11.
Article27. Wilson CA, Berkowitz BA, Sato Y, et al. Treatment with intravitreal steroid reduces blood-retinal barrier breakdown due to retinal photocoagulation. Arch Ophthalmol. 1992; 110:1155–9.
Article28. Antoszyk AN, Gottlieb JL, Machemer R, Hatchell DL. The effects of intravitreal triamcinolone acetonide on experimental preretinal neovascularization. Graefes Arch Clin Exp Ophthalmol. 1993; 231:34–40.
Article29. Penfold PL, Wen L, Madigan MC, et al. Modulation of permeability and adhesion molecule expression by human choroidal endothelial cells. Invest Ophthalmol Vis Sci. 2002; 43:3125–30.30. Penfold PL, Wong JG, Gyory J, Billson FA. Effects of triamcinolone acetonide on microglial morphology and quantitative expression of MHC-II in exudative age-related macular degeneration. Clin Experiment Ophthalmol. 2001; 29:188–92.
Article31. Chen SD, Sundaram V, Lochhead J, Patel CK. Intravitreal triamcinolone for the treatment of ischemic macular edema associated with branch retinal vein occlusion. Am J Ophthalmol. 2006; 141:876–83.
Article32. Ozdek S, Deren YT, Gurelik G, Hasanreisoglu B. Posterior subtenon triamcinolone, intravitreal triamcinolone and grid laser photocoagulation for the treatment of macular edema in branch retinal vein occlusion. Ophthalmic Res. 2008; 40:26–31.
Article33. Scott IU, Ip MS, VanVeldhuisen PC, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular Edema secondary to branch retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 6. Arch Ophthalmol. 2009; 127:1115–28.34. Jonas JB, Akkoyun I, Kamppeter B, et al. Branch retinal vein occlusion treated by intravitreal triamcinolone acetonide. Eye. 2005; 19:65–71.
Article35. Cheng KC, Wu WC. Intravitreal triamcinolone acetonide for patients with macular edema due to branch retinal vein occlusion. Kaohsiung J Med Sci. 2006; 22:321–30.
Article36. Gutman FA. Macular edema in branch retinal vein occlusion: prognosis and management. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1977; 83:488–95.37. Lee SU, Kim SJ, Park YM, et al. Grid laser photocoagulation after intravitreal triamcinolone for macular edema associated with branch retinal vein occlusion. J Korean Ophthalmol Soc. 2009; 50:704–9.
Article38. Bhavsar AR, Ip MS, Glassman AR. DRCRnet and the SCORE Study Groups. The risk of endophthalmitis following intravitreal triamcinolone injection in the DRCRnet and SCORE clinical trials. Am J Ophthalmol. 2007; 144:454–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Efficacy of Intravitreal Triamcinolone Acetonide for Macular Edema in Branched Retinal Vein Occlusion
- The Effectiveness of Intravitreal Triamcinolone Injection for the Treatment of Macular Edema
- The Effect of Intravitreal Triamcinolone Acetonide on Cystoid Macular Edema
- Intravitreal Triamcinolone Versus Bevacizumab for Treatment of Macular Edema Secondary to Branch Retinal Vein Occlusion
- Grid Laser Photocoagulation After Intravitreal Triamcinolone for Macular Edema Associated With Branch Retinal Vein Occlusion