J Korean Ophthalmol Soc.
2011 Mar;52(3):364-372. 10.3341/jkos.2011.52.3.364.
A Case Report of Acute Zonal Occult Outer Retinopathy Showing Acute Idiopathic Blind Spot Enlargement
- Affiliations
-
- 1Department of Ophthalmology, Kyungpook National University School of Medicine, Daegu, Korea. fhak@dreamwiz.com
- KMID: 2214304
- DOI: http://doi.org/10.3341/jkos.2011.52.3.364
Abstract
- PURPOSE
To present a case of acute zonal occult outer retinopathy (AZOOR) with acute idiopathic blind spot enlargement (AIBSE) investigated using indocyanine green angiography (ICGA), multifocal electroretinography (multifocal ERG) and spectral domain-OCT (SD-OCT).
CASE SUMMARY
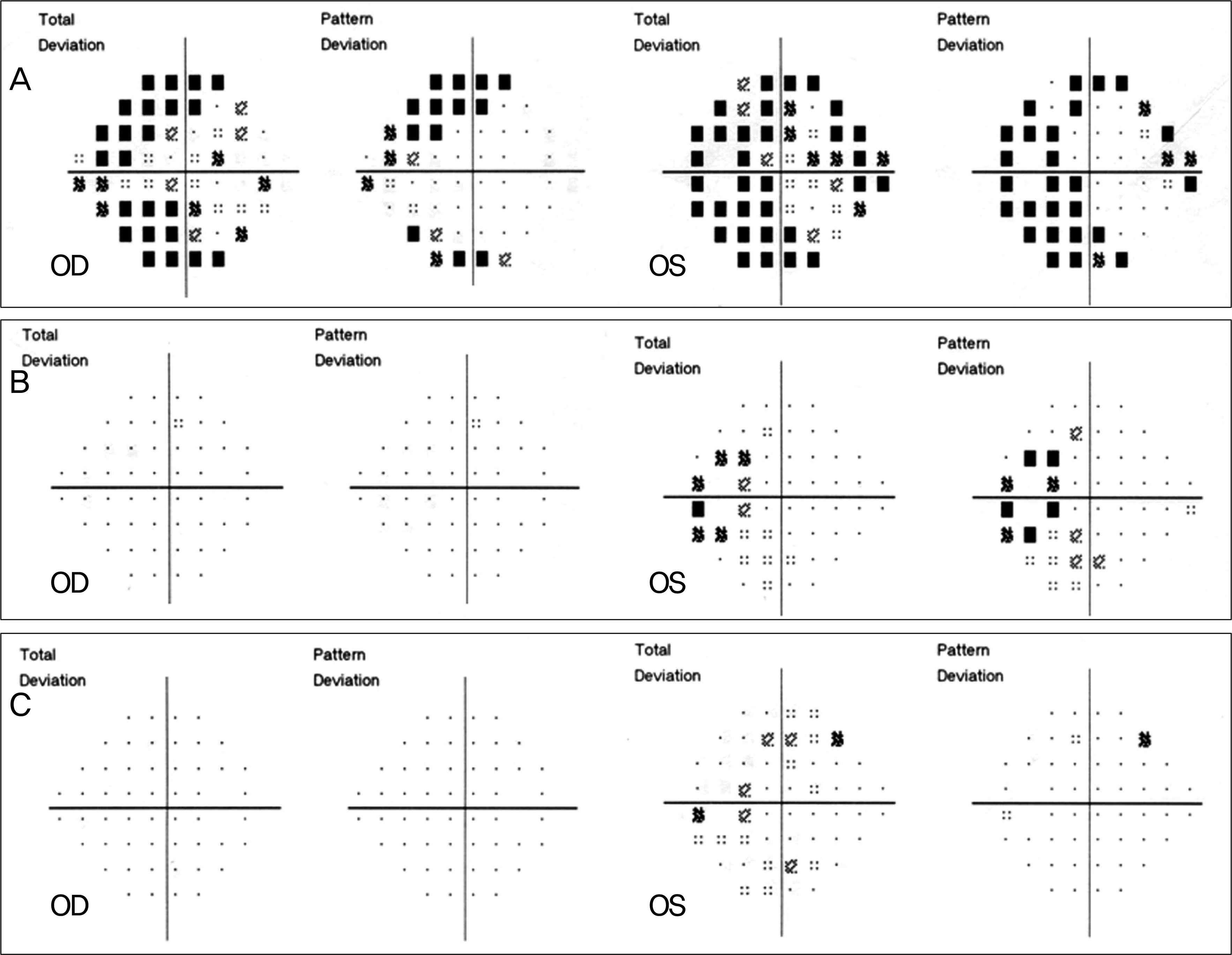
A healthy 31-year-old female with photopsia and a five-day visual field defect in her left eye showed no abnormal findings in ocular examinations such as slit lamp and fundus examination, fluorescein angiography (FAG), or full field ERG as well as in the systemic neurologic examination. In the late phase of ICGA, there were multiple hypofluorescent spots around the optic disc and scattered through the posterior pole. The patient showed an amplitude decrease of multifocal ERG and the destruction of the boundary between the inner and outer segments of the photoreceptors in the SD-OCT examined in the retinal area corresponding to the visual field defect. The patient was diagnosed with AZOOR and was followed-up without treatment. After three months, no abnormal SD-OCT or visual field test findings were observed and no symptoms remained; however, a slightly depressed response on multifocal ERG was present.
CONCLUSIONS
ICGA, multifocal ERG and SD-OCT could be useful methods to detect AZOOR with EBS.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Ocular Syphilis Presented as Occult Outer Retinopathy
Sung Who Park, Jong Ho Park, Ik Soo Byon, Ji Eun Lee
J Korean Ophthalmol Soc. 2014;55(5):785-788. doi: 10.3341/jkos.2014.55.5.785.Clinical Characteristics of Acute Zonal Occult Outer Retinopathy
Ki Woong Bae, Kyu Hyung Park, Se Joon Woo, Jeong Min Hwang
J Korean Ophthalmol Soc. 2016;57(3):413-419. doi: 10.3341/jkos.2016.57.3.413.
Reference
-
References
1. Fletcher WA, Imes RK, Goodman D, Hoyt WF. Acute idiopathic blind spot enlargement. A big blind spot syndrome without optic disc edema. Arch Ophthalmol. 1988; 106:44–9.2. Hamed LM, Glaser JS, Gass JD, Schatz NJ. Protracted enlargement of the blind spot in multiple evanescent white dot syndrome. Arch Ophthalmol. 1989; 107:194–8.
Article3. Jampol LM, Wiredu A. MEWDS, MFC, PIC, AMN, AIBSE, and AZOOR: one disease or many? Retina. 1995; 15:373–8.4. Gass JD. Overlap among acute idiopathic blind spot enlargement syndrome and other conditions. Arch Ophthalmol. 2001; 119:1729–31.
Article5. Hamed LA, Schatz NJ, Glaser JS, Gass JD. Acute idiopathic blind spot enlargement without optic disc edema. Arch Ophthalmol. 1988; 106:1030–1.
Article6. Gass JD. The acute zonal outer retinopathies. Am J Ophthalmol. 2000; 130:655–7.
Article7. Gass JD. Acute zonal occult outer retinopathy. Donders Lecture: The Netherlands Ophthalmological Society, Maastricht, Holland, June 19, 1992. J Clin Neuroophthalmol. 1993; 13:79–97.8. Gass JD, Agarwal A, Scott IU. Acute zonal occult outer retinopathy: a long-term followup study. Am J Ophthalmol. 2002; 134:329–39.
Article9. Choi HJ, Hwang JM. A Case report of acute zonal occult outer retinopathy. J Korean Ophthalmol Soc. 2003; 44:1384–91.10. Yasuda K, Shimura M, Noro M, et al. Clinical course of acute retinal zonal occult outer retinopathy in visual field and multifocal electroretinogram. Br J Ophthalmol. 1999; 83:1089–90.11. Kondo N, Kondo M, Miyake Y. Acute idiopathic blind spot enlargement syndrome: prolonged retinal dysfunction revealed by multifocal electroretinogram technique. Am J Ophthalmol. 2001; 132:126–8.
Article12. Pece A, Sadun F, Trabucchi G, Brancato R. Indocyanine green angiography in enlarged blind spot syndrome. Am J Ophthalmol. 1998; 126:604–7.
Article13. Spaide RF, Koizumi H, Freund KB. Photoreceptor outer segment abnormalities as a cause of blind spot enlargement in acute zonal occult outer retinopathy-complex diseases. Am J Ophthalmol. 2008; 146:111–20.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fulminant Progressive Atypical Acute Zonal Occult Outer Retinitis
- Acute Zonal Occult Outer Retinopathy Mimicking Retrobulbar Optic Neuritis
- A Case Report of Acute Zonal Occult Outer Retinopathy
- Acute Zonal Occult Outer Retinopathy, Responsive to an Immunosuppressive Agent: A Case Report
- Ocular Syphilis Presented as Occult Outer Retinopathy