J Korean Ophthalmol Soc.
2009 Aug;50(8):1174-1178. 10.3341/jkos.2009.50.8.1174.
Transscleral IOL Fixation With Preserved Anterior Vitreous Face in Marfan Syndrome With Ectopia Lentis
- Affiliations
-
- 1Department of Ophthalmology, Maryknoll Hospital, Busan, Korea. wansookim@yahoo.com
- 2Department of Ophthalmology, St. Mary's Hosital, Busan, Korea.
- KMID: 2212530
- DOI: http://doi.org/10.3341/jkos.2009.50.8.1174
Abstract
- PURPOSE
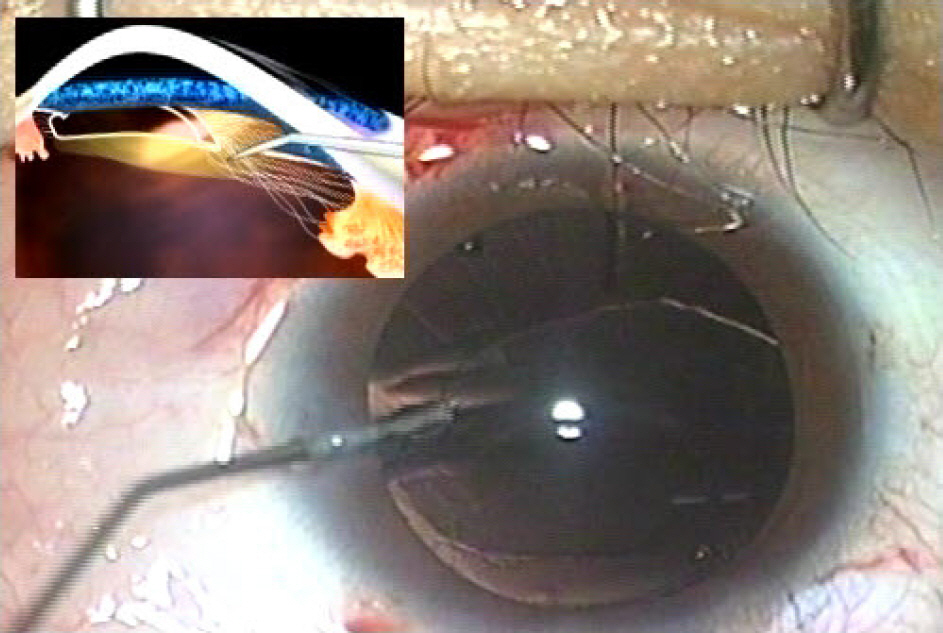
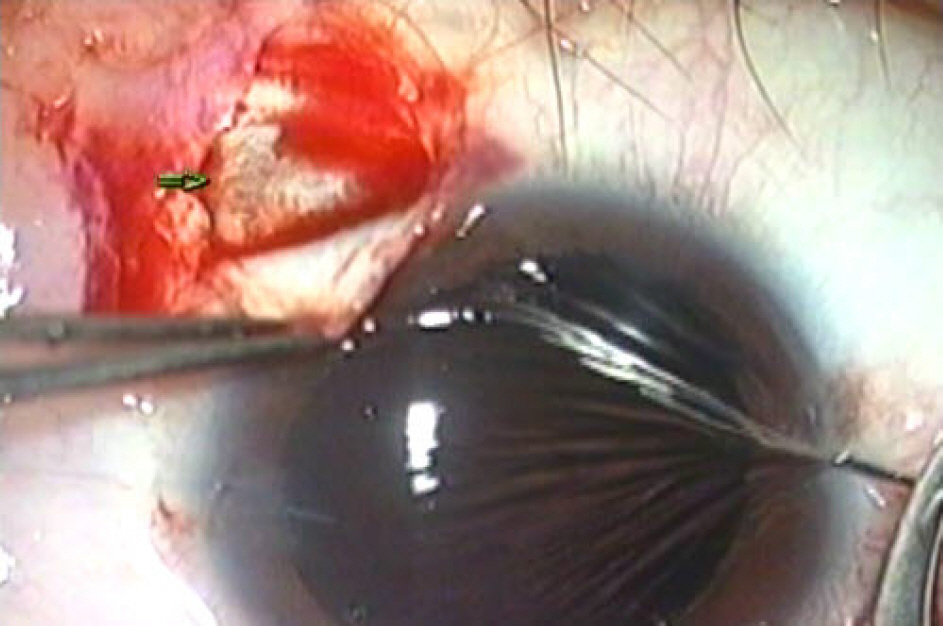
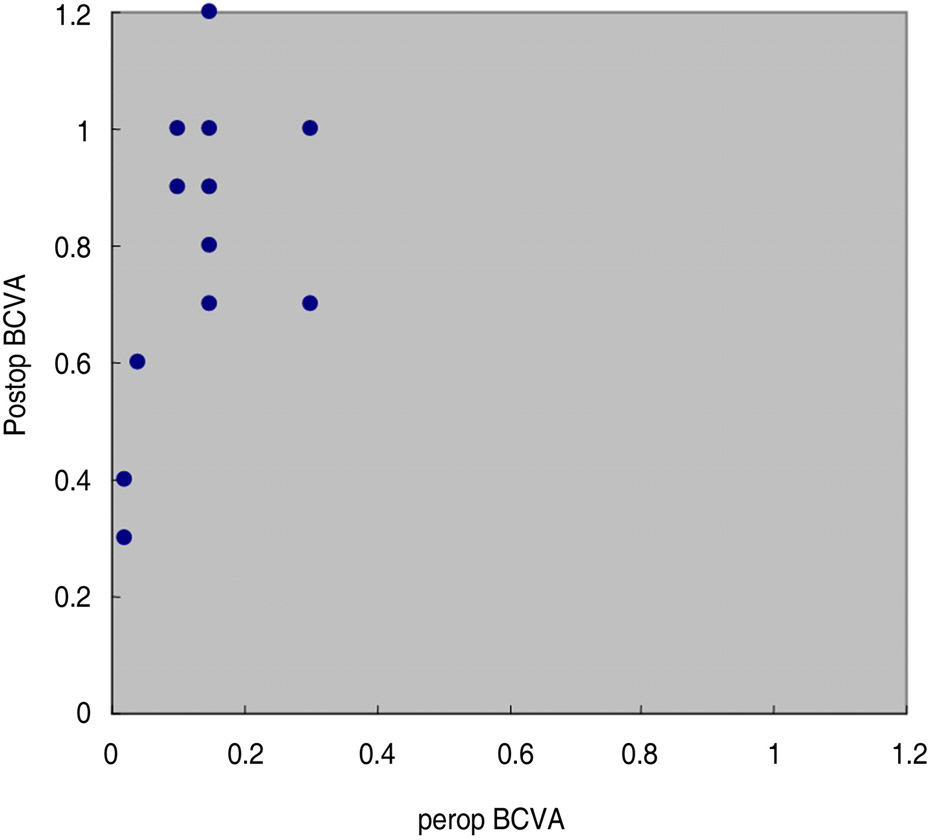
To evaluate the safety and efficacy of transscleral intraocular lens (IOL) fixation while preserving the anterior vitreous face in treating ectopia lentis of Marfan syndrome. METHODS: This study included six patients (12 eyes) who had undergone surgical intervention for ectopia lentis with or without lenticular opacity. We compared the best-corrected visual acuity (BCVA) before and after the surgery and evaluated perioperative complications. RESULTS: The mean age at the time of surgery was 18.2+/-10.7 years. The mean follow-up period was 11.2+/-7.1 months. Mean BCVA scores changed from 0.96+/-0.37 (LogMar Value) to 0.14+/-0.17 (LogMar Value). All patients showed more than two lines of improvement in visual acuity. In two eyes, pupillary capture was found. Medically controllable intraocular pressure elevation was found in three eyes. CONCLUSIONS: This study suggests that transscleral IOL fixation with a preserved anterior vitreous face can be a safe and effective technique in treating the ectopia lentis of Marfan syndrome.
MeSH Terms
Figure
Reference
-
References
1. Maumenee IH. The eye in the Marfan syndrome. Trans Am Ophthalmol Soc. 1981; 79:684–733.2. Cross HE, Hensen AD. Ocular manifestation in the Marfan syndrome and homocystinuria. Am J Ophthalmol. 1973; 75:403–20.3. Nelson LB, Maumenee IH. Ectopia lentis. Surv Ophthalmol. 1982; 27:143–60.
Article4. Hindle NW, Crawford JS. Dislocation of the lens in Marfan's syndrome. Can J Ophthalmol. 1969; 4:128–34.5. Allen RA, Straatsma BR, Apt L, Hall MO. Ocular manifestations of the Marfan syndrome. Trans Am Acad Ophthalmol Otolaryngol. 1967; 71:18–38.6. Stephenson WV. Anterior megalophthalmos and arachnodactyly. Am J Ophthalmol. 1954; 8:315–7.7. Reese PD, Weingeist TA. Pars plana management of ectopia lentis in children. Arch Ophthalmol. 1987; 105:1202–4.
Article8. Halpert M, BenErzra D. Surgery of the hereditary subluxated lens in children. Ophthalmology. 1996; 103:681–6.
Article9. Yu YS, Kang YH, Lim KH. Improvements in visual acuity following limbal lensectomy for subluxated lenses in children. Ophthalmic Surg Lasers. 1997; 28:1006–10.
Article10. Dietlein TS, Jacobi PC, Konen W, Krieglstein GK. Complications of endocapsular tension ring implantation in a child with Marfan's syndrome. J Cataract Refract Surg. 2000; 26:937–40.
Article11. Yu YS, Awh JY, Lee JH. Management of ectopia lentis in children. J Korean Ophthalmol Soc. 1999; 40:1979–8.12. Romano PE, Kerr NC, Hope GM. Bilateral ametropic functional amblyopia in genetic ectopia lentis: its relation to the amount of subluxation, an indicator for early surgical treatment. Binocular Vis Strabismus Q. 2002; 17:235–41.13. Guo X, Chen Y. Post lensectomy amblyopia therapy in patients with ectopia lentis. Binocular Vision Eye Surg. 1994; 9:309–12.14. Straatsma BR, Allen RA, Pettit TH, Hall MO. Subluxation of the lens treated with iris photocoagulation. Am J Ophthalmol. 1966; 61:1312–24.
Article15. Maumenee AE, Ryan SJ. Aspiration technique in the management of the dislocated lens. Am J Ophthalmol. 1969; 68:808–12.
Article16. Varga B. The results of my operations improving visual acuity of ectopia lentis. Ophthalmologica. 1971; 162:98–110.
Article17. Jensen AD, Cross HE. Surgical treatment of dislocated lenses in the Marfan syndrome and homocystinuria. Trans Am Acad Ophthalmol Otolaryngol. 1972; 76:1491–9.18. Peyman GA, Raichand M, Goldberg MF, Ritacia D. Management of subluxated and dislocated lenses with the vitriophage. Br J Ophthalmol. 1979; 63:771–8.19. Girard LJ. Pars plana lensectomy for subluxated and dislocated lenses. Ophthalmic Surg. 1981; 12:491–5.
Article20. Tsai Y, Tseng S. Transscleral fixation of foldable intraocular lens after pars plana lensectomy in eyes with a subluxated lens. J Cataract Refract Surg. 1999; 25:722–6.
Article21. Ruttum MS. Managing situations involving children with ectopia lentis. J Pediatr Ophthalmol Strabismus. 1995; 32:74–5.
Article22. Vadala P, Capozzi P, Fortunato M, et al. Intraocular lens implantation in Marfan syndrome. J Pediatr Ophthalmol Strabismus. 2000; 37:206–8.