J Korean Surg Soc.
2013 Aug;85(2):51-57. 10.4174/jkss.2013.85.2.51.
Efficacy and safety of hyaluronate membrane in the rabbit cecum-abdominal wall adhesion model
- Affiliations
-
- 1Department of Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea. wizard95@cha.ac.kr
- 2R&D Center, Genewel Co., Seongnam, Korea.
- KMID: 2212516
- DOI: http://doi.org/10.4174/jkss.2013.85.2.51
Abstract
- PURPOSE
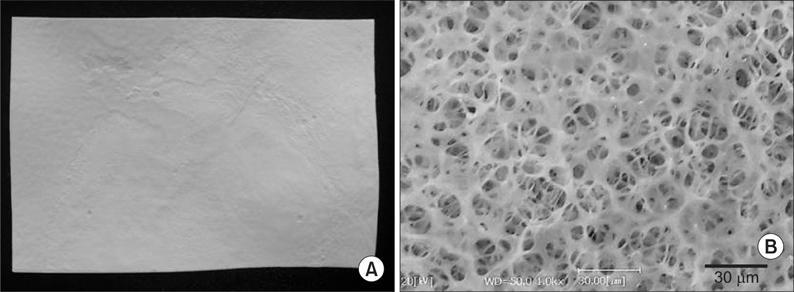
Tissue adhesion is a well-known postsurgical phenomenon, causing pain, functional obstruction, and difficult reoperative surgery. To overcome these problems, various synthetic and natural polymer membranes have been developed as postoperative tissue adhesion barriers. However, limitation in their use has hindered its actual application. We prepared a hyaluronate membrane (HM) to evaluate its efficacy and safety as an adhesion barrier compared to a commercialized product (Interceed, Ethicon).
METHODS
To evaluate the antiadhesion effect, a cecum-abdominal wall abrasion model was adopted in a rabbit. The denuded cecum was covered by Interceed or HM or neither and apposed to the abdominal wall (each, n = 10). Four weeks after surgery, the level of adhesion was graded. Acute and chronic toxicity of the three groups were also evaluated.
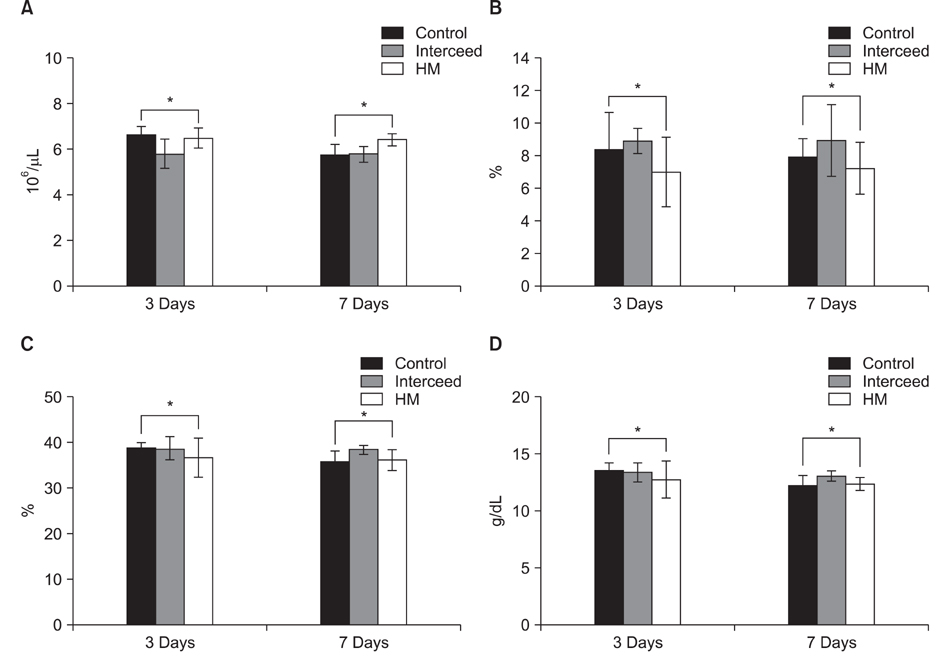
RESULTS
Blood samples drawn to evaluate acute toxicity at postoperative day 3 and 7 showed no significant difference among the three groups. The grade and area of adhesion were significantly lower in the HM compared to those of the control and Interceed at four weeks after surgery. Histologic evaluations, which was carried out to estimate tissue reactions at the site of application, as well as to assess chronic toxicity for the major organs, were not significantly different in the three groups.
CONCLUSION
This study showed that the antiadhesion efficacy of HM was superior to commercialized antiadhesion membrane, Interceed. Low inflammatory response and nontoxicity were also demonstrated. From these results, we suggest that the HM is a good candidate as a tissue adhesion barrier.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Effect of polylactic film (Surgi-Wrap) on preventing postoperative ileus after major hepato-pancreato-biliary surgery
Chang Hyung Lee, Hongbeom Kim, In Woong Han, Suh Min Kim, Beom Seok Kwak, Yong Hae Baik, Young Jin Park, Min Gu Oh
Ann Hepatobiliary Pancreat Surg. 2016;20(4):191-196. doi: 10.14701/ahbps.2016.20.4.191.
Reference
-
1. Yang HY, Suh KS, Youn YK, Kim SW, Kim SJ, Lee KU, et al. A clinical analysis of intestinal obstruction in the adult. J Korean Surg Soc. 1997. 52:335–342.2. Almeida OD Jr, Val-Gallas JM. Conscious pain mapping. J Am Assoc Gynecol Laparosc. 1997. 4:587–590.3. Marana R, Muzii L. DiZerega GS, editor. Infertility and adhesions. Peritoneal surgery. 2000. New York: Springer-Verlag;329–333.4. Lee WJ, Moon BI, Park JB, Kim IM, You BO. The factors influencing the treatment for the mechanical intestinal obstruction due to adhesion. J Korean Surg Soc. 1995. 49:192–203.5. Falk K, Bjorquist P, Stromqvist M, Holmdahl L. Reduction of experimental adhesion formation by inhibition of plasminogen activator inhibitor type 1. Br J Surg. 2001. 88:286–289.6. Shim HS, Lee YW, Lee YM, Oh YH, Kwon SW, Kim JH, et al. Evaluation of resorbable materials for preventing surgical adhesion on rat experiment. J Korean Surg Soc. 2002. 63:179–186.7. Burns JW, Colt MJ, Burgees LS, Skinner KC. Preclinical evaluation of Seprafilm bioresorbable membrane. Eur J Surg Suppl. 1997. 40–48.8. Haney AF, Doty E. Murine peritoneal injury and de novo adhesion formation caused by oxidized-regenerated cellulose (Interceed [TC7]) but not expanded polytetrafluoroethylene (Gore-Tex Surgical Membrane). Fertil Steril. 1992. 57:202–208.9. Wiseman DM, Gottlick-Iarkowski L, Kamp L. Effect of different barriers of oxidized regenerated cellulose (ORC) on cecal and sidewall adhesions in the presence and absence of bleeding. J Invest Surg. 1999. 12:141–146.10. Wiseman DM, Trout JR, Diamond MP. The rates of adhesion development and the effects of crystalloid solutions on adhesion development in pelvic surgery. Fertil Steril. 1998. 70:702–711.11. Rajab TK, Wallwiener M, Talukdar S, Kraemer B. Adhesionrelated complications are common, but rarely discussed in preoperative consent: a multicenter study. World J Surg. 2009. 33:748–750.12. Song HJ, Kim JW, Park JS, Kim YS, Choi YS, Kim BG, et al. Effects of three different types of anti-adhesive agents in a rat abdominal wall defect model. J Korean Surg Soc. 2009. 77:7–14.13. Yaacobi Y, Israel AA, Goldberg EP. Prevention of postoperative abdominal adhesions by tissue precoating with polymer solutions. J Surg Res. 1993. 55:422–426.14. Luciano AA, Hauser KS, Benda J. Evaluation of commonly used adjuvants in the prevention of postoperative adhesions. Am J Obstet Gynecol. 1983. 146:88–92.15. Oh SH, Kim JK, Song KS, Noh SM, Ghil SH, Yuk SH, et al. Prevention of postsurgical tissue adhesion by anti-inflammatory drug-loaded pluronic mixtures with sol-gel transition behavior. J Biomed Mater Res A. 2005. 72:306–316.16. Lee YW, Chu B, Lee YG, Kim NH, Kim JH, Kim KI, et al. Efficacy and safety of the electrospun nanofibrous adhesion barrier for laparoscopic surgery in a rabbit model. J Korean Surg Soc. 2009. 76:73–80.17. Kwon SW, Lim SH, Lee YW, Lee YG, Chu BY, Lee JH, et al. Anti-adhesive effect of poloxamer/alginate/CaCl2 mixture in the rat model. J Korean Surg Soc. 2006. 71:280–287.18. Avital S, Bollinger TJ, Wilkinson JD, Marchetti F, Hellinger MD, Sands LR. Preventing intra-abdominal adhesions with polylactic acid film: an animal study. Dis Colon Rectum. 2005. 48:153–157.19. Ersoy E, Ozturk V, Yazgan A, Ozdogan M, Gundogdu H. Effect of polylactic acid film barrier on intra-abdominal adhesion formation. J Surg Res. 2008. 147:148–152.20. Cordewener FW, Bos RR, Rozema FR, Houtman WA. Poly(L-lactide) implants for repair of human orbital floor defects: clinical and magnetic resonance imaging evaluation of long-term results. J Oral Maxillofac Surg. 1996. 54:9–13.21. Boland GM, Weigel RJ. Formation and prevention of postoperative abdominal adhesions. J Surg Res. 2006. 132:3–12.22. Franklin RR. Reduction of ovarian adhesions by the use of Interceed. Ovarian Adhesion Study Group. Obstet Gynecol. 1995. 86:335–340.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Efficacy and Safety of HA/CMC Anti-adhesion Barrier Solution with Varying Viscosities
- Evaluation of Resorbable Materials for Preventing Surgical Adhesion on Rat Experiment
- Efficacy and Safety of the Electrospun Nanofibrous Adhesion Barrier for Laparoscopic Surgery in a Rabbit Model
- Anti-adhesive Effect of Poloxamer/Alginate/CaCl2 Mixture in the Rat Model
- The Effect of Hyaluronate Membrane on Prevention of Adhesion after Rectal Cancer Surgery: a Prospective Study