J Korean Ophthalmol Soc.
2009 Jun;50(6):957-962. 10.3341/jkos.2009.50.6.957.
A Case of Functional Bitemporal Hemianopia Respecting the Vertical Meridian
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University School of Medicine, Seoul, Korea. hjm@snu.ac.kr
- 2Department of Ophthalmology, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2212378
- DOI: http://doi.org/10.3341/jkos.2009.50.6.957
Abstract
-
PURPOSE: To report a case of functional bilateral hemianopia which was not associated with any organic causes.
CASE SUMMARY
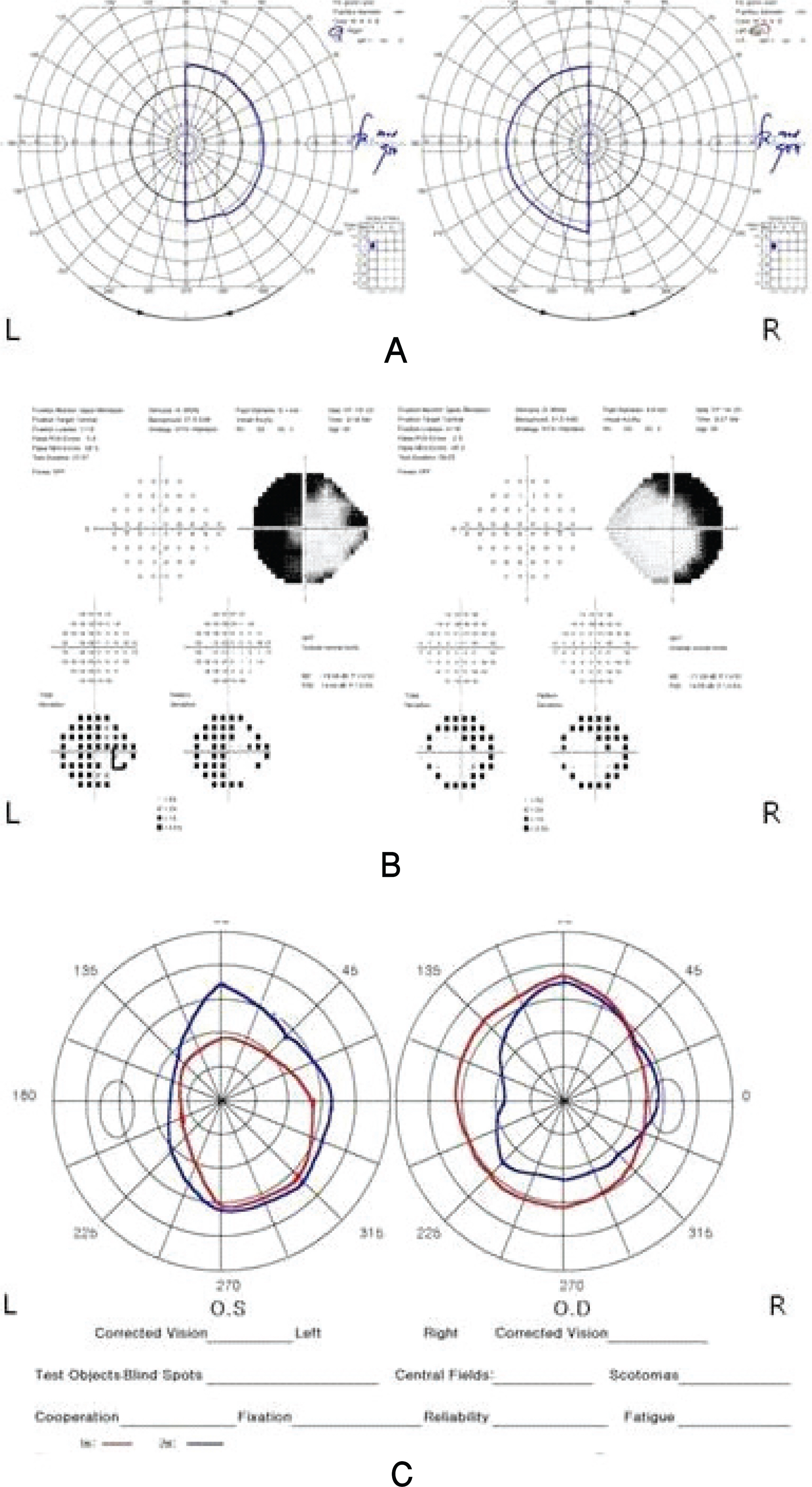
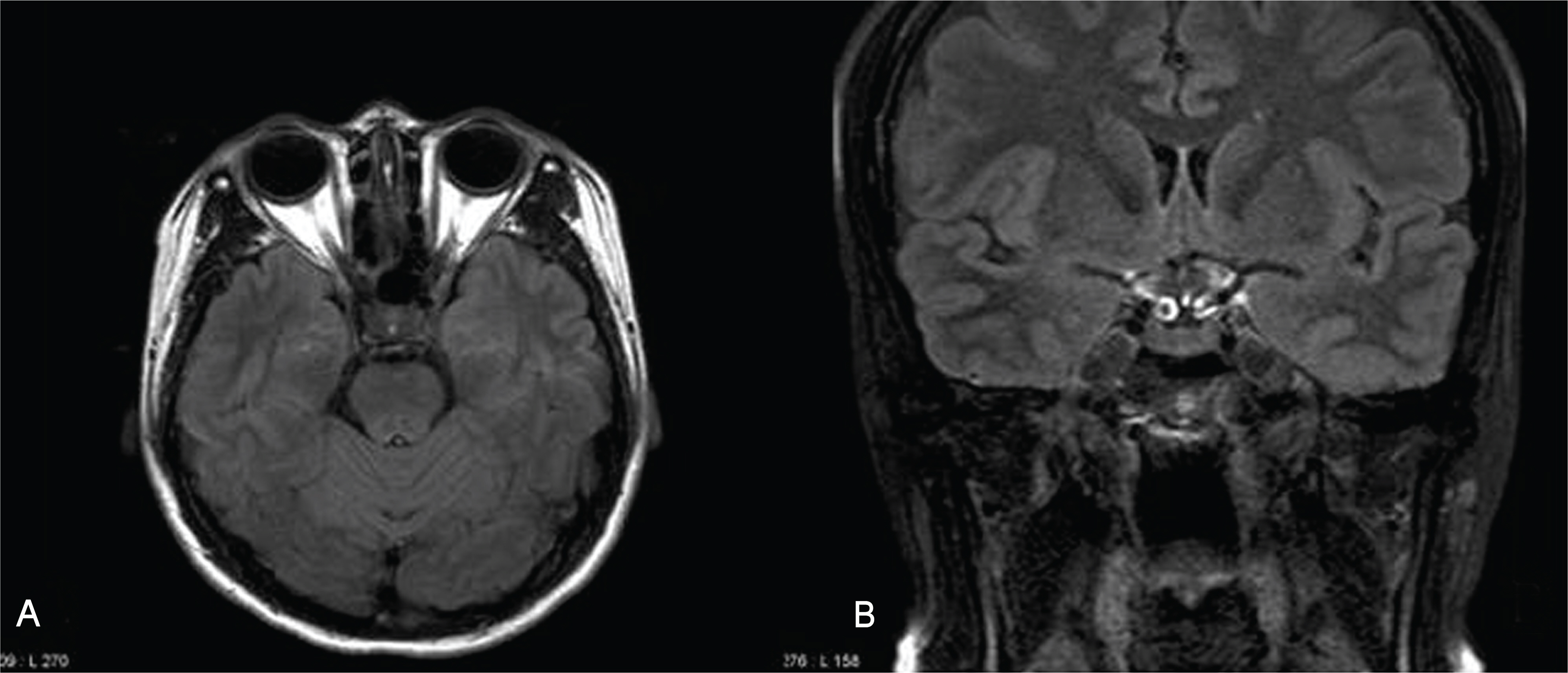
A 35-year-old female patient presented with bilateral disturbance of visual acuity and visual field, which had begun 8 months prior. Goldmann perimetry showed bitemporal hemianopsia respecting the vertical meridian. Pupillary response was normal, and the anterior segment, fundus, and optic nerve were also normal bilaterally. However, the tangent screen test and Humphrey visual field test showed a widening of hemianopia not respecting the vertical meridian, and the crossing of isopters at 1 m and 2 m with the tangent screen test. In addition, multifocal electroretinogram and multifocal visual evoked potential did not reveal any abnormal findings corresponding to the bitemporal hemianopia. Brain magnetic resonance imaging showed no abnormal findings in the orbit and brain.
CONCLUSIONS
Bitemporal hemianopsia can be developed functionally, although it may be rare. Repetition of various visual field tests and use of multifocal electrophysiologic studies can be helpful in the differential diagnosis.
MeSH Terms
Figure
Reference
-
References
1. Palmowski AM, Fischer A, Ruprecht KW. Multifocal examination techniques in malingering: case report of a patient with monocular vertical hemianopia. Graefes Arch Clin Exp Ophthalmol. 2003; 241:70–1.
Article2. Hershenfeld SA, Sharpe JA. Monocular temporal hemianopia. Br J Ophthalmol. 1993; 77:424–7.
Article3. Bakker SL, Hasan D, Bijvoet HW. Compression of the visual pathway by anterior cerebral artery aneurysm. Acta Neurol Scand. 1999; 99:204–7.
Article4. Hilton GF, Hoyt WF. An arteriosclerotic chiasmal syndrome. Bitemporal hemianopia associated with fusiform dilatation of the anterior cerebral arteries. JAMA. 1966; 196:1018–20.
Article5. Shikishima K, Kitahara K, Mizobuchi T, Yoshida M. Interpretation of visual field defects respecting the vertical meridian and not related to distinct chiasmal or postchiasmal lesions. J Clin Neurosci. 2006; 13:923–8.
Article6. Smith TJ, Baker RS. Perimetric findings in functional disorders using automated techniques. Ophthalmology. 1987; 94:1562–6.
Article7. Ohkubo H. Visual field in hysteria-reliability of visual field by Goldmann perimetry. Doc Ophthalmol. 1989; 71:61–7.
Article8. Thompson JC, Kosmorsky GS, Ellis BD. Field of dreamers and dreamed-up fields: functional and fake perimetry. Ophthalmology. 1996; 103:117–25.9. Kim SY, Lee DH, Park SH. An analysis of visual fields in patients with posttraumatic functional visual loss. J Korean Ophthalmol Soc. 2004; 45:469–79.10. Keltner JL, Johnson CA, Spurr JO, Beck RW. Baseline visual field profile of optic neuritis. The experience of the optic neuritis treatment trial. Optic Neuritis Study Group. Arch Ophthalmol. 1993; 1112:31–4.11. Gittinger JW Jr. Functional monocular temporal hemianopsia. Am J Ophthalmol. 1986; 101:226–31.
Article12. Savino PJ, Glaser JS, Schatz NJ. Traumatic chiasmal syndrome. Neurology. 1980; 30:963–70.
Article13. Johnson LN, Rabinowitz YS, Hepler RS. Hemianopia respecting the vertical meridian and with foveal sparing from retinal degeneration. Neurology. 1989; 39:872–3.
Article14. Miele DL, Odel JG, Behrens MM, et al. Functional bitemporal quadrantopia and the multifocal visual evoked potential. J Neuroophthalmol. 2000; 20:159–62.
Article15. Massicotte EC, Semela L, Hedges TR 3rd. Multifocal visual evoked potential in nonorganic visual field loss. Arch Ophthalmol. 2005; 123:364–7.
Article16. Goldberg I, Graham SL, Klistorner AI. Multifocal objective perimetry in the detection of glaucomatous field loss. Am J Ophthalmol. 2002; 133:29–39.17. Maccolini E, Andreoli A, Valde G, et al. Hemifield pattern-reversal visual evoked potentials (VEPs) in retrochiasmal lesions with homonymous visual field defect. Ital J Neurol Sci. 1986; 7:437–42.
Article18. Woung LC, Jou JR, Liaw SL. Visual function in recovered ethambutol optic neuropathy. J Ocul Pharmacol Ther. 1995; 11:411–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bitemporal Hemianopia Associated with Anti-Tuberculosis Medication
- Optic Chiasmal Enhancement Revealed by Magnetic Resonance Imaging in a Patient with Ethambutol-induced Toxic Optic Neuropathy
- Reversible Homonymous Hemianopia Associated with Focal Hyperperfusion in Hyperglycemic State
- Correlation of OCT and Hemifield Pattern VEP in Hemianopia
- Bitemporal Hemianopsia in Ethambutol-Induced Optic Neuropathy