J Korean Ophthalmol Soc.
2009 Feb;50(2):308-312. 10.3341/jkos.2009.50.2.308.
Late-onset Hypertrophic Corneal Scars After Laser-assisted Subepithelial Keratectomy With Mitomycin C
- Affiliations
-
- 1Department of Ophthalmology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. hwtchah@amc.seoul.kr
- KMID: 2212069
- DOI: http://doi.org/10.3341/jkos.2009.50.2.308
Abstract
- PURPOSE
To report late-onset hypertrophic corneal scars after laser epithelial keratomileusis (LASEK) with mitomycin C.
CASE SUMMARY
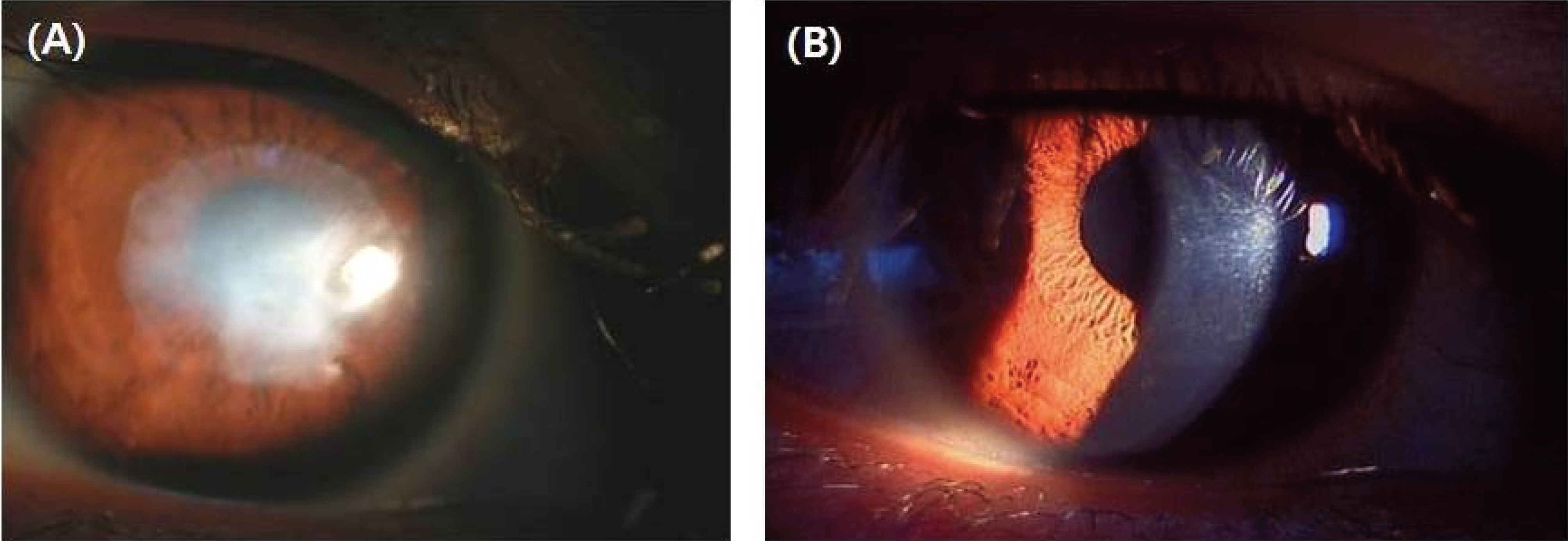
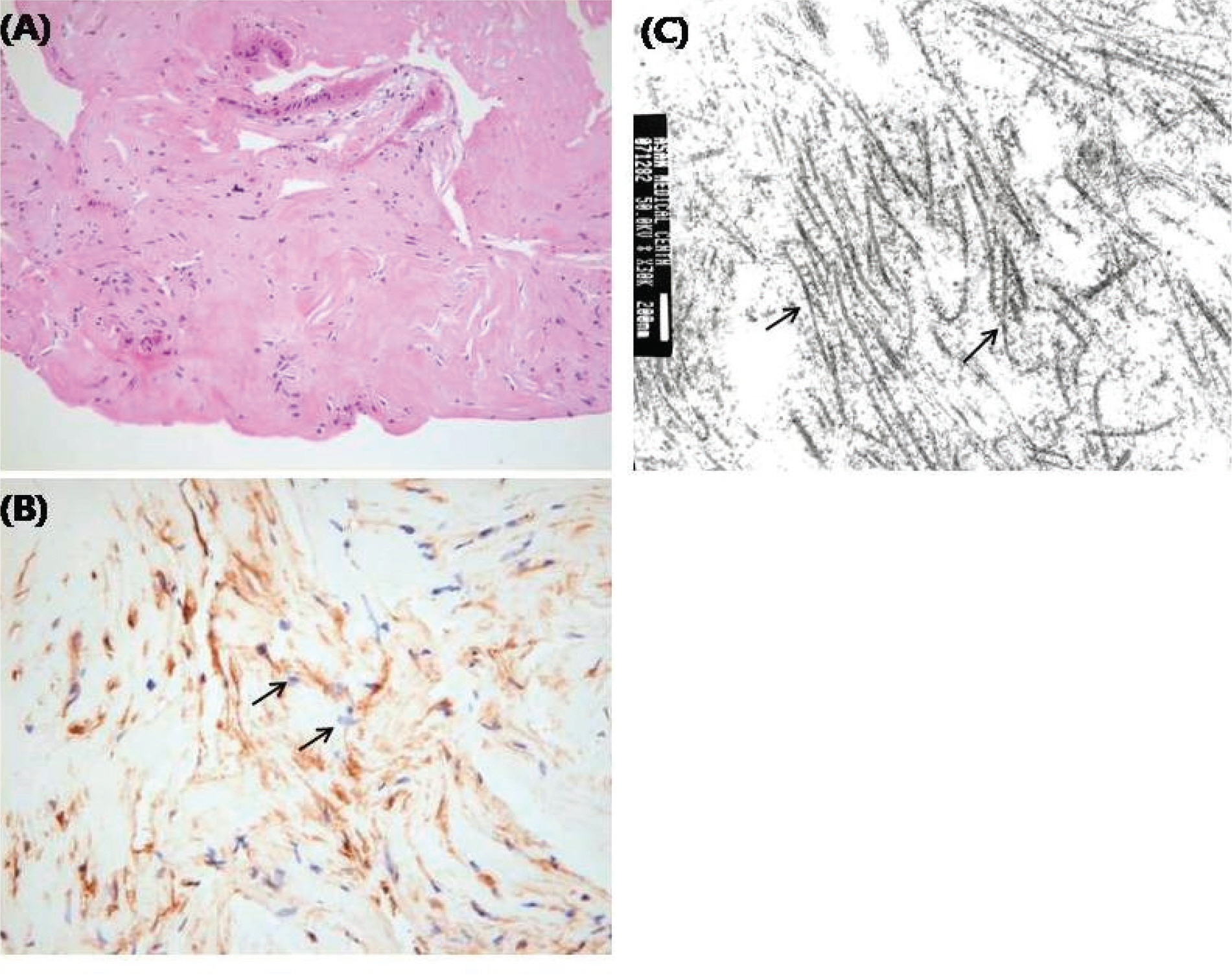
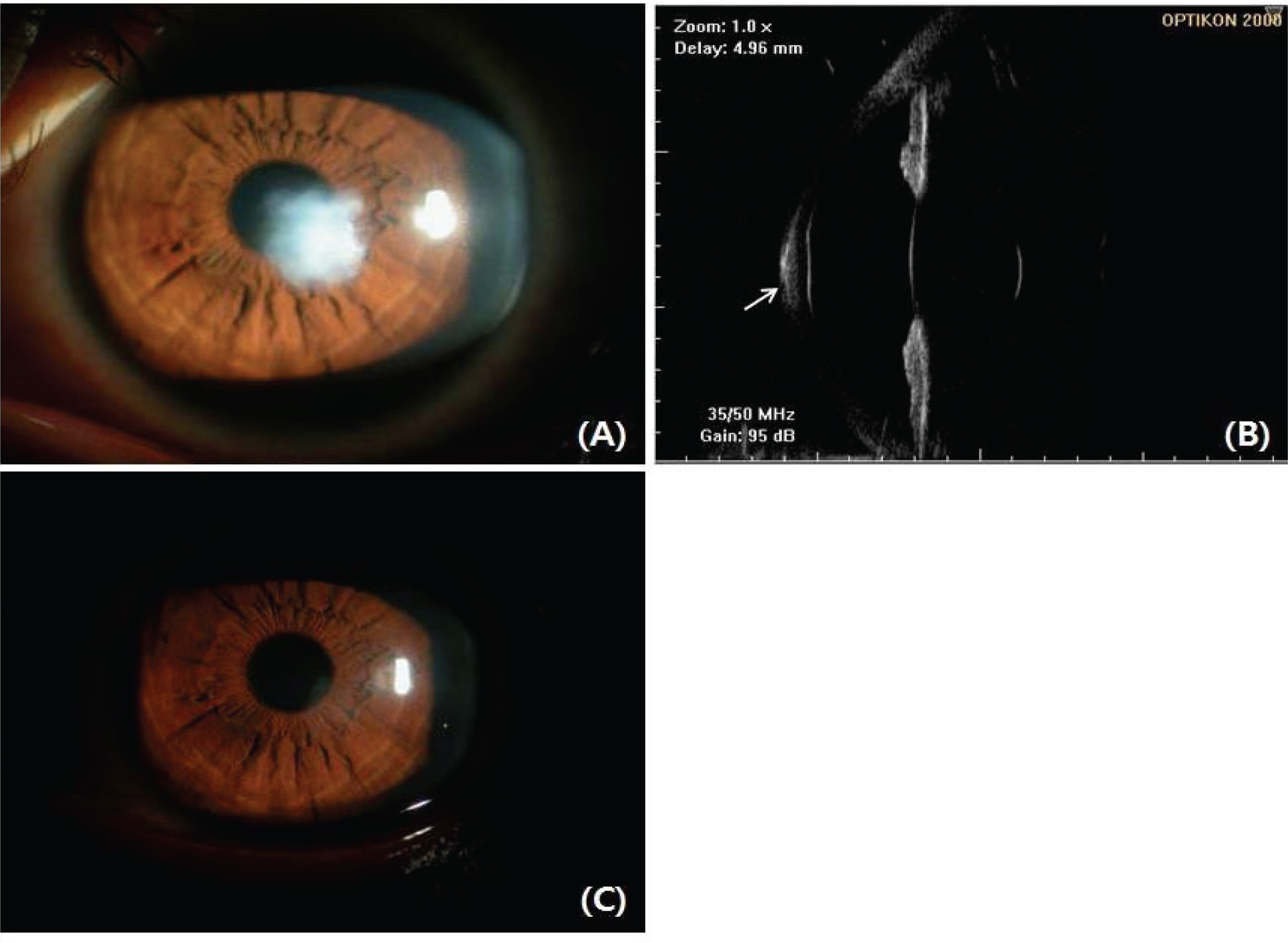
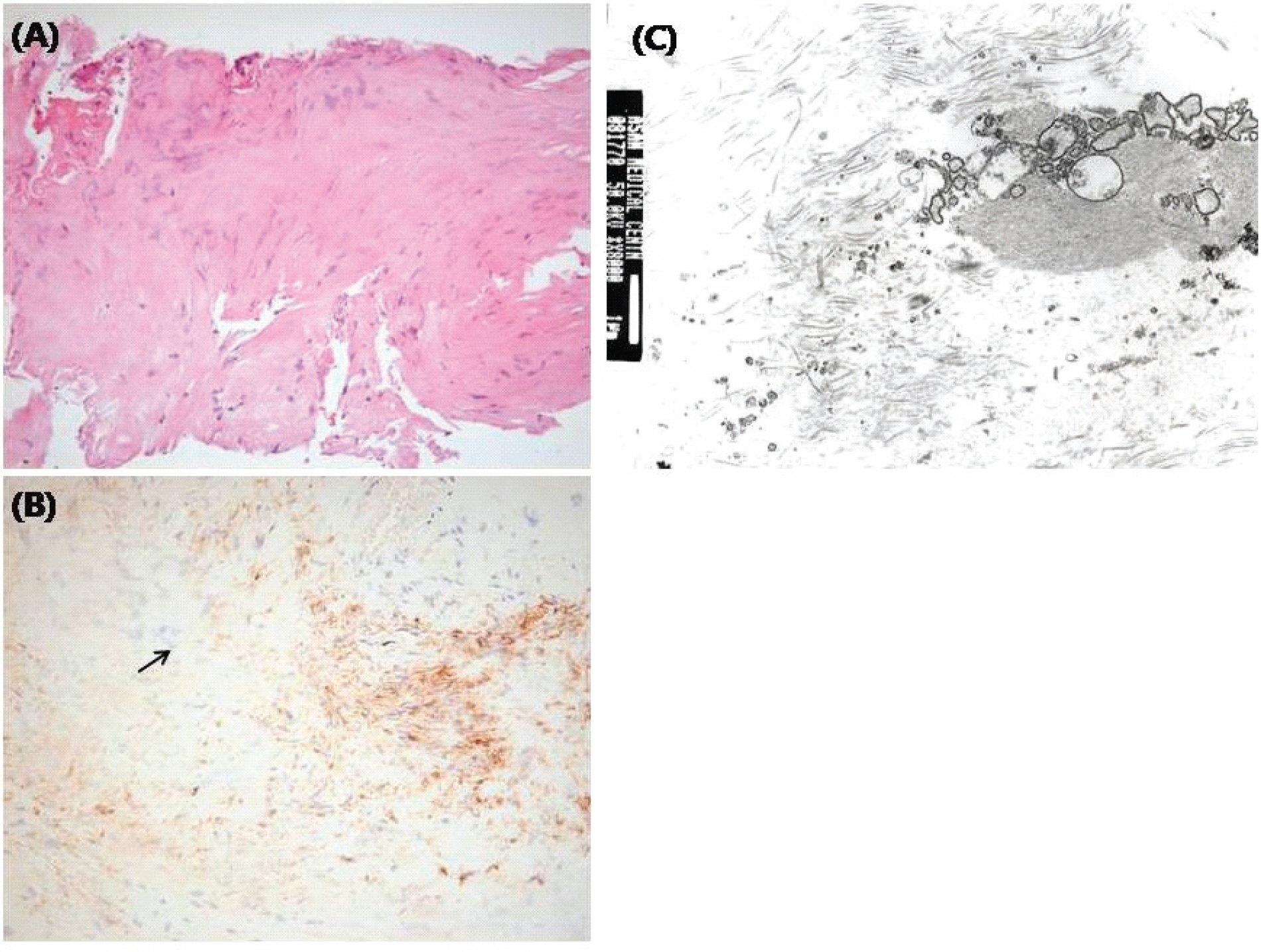
Case 1. A 34-year-old man who had undergone LASEK with mitomycin C 15 months prior was referred to our clinic because of corneal opacity of his right eye. After LASEK, there have been no abnormalities in either of his eyes. However, 11 monthsafter LASEK, he experienced decreased visual acuity in his right eye. The visual acuity was 0.03 in his right eye and 1.0 in his left eye. On slit lamp examination there was a whitish, hypertrophic scarin his right cornea. The lesion was located in the corneal center and the subepithelial space. Central corneal thickness was 828 microm. Case 2. A 23-year-old woman who had undergone LASEK with mitomycin C 14 months before was referred our clinic because of corneal opacity of her left eye. After LASEK, there had been no abnormalities in either of her eyes. However, 12 months after LASEK she experienced decreased visual acuity in her left eye. The visual acuity was 1.0 in her right eye and 0.2 in her left eye. On slit lamp examination there was a whitish, hypertrophic scar in her left cornea. Central corneal thickness was 794 microm.
CONCLUSIONS
Manual debridement was performed to remove the hypertrophic scar in both cases. Case 1. After manual debridement, visual acuity of the right eye improved to 0.63. Case 2. After manual debridement, best-corrected visual acuity of the left eye was 0.63.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Taneri S, Zieske JD, Azar DT. Evolution, techniques, clinical outcomes, and pathophysiology of LASEK: Review of the literature. Surv Ophthalmol. 2004; 49:576–602.
Article2. Camellin M. Laser epithelial keratomileusis for myopia. J Refract Surg. 2003; 19:666–70.
Article3. Claringbold TV II. Laser-assisted subepithelial keratectomy for the correction of myopia. J Cataract Refract Surg. 2002; 28:18–22.4. Brancato R, Schiavone N, Siano S, et al. Prevention of corneal keratocyte apoptosis after argon fluoride excimer laser irradia-tion with the free radical scavenger ubiquinone Q10. Eur J Ophthalmol. 2000; 10:32–8.
Article5. Wang MX, Gray TB, Park WC, et al. Reduction in corneal haze and apoptosis by amniotic membrane matrix in excimer laser photoablation in rabbits. J Cataract Refract Surg. 2001; 27:310–9.
Article6. Vinciguerra P, Camesasca FI, Ponzin D. Use of amino acids in refractive surgery. J Refract Surg. 2002; 18:374–7.
Article7. Corbett MC, O’Brart DP, Patmore AL, Marshall J. Effect of collagenase inhibitors on corneal haze after PRK. Exp Eye Res. 2001; 72:253–9.
Article8. Vetrugno M, Maino A, Cardia G, et al. A randomised, double masked, clinical trial of high dose vitamin A and vitamin E supplementation after photorefractive keratectomy. Br J Ophthalmol. 2001; 85:537–9.
Article9. Brancato R, Fiore T, Papucci L, et al. Concomitant effect of topical ubiquinone Q10 and vitamin E to prevent keratocyte apoptosis after excimer laser photoablation in rabbits. J Refract Surg. 2002; 18:135–9.
Article10. Yee RW, Yee SB. Update on laser subepithelial keratectomy (LASEK). Curr Opin Ophthalmol. 2004; 15:333–41.
Article11. Kim ES, Jin KH. Evaluation of the prophylactic use of mitomycin to inhibit haze formation after LASEK. J Korean Ophthalmol Soc. 2007; 48:623–9.12. Verweij J, Pinedo HM. Mitomycin C: mechanism of action, usefulness and limitations. Anticancer Drugs. 1990; 1:5–13.13. Xu H, Liu S, Xia X, et al. Mitomycin C reduces haze formation in rabbits after excimer laser photorefractive keratectomy. J Refract Surg. 2001; 17:342–9.
Article14. Rouweyha RM, Chuang AZ, Mitra S, et al. Laser epithelial keratomileusis for myopia with the autonomous laser. J Refract Surg. 2002; 18:217–24.
Article15. Chalita MR, Tekwani NH, Krueger RR. Laser epithelial keratomileusis: outcome of initial cases performed by an experienced surgeon. J Refract Surg. 2003; 19:412–5.
Article16. Kim JK, Kim SS, Lee HK, et al. Laser in situ keratomileusis versus laser assisted subepithelial keratectomy for the correction of high myopia. J Cataract Refract Surg. 2004; 30:1405–11.17. Baldwin HC, Marshall J. Growth factors in corneal wound healing following refractive surgery: a review. Acta Ophthalmol Scand. 2002; 80:238–47.
Article18. Nakamura K, Kurosaka D, Bissen-Miyajima H, Tsubota K. Intact corneal epithelium is essential for the prevention of stromal haze after laser assisted in situ keratomileusis. Br J Ophthalmol. 2001; 85:209–13.
Article19. Wilson SE, Mohan RR, Hong JW, et al. The wound healing response after laser in situ keratomileusis and photorefractive keratectomy; elusive control of biological variability and effect of custom laser vision correction. Arch Ophthalmol. 2001; 119:889–96.20. Kaji Y, Soya K, Amano S, et al. Relation between corneal haze and transforming growth factor-beta1 after photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 2001; 27:1840–6.21. Kuo IC, Seitz B, LaBree L, McDonnell PJ. Can zinc prevent apoptosis of anterior keratocytes after superficial keratectomy. Cornea. 1997; 16:550–5.
Article22. Corbett MC, Prydal JI, Verma S, et al. An in vivo investigation of the structures responsible for corneal haze after photorefractive keratectomy and their effect on visual function. Ophthalmology. 1996; 103:1366–80.
Article23. Moller-Pedersen T, Cavanagh HD, Petroll WM, Jester JV. Stromal wound healing explains refractive instability and haze development after photorefractive keratectomy; a 1-year confocal microscopic study. Ophthalmology. 2000; 107:1235–45.24. Pallikaris IG, Naoumidi II, Kalyvianaki MI, Katsanevaki VJ. Epi-LASIK: comparative histological evaluation of mechanical and alcohol assistedepithelial separation. J Cataract Refract Surg. 2003; 29:1496–501.25. Lin N, Yee SB, Mitra S, et al. Prediction of corneal haze using an ablation depth/corneal thickness ratio after laser epithelial keratomileusis. J Cataract Refract Surg. 2004; 20:797–802.
Article26. Cua IY, Pepose JS. Late corneal scarring after photorefractive keratectomy concurrent with the development of systemic lupus erythematosus. J Cataract Refract Surg. 2002; 18:750–2.27. Qazi MA, Johnson TW, Pepose JS. Development of late-onset subepithelial corneal haze after laser-assisted subepithelial keratectomy with prophylactic intraoperative mitomycin-C. J Cataract Refract Surg. 2006; 32:1573–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corneal Opacity Caused by LASEK with Improper High-concentrated Mitomycin-C
- Combined Mitomycin-C Assisted Photorefractive Keratectomy in the Treatment of Epithelial Ingrowth after LASIK
- Development of EKC after Eximer Laser Photorefractive Surgery and Subsequent Recurrence of EKC-like Keratitis
- Effect of Mitomycin C on Rabbit Corneal Wound Healing after Excimer Laser Photorefractive Keratectomy
- Evaluation of the Prophylactic Use of Mitomycin to Inhibit Haze Formation after LASEK