J Korean Surg Soc.
2010 Nov;79(5):332-339. 10.4174/jkss.2010.79.5.332.
Is Central Lymph Node Dissection Mandatory in 2 cm or Less Sized Papillary Thyroid Cancer?
- Affiliations
-
- 1Department of Surgery, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea. yjsuh@catholic.ac.kr
- KMID: 2212037
- DOI: http://doi.org/10.4174/jkss.2010.79.5.332
Abstract
- PURPOSE
There have been controversies on the scope of central lymph node dissection (CND) in papillary thyroid cancer (PTC). We performed this study to determine the role of CND for patients having PTC measuring 2 cm or less.
METHODS
530 cases of PTC less than 2 cm had undergone lobectomy plus isthmectomy (LI) with CND or without CND. Clinicopathologic records and clinical outcome were evaluated, retrospectively.
RESULTS
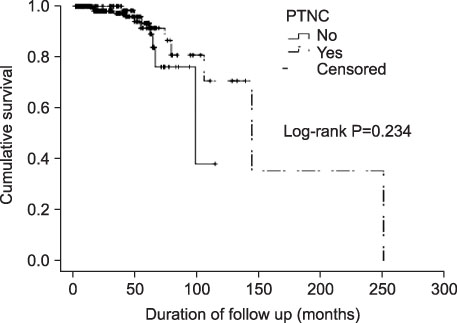
Comparing recurrence rates in LI with CND group (4/174, 2.30%) and LI without CND group (16/356, 4.49%), there was no significant statistical difference in recurrence (P=0.331). We compared 20 patients with recurrences and 510 patients of no recurrence. The size of tumor seemed to influence recurrence (P<0.001) and the size of tumor developing recurrence was larger than the other (1.11 cm vs. 0.75 cm). When considering division into PTC and papillary thyroid microcarcinoma (PTMC), PTMC showed less recurrence significantly (P=0.006). No other variables such as age, sex, tumor location, extrathyroidal extension seemed to be related to the recurrence.
CONCLUSION
We could not find any relevant role of CND to prevent recurrence either locally or regionally in cases of no lymph node metastasis after CND for patients having PTC measuring 2 cm or less. Moreover, prophylactic CND is not mandatory for all cases of PTC less than 2 cm.
Keyword
MeSH Terms
Figure
Reference
-
1. Incidence of Thyroid Cancer in 2007. Korea Central Cancer Registry; Ministry of Health, Welfare and Family Affairs. 2009. 12. 21. Korea: Available from: http://www.cancer.go.kr/cms/cancer/cancer_is/04/1191182_1753.html.2. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009. 19:1167–1214.3. Sherman SI, Angelos P, Ball DW, Byrd D, Clark OH, Daniels GH, et al. NCCN Clinical Practice Guidelines in Oncology. Thyroid Carcinoma. National Comprehensive Cancer Network 2009. National Comprehensive Cancer Network Thyroid Carcinoma Panel. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.4. Shaha AR. Implications of prognostic factors and risk groups in the management of differentiated thyroid cancer. Laryngoscope. 2004. 114:393–402.5. Caron NR, Clark OH. Papillary thyroid cancer: surgical management of lymph node metastases. Curr Treat Options Oncol. 2005. 6:311–322.6. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. American Thyroid Association Guidelines Taskforce. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2006. 16:109–142.7. Machens A, Holzhausen HJ, Dralle H. Skip metastases in thyroid cancer leaping the central lymph node compartment. Arch Surg. 2004. 139:43–45.8. Qubain SW, Nakano S, Baba M, Takao S, Aikou T. Distribution of lymph node micrometastasis in pN0 well-differentiated thyroid carcinoma. Surgery. 2002. 131:249–256.9. Scheumann GF, Gimm O, Wegener G, Hundeshagen H, Dralle H. Prognostic significance and surgical management of locoregional lymph node metastases in papillary thyroid cancer. World J Surg. 1994. 18:559–567.10. Tisell LE, Nilsson B, Mölne J, Hansson G, Fjälling M, Jansson S, et al. Improved survival of patients with papillary thyroid cancer after surgical microdissection. World J Surg. 1996. 20:854–859.11. Sywak M, Cornford L, Roach P, Stalberg P, Sidhu S, Delbridge L. Routine ipsilateral level VI lymphadenectomy reduces postoperative thyroglobulin levels in papillary thyroid cancer. Surgery. 2006. 140:1000–1005.12. Roh JL, Park JY, Park CI. Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg. 2007. 245:604–610.13. Cavicchi O, Piccin O, Caliceti U, De Cataldis A, Pasquali R, Ceroni AR. Transient hypoparathyroidism following thyroidectomy: a prospective study and multivariate analysis of 604 consecutive patients. Otolaryngol Head Neck Surg. 2007. 137:654–658.14. Lee YS, Kim SW, Kim SW, Kim SK, Kang HS, Lee ES, et al. Extent of routine central lymph node dissection with small papillary thyroid carcinoma. World J Surg. 2007. 31:1954–1959.15. Sherman SI, Angelos P, Ball DW, Byrd D, Clark OH, Daniels GH, et al. National Comprehensive Cancer Network Thyroid Carcinoma Panel. Thyroid carcinoma. J Natl Compr Canc Netw. 2007. 5:568–621.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Central Neck Lymph Node Metastasis from Papillary Thyroid Cancers
- A Clinical Review of Lymph Node Metastases for Papillary Thyroid Cancer
- Regional Lymph Node Metastasis in Papillary Thyroid Cancer
- The Pattern of Cervical Lymph Node Metastases in Papillary Thyroid Cancer
- Central Neck Dissection for Papillary Thyroid Carcinoma