J Korean Ophthalmol Soc.
2008 Apr;49(4):583-588. 10.3341/jkos.2008.49.4.583.
Correlation of Preoperative Optical Coherence Tomography with Preand Postoperative Visual Acuity of Macular Hole
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Pusan National University, Pusan, Korea. jlee@pusan.ac.kr
- KMID: 2211488
- DOI: http://doi.org/10.3341/jkos.2008.49.4.583
Abstract
-
PURPOSE: To evaluate the correlation between preoperative optical coherence tomography (OCT) parameters and pre- and post-operative visual acuity after macular hole surgery.
METHODS
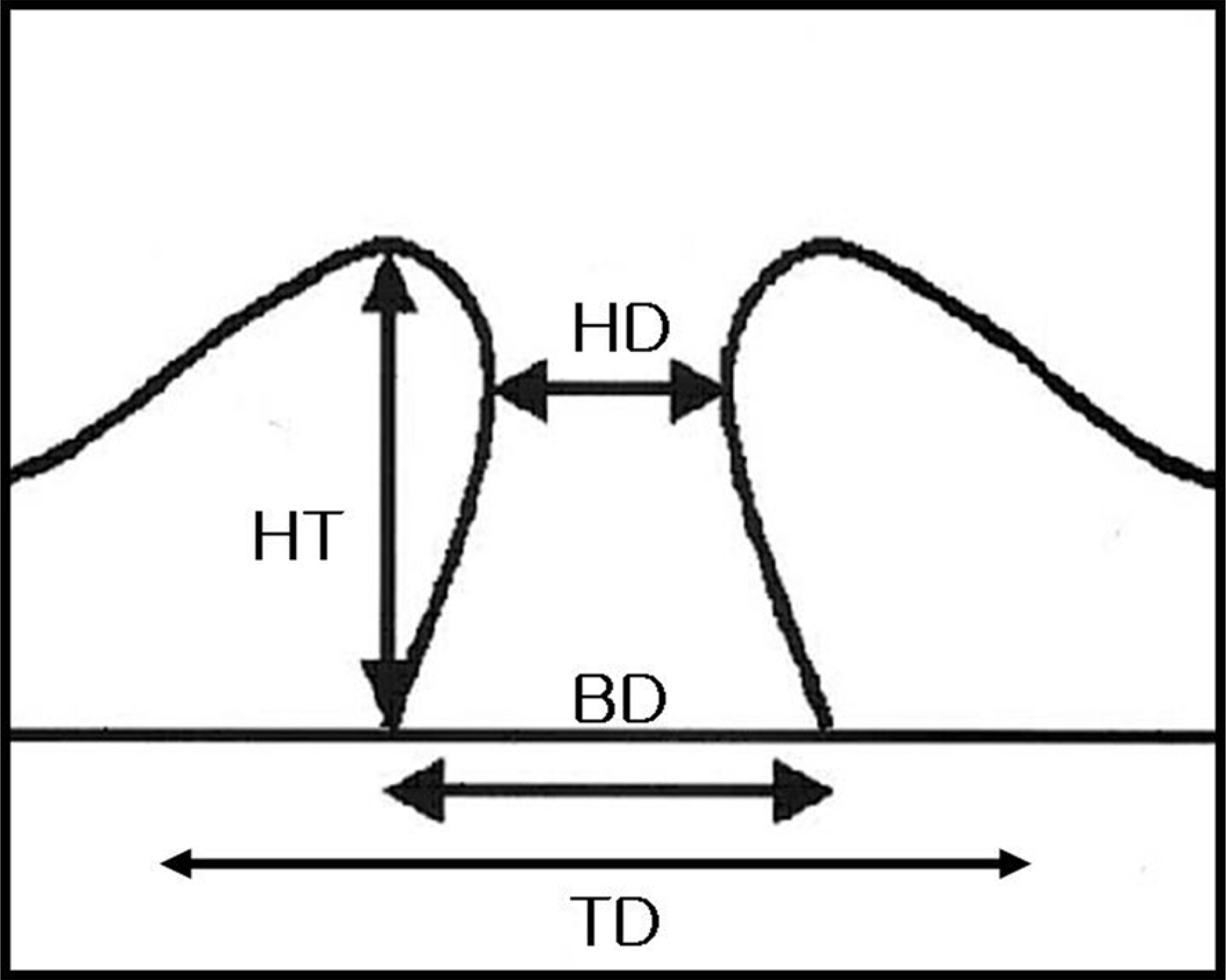
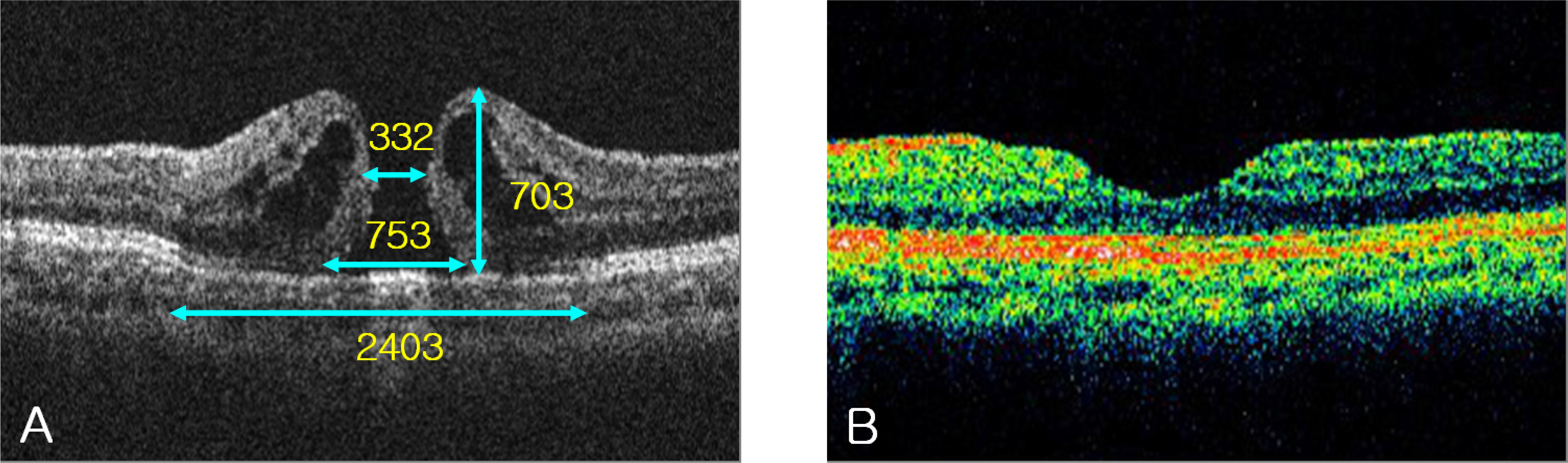
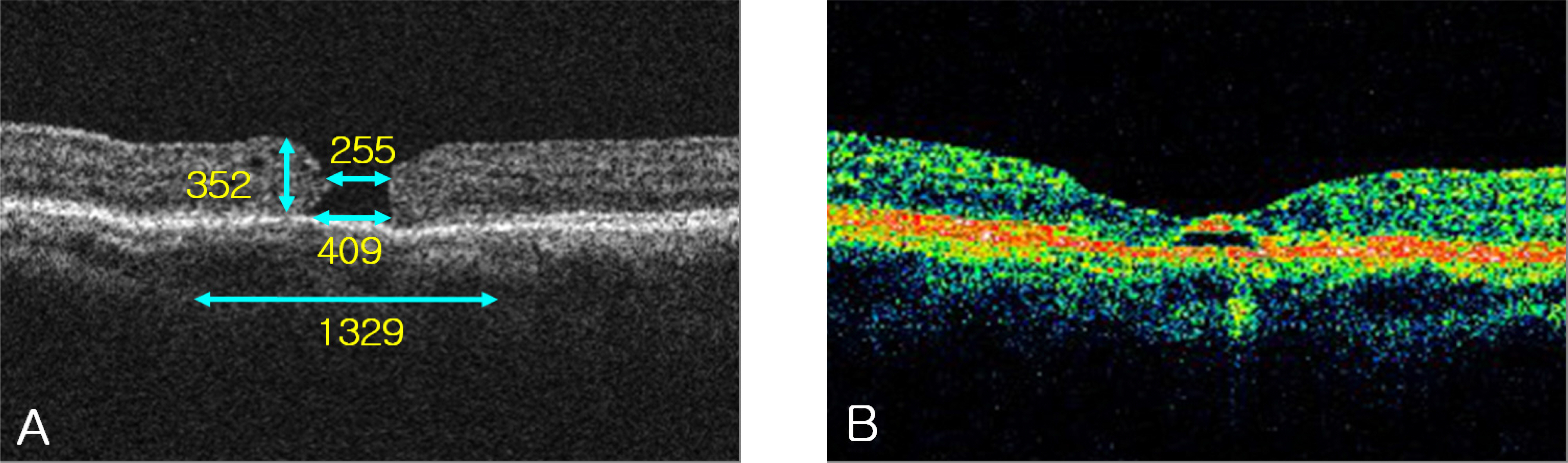
Twenty-five eyes of 24 patients who underwent macular hole surgery with a postoperative follow-up longer than 6 months were studied. On enhanced preoperative horizontal and vertical OCT scans, various parameters including hole diameter, base diameter, total lesion diameter, and hole height were measured. Hole form factor (HFF) and macular hole index (MHI) were calculated. The correlation between the parameters and pre- and post-operative visual acuity, as well as visual acuity change, was analyzed.
RESULTS
There was a significant correlation between hole height and preoperative visual acuity (P=0.018). Better postoperative visual outcome was correlated with a smaller hole diameter, smaller total lesion diameter, and greater hole height (P=0.002, 0.043 and 0.037). HFF and MHI were correlated with visual acuity change (P=0.024 and <0.001)
CONCLUSIONS
The correlation between visual acuity and hole height suggests that the height represents the amount of neural tissue in the retina. Relatively greater improvement in visual acuity is expected in eyes with high HFF or MHI even when preoperative visual acuity is low.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Gass JD. Idiopathic senile macular hole: its early stages and pathogenesis. Arch Ophthalmol. 1988; 106:629–39.
Article2. Altaweel M, Ip M. Macular hole:improved understanding of pathogenesis, staging, and management based on optical coherence tomography. Semin Ophthalmol. 2003; 18:58–66.3. Smiddy WE, Flynn HW. Pathogenesis of macular holes and therapeutic implications. Am J Ophthalmol. 2004; 137:525–37.
Article4. Puliafito CA, Hee MR, Lin CP, et al. Imaging of macular diseases with optical coherence tomography. Ophthalmology. 1995; 102:217–29.
Article5. Hee MR, Puliafito CA, Wong C, et al. Optical coherence tomography of macular holes. Ophthalmology. 1995; 102:748–56.
Article6. Ullrich S, Haritoglou C, Gass C, et al. Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol. 2002; 86:390–3.
Article7. Kusuhara S, Teraoka Escaño MF, Fujii S, et al. Prediction of postoperative visual outcome based on hole configuration by optical coherence tomography in eyes with idiopathic macular holes. Am J Ophthalmol. 2004; 138:709–16.
Article8. Lee JE, Kim EH, Oum BS. Relationship between visual acuity and photoreceptor layer or foveal thickness on optical coherence tomography after macular hole surgery. J Korean Ophthalmol Soc. 2006; 47:1966–71.9. Villate N, Lee JE, Venkatraman A, Smiddy WE. Photoreceptor layer fearues in eyes with closed macular holes: optical coherence tomography findings and correlation with visual outcomes. Am J Ophthalmol. 2005; 139:280–9.10. Takahashi H, Kishi S. Tomographic fearues of a lamellar macular hole formation and a lamellar hole that progressed to a full‐ thickness macular hole. Am J Ophthalmol. 2000; 130:677–9.11. Gaudric A, Haouchine B, Massin P. Macular hole formation: new data provided by optical coherence tomography. Arch Opthalmol. 1999; 117:744–51.12. Sjaarda RN, Frank DA, Glaser BM, et al. Resolution of an absolute scotoma and improvement of relative scotoma after successful macular hole surgery. Am J Ophthalmol. 1993; 116:129–39.13. Seo MS, Kang SJ. Prognostic factors in idiopathic macular hole surgery. J Korean Ophthalmol Soc. 2000; 41:1746–52.14. Kim KS, Kim YC. Surgical results of vitrectomy for macular holes, according to the hole size. J Korean Ophthalmol Soc. 2006; 47:927–32.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-Term Visual Outcomes and Prognostic Factors for Successful Idiopathic Macular Hole
- The Evaluation of Prognostic Factors after Vitrectomy for Idiopathic Macular Hole with OCT
- The Evaluation of Prognostic Factors after Vitrectomy for Lamellar Macular Hole Using Optical Coherence Tomography
- The Spontaneous Resolution of Idiopathic Macular Hole Diagnosed with OCT
- Reorganization of Photoreceptor Layer on Optical Coherence Tomography Concurrent with Visual Improvement after Macular Hole Surgery