J Korean Soc Magn Reson Med.
2010 Dec;14(2):95-102. 10.13104/jksmrm.2010.14.2.95.
MRI Findings of Triple Negative Breast Cancer: A Comparison with Non-Triple Negative Breast Cancer
- Affiliations
-
- 1Department of Radiology, College of Medicine, The Catholic University of Korea, Korea. rad-ksh@catholic.ac.kr
- 2Clinical Research Coordinating Center, College of Medicine, The Catholic Medical Center, Korea.
- 3Department of Surgery, College of Medicine, The Catholic University of Korea, Korea.
- KMID: 2206906
- DOI: http://doi.org/10.13104/jksmrm.2010.14.2.95
Abstract
- PURPOSE
To evaluate the magnetic resonance imaging (MRI) and clinicopathological features of triple negative breast cancer, and compare them with those of non-triple negative breast cancer.
MATERIALS AND METHODS
This study included 231 pathologically confirmed breast cancers from January 2007 to May 2008. We retrospectively reviewed the MRI findings according to the Breast Imaging Reporting and Data System (BI-RADS) lexicon: mass or non-mass type, mass shape, mass margin, non-mass distribution, and enhancement pattern. Histologic type, histologic grade, and the results for epidermal growth factor receptor, p53, and Ki 67 were reviewed.
RESULTS
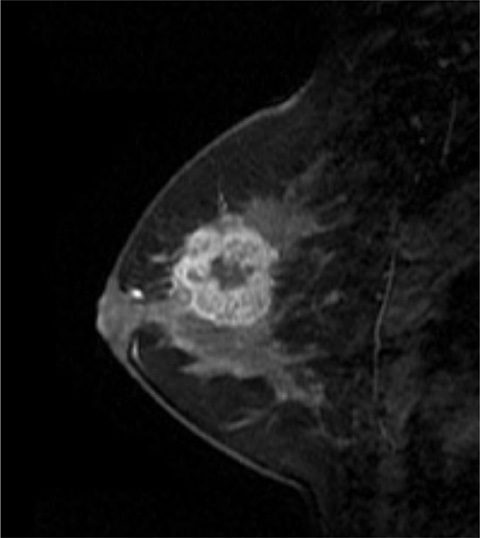
Of 231 patients, 43(18.6%) were triple negative breast cancer. Forty triple negative breast cancers (93.0%) were mass-type lesion on MRI. A round or oval or lobular shape (p=0.006) and rim enhancement (p=0.004) were significantly more in triple negative breast cancer than non-triple negative breast cancer. In contrast, irregular shape (p=0.006) and spiculated margins (p=0.032) were significantly more in non-triple negative breast cancer. Old age (p=0.019), high histologic grade (p<0.0001), EGFR positivity (p<0.0001), p53 overexpression (p=0.038), and Ki 67 expression (<0.0001) were significantly associated with the triple negative breast cancer.
CONCLUSION
MRI finding may be helpful for differentiation between triple negative and non-triple negative breast cancer.
Keyword
MeSH Terms
Figure
Reference
-
1. Reis-Filho JS, Tutt AN. Triple negative tumours: a critical review. Histopathology. 2008. 52:108–118.2. Iwase H, Kurebayashi J, Tsuda H, et al. Clinicopathological analyses of triple negative breast cancer using surveillance data from the Registration Committee of the Japanese Breast Cancer Society. Breast Cancer. 17:118–124.3. Dent R, Trudeau M, Pritchard KI, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007. 13:4429–4434.4. Trivers KF, Lund MJ, Porter PL, et al. The epidemiology of triple-negative breast cancer, includ ing race. Cancer Causes Control. 2009. 20:1071–1082.5. Uematsu T, Kasami M, Yuen S. Triple-negative breast cancer: correlation between MR imaging and pathologic findings. Radiology. 2009. 250:638–647.6. Chen JH, Agrawal G, Feig B, et al. Triple-negative breast cancer: MRI features in 29 patients. Ann Oncol. 2007. 18:2042–2043.7. Yang WT, Dryden M, Broglio K, et al. Mammographic features of triple receptor-negative primary breast cancers in young premenopausal women. Breast Cancer Res Treat. 2008. 111:405–410.8. Facius M, Renz DM, Neubauer H, et al. Characteristics of ductal carcinoma in situ in magnetic resonance imaging. Clin Imaging. 2007. 31:394–400.9. Rosen EL, Smith-Foley SA, DeMartini WB, Eby PR, Peacock SLehman CD. BI-RADS MRI enhancement characteristics of ductal carcinoma in situ. Breast J. 2007. 13:545–550.10. Weigelt B, Kreike B, Reis-Filho JS. Metaplastic breast carcinomas are basal-like breast cancers: a genomic profiling analysis. Breast Cancer Res Treat. 2009. 117:273–280.11. Reis-Filho JS, Milanezi F, Steele D, et al. Metaplastic breast carcinomas are basal-like tumours. Histopathology. 2006. 49:10–21.12. Leibl S, Moinfar F. Metaplastic breast carcinomas are negative for Her-2 but frequently express EGFR (Her-1): potential relevance to adjuvant treatment with EGFR tyrosine kinase inhibitors? J Clin Pathol. 2005. 58:700–704.13. Reis-Filho JS, Milanezi F, Carvalho S, et al. Metaplastic breast carcinomas exhibit EGFR, but not HER2, gene amplification and overexpression: immunohistochemical and chromogenic in situ hybridization analysis. Breast Cancer Res. 2005. 7:R1028–R1035.14. Kuroda N, Fujishima N, Inoue K, et al. Basal-like carcinoma of the breast: further evidence of the possibility that most metaplastic carcinomas may be actually basal-like carcinomas. Med Mol Morphol. 2008. 41:117–120.15. Sasaki Y, Tsuda H. Clinicopathological characteristics of triple-negative breast cancers. Breast Cancer. 2009. 16:254–259.16. Corkery B, Crown J, Clynes M, O'Donovan N. Epidermal growth factor receptor as a potential therapeutic target in triple-negative breast cancer. Ann Oncol. 2009. 20:862–867.17. Rolland P, Spendlove I, Madjd Z, et al. The p53 positive Bcl-2 negative phenotype is an independent marker of prognosis in breast cancer. Int J Cancer. 2007. 120:1311–1317.18. Viale G, Rotmensz N, Maisonneuve P, et al. Invasive ductal carcinoma of the breast with the "triple-negative" phenotype: prognostic implications of EGFR immunoreactivity. Breast Cancer Res Treat. 2009. 116:317–328.19. Biswas DK, Iglehart JD. Linkage between EGFR family receptors and nuclear factor kappaB (NF-kappaB) signaling in breast cancer. J Cell Physiol. 2006. 209:645–652.20. Nogi H, Kobayashi T, Suzuki M, et al. EGFR as paradoxical predictor of chemosensitivity and outcome among triple-negative breast cancer. Oncol Rep. 2009. 21:413–417.21. Chae BJ, Bae JS, Lee A, et al. p53 as a specific prognostic factor in triple-negative breast cancer. Jpn J Clin Oncol. 2009. 39:217–224.22. Yamamoto Y, Ibusuki M, Nakano M, Kawasoe T, Hiki R, Iwase H. Clinical significance of basal-like subtype in triple-negative breast cancer. Breast Cancer. 2009. 16:260–267.23. Viale G, Regan MM, Mastropasqua MG, et al. Predictive value of tumor Ki-67 expression in two randomized trials of adjuvant chemoendocrine therapy for node-negative breast cancer. J Natl Cancer Inst. 2008. 100:207–212.24. Ding SL, Sheu LF, Yu JC, et al. Expression of estrogen receptor-alpha and Ki67 in relation to pathological and molecular features in early-onset infiltrating ductal carcinoma. J Biomed Sci. 2004. 11:911–919.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinicopathologic Characteristics and Prognosis of Early Stage Triple Negative Breast Cancer: Comparison with Non-triple Negative Group
- Fear of Cancer Recurrence and Unmet Needs in Triple Negative Breast Cancer Survivors
- Comment on “Histomorphological Factors Predicting the Response to Neoadjuvant Chemotherapy in Triple-Negative Breast Cancerâ€
- Bilateral Triple-Negative Invasive Breast Cancer with a BRCA2 Mutation, and Glioblastoma: A Case Report and Literature Review
- Comment to “Patients with Concordant Triple-Negative Phenotype between Primary Breast Cancers and Corresponding Metastases Have Poor Prognosisâ€