J Korean Med Assoc.
2015 Sep;58(9):786-794. 10.5124/jkma.2015.58.9.786.
Prevention and treatment of pressure ulcers
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. lionheo@snu.ac.kr
- KMID: 2195090
- DOI: http://doi.org/10.5124/jkma.2015.58.9.786
Abstract
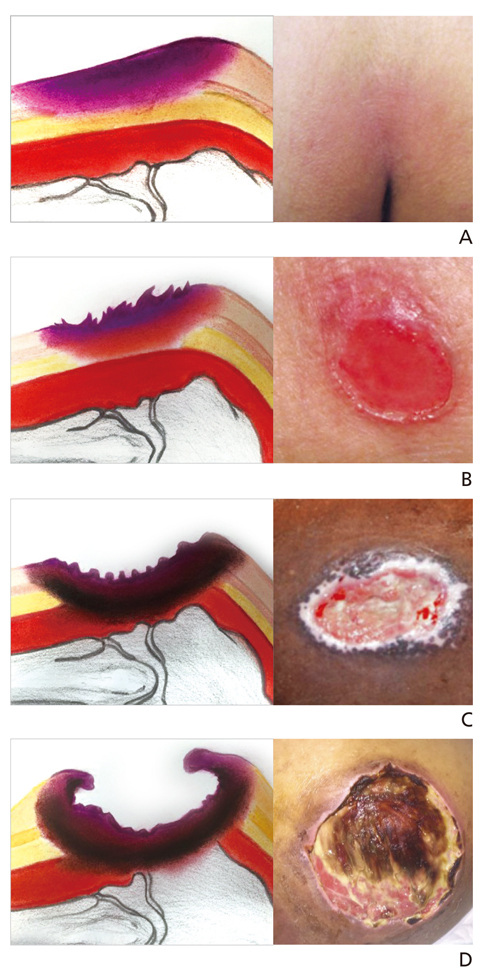
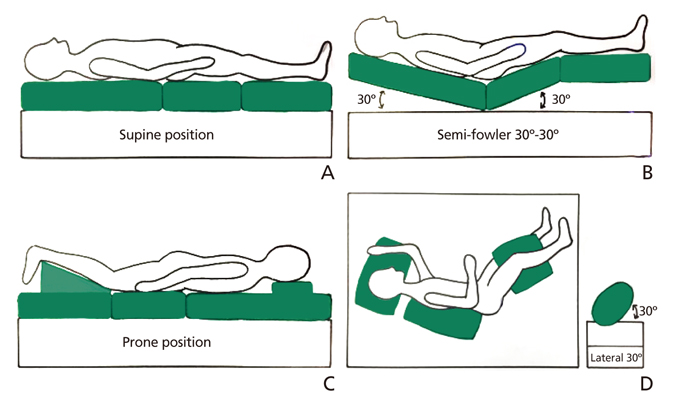
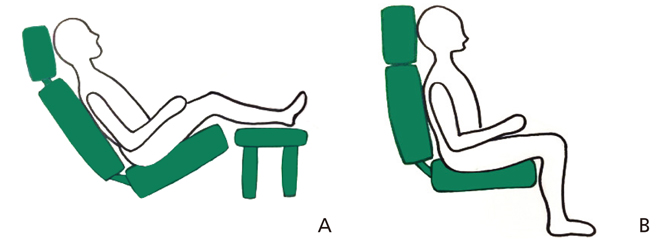
- Repeated or chronic pressure on the eminent part of the body will cause circulation disorder to the affected part of the body. The lack of circulation will result in damage and necrosis of the tissue. This phenomenon is defined as pressure sore. Due to growth of aging population and chronic disease, incidence and prevalence rate is in-creasing rapidly. This leads to increased duration of hospital stay, and medical expenditure. Hence, prevention of pressure sore and appropriate treatment is essential in order to diminish distress of the patient and health care provider. Prevention of pressure sore can be accomplished by frequent position change of the patient, skin care, and appropriate nutrition care. Frequent position change is known to be the most important and effective method to prevent pressure sore. Skin care can be achieved by choosing proper dressing material, management of exu-date, and protection of the tissue around the wound. In addition, appropriate nutrition care in order to correct protein-calorie imbalance should also be performed. Necrotic tissue can cause inflammation, and it can also be a good source of bacterial growth. Therefore, debridement of necrotic tissue is most fundamental and essential part in the treatment of pressure sore. Meanwhile, when the patient is not a candidate for surgical treatment due to poor general condition, many methods of dressing can be performed. Recently, dressing material with silver component, and vacuum assisted closure dressing is being performed frequently. In case of surgical treatment, after debridement of necrotic tissue, reconstruction can be performed by split-thickness skin grafting, full-thickness skin grafting, or primary closure. However, majority of reconstruction is performed by flap surgery. Rotation or advancement flap is usually performed.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Chronic wound
Jong Won Rhie
J Korean Med Assoc. 2015;58(9):784-785. doi: 10.5124/jkma.2015.58.9.784.
Reference
-
1. Kim JY, Heo CY, Minn KW. Clinical application of maggots in pressure ulcer. J Korean Wound Care Soc. 2007; 3:78–82.2. Oh KS, Lim SY, Mun GH, Hyon WS, Bang SI. The treatment of pressure sore. J Korean Wound Care Soc. 2005; 1:83–86.3. Kwon H, Jang IS, Lee JK, Lim P. Clinical observation of the pressure ulcer. J Korean Soc Plast Reconstr Surg. 1996; 23:818–826.4. Qaseem A, Mir TP, Starkey M, Denberg TD. Clinical Guide-lines Committee of the American College of Physicians. Risk assessment and prevention of pressure ulcers: a clinical practice guideline from the Ameri-can College of Physicians. Ann Intern Med. 2015; 162:359–369.
Article5. Kim KR. Nutrition management for pressure sore. J Korean Wound Manage Soc. 2010; 6:33–36.6. Park MS. The influence of aging on wound healing and risk fac-tors of pressure ulcer in the elderly. J Korean Wound Manage Soc. 2008; 4:88–91.7. Park KH. Dressing for pressure ulcers. J Korean Wound Manage Soc. 2008; 4:24–27.8. Lee KC, Moon JB, Kwon YS, Cha BH, Kim SK. Clinical con-siderations of the surgical treatments of the pressure sore. J Korean Soc Plast Reconstr Surg. 2007; 34:574–579.