J Korean Med Assoc.
2014 Aug;57(8):695-703. 10.5124/jkma.2014.57.8.695.
Concept of perforator flap and reconstruction using microsurgery
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Hanyang University, School of Medicine, Seoul, Korea.
- 2Department of Plastic and Reconstructive Surgery, The Catholic University of Korea College of Medicine, Seoul, Korea. sw1215@catholic.ac.kr
- KMID: 2194920
- DOI: http://doi.org/10.5124/jkma.2014.57.8.695
Abstract
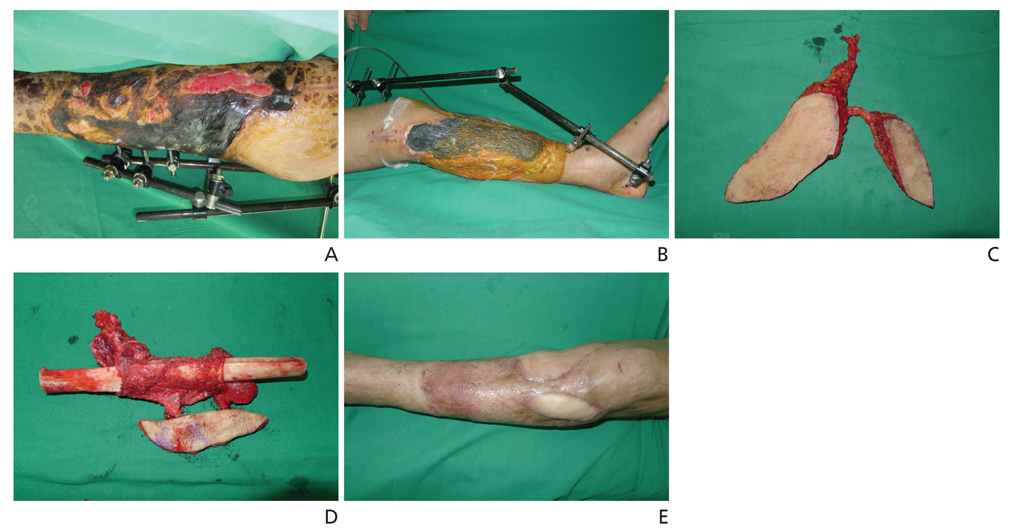
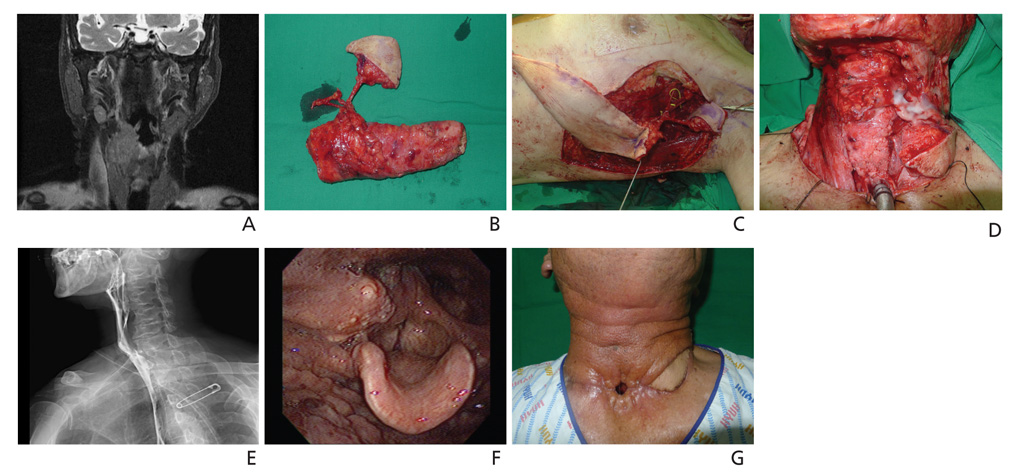
- Free tissue transfer has revolutionized tissue reconstruction. Microvascular operation techniques using free tissue transfer make it possible to precisely restore various defects and deformities. There are various surgical flaps available for this surgery, such as muscle flaps, musculocutaneous flaps, or fasciocutaneous flaps. The development of perforator flaps enables multi-component reconstruction with reduced donor site morbidity. Successful reconstruction must be approached with the goals of not only providing stable coverage, but most importantly, of restoring function. Therefore, the selection of flaps is dependent on the recipient site characteristics and the functional and aesthetic results at both the recipient and donor sites. With the high success rate of free flaps and the popularization of the perforator flap, microvascular surgery has played a major role in various reconstructive fields.
MeSH Terms
Figure
Reference
-
1. Murphy JB. Resection of arteries and veins injured in continuity-end-to-end of suture-experimental and clinical research. Med Rec. 1897; 51:73–88.2. Carrel A. The operative technique of vascular anastomoses and the transplantation of viscera. Clin Orthop Relat Res. 1963; 29:3–6.3. Jacobson JH, Suarez EL. Microsurgery in anastomosis of small vessels. Surg Forum. 1960; 11:243–245.4. Daniel RK, Taylor GI. Distant transfer of an island flap by microvascular anastomoses: a clinical technique. Plast Reconstr Surg. 1973; 52:111–117.5. O'Brien BM, MacLeod AM, Hayhurst JW, Morrison WA. Successful transfer of a large island flap from the groin to the foot by microvascular anastomoses. Plast Reconstr Surg. 1973; 52:271–278.6. Chung CN. Clinical observation on skin graft and flap. J Korean Soc Plast Reconstr Surg. 1974; 1:23–39.7. Lim P, Cho MJ, Cho HS, Hur E, Lee JW, Ham KS. An axillary scar contracture corrected by microvascular free groin flap transfer. J Korean Soc Plast Reconstr Surg. 1978; 5:189–194.8. Orticochea M. The musculo-cutaneous flap method: an immediate and heroic substitute for the method of delay. Br J Plast Surg. 1972; 25:106–110.
Article9. Ponten B. The fasciocutaneous flap: its use in soft tissue defects of the lower leg. Br J Plast Surg. 1981; 34:215–220.
Article10. Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg. 1989; 42:645–648.
Article11. Kim JT. Latissimus dorsi perforator flap. Clin Plast Surg. 2003; 30:403–431.
Article12. Kim JT. Two options for perforator flaps in the flank donor site: latissimus dorsi and thoracodorsal perforator flaps. Plast Reconstr Surg. 2005; 115:755–763.
Article13. Armstrong MB, Masri N, Venugopal R. Reconstructive microsurgery: reviewing the past, anticipating the future. Clin Plast Surg. 2001; 28:671–686.14. Saint-Cyr M, Wong C, Buchel EW, Colohan S, Pederson WC. Free tissue transfers and replantation. Plast Reconstr Surg. 2012; 130:858e–878e.
Article15. Kang MJ, Chung CH, Chang YJ, Kim KH. Reconstruction of the lower extremity using free flaps. Arch Plast Surg. 2013; 40:575–583.
Article16. Han DH, Park MC, Park DH, Song H, Lee IJ. Role of muscle free flap in the salvage of complicated scalp wounds and infected prosthetic dura. Arch Plast Surg. 2013; 40:735–741.
Article17. Genden EM, Rinaldo A, Suarez C, Wei WI, Bradley PJ, Ferlito A. Complications of free flap transfers for head and neck reconstruction following cancer resection. Oral Oncol. 2004; 40:979–984.
Article18. Mun GH, Kim HJ, Cha MK, Kim WY. Impact of perforator mapping using multidetector-row computed tomographic angiography on free thoracodorsal artery perforator flap transfer. Plast Reconstr Surg. 2008; 122:1079–1088.
Article19. Park CW, Kim YH, Hwang KT, Kim JT. Reconstruction of a severely crushed leg with interpositional vessel grafts and latissimus dorsi flap. Arch Plast Surg. 2012; 39:417–421.
Article20. Breidenbach WC 3rd. Emergency free tissue transfer for reconstruction of acute upper extremity wounds. Clin Plast Surg. 1989; 16:505–514.
Article21. Park JH, Min KH, Eun SC, Lee JH, Hong SH, Kim CW. Scalp free flap reconstruction using anterolateral thigh flap pedicle for interposition artery and vein grafts. Arch Plast Surg. 2012; 39:55–58.
Article22. Kimata Y, Uchiyama K, Ebihara S, Yoshizumi T, Asai M, Saikawa M, Hayashi R, Jitsuiki Y, Majima K, Ohyama W, Haneda T, Nakatsuka T, Harii K. Versatility of the free anterolateral thigh flap for reconstruction of head and neck defects. Arch Otolaryngol Head Neck Surg. 1997; 123:1325–1331.
Article23. Koshima I, Yamamoto H, Hosoda M, Moriguchi T, Orita Y, Nagayama H. Free combined composite flaps using the lateral circumflex femoral system for repair of massive defects of the head and neck regions: an introduction to the chimeric flap principle. Plast Reconstr Surg. 1993; 92:411–420.
Article24. Grover R, Nelson JA, Fischer JP, Kovach SJ, Serletti JM, Wu LC. The impact of perforator number on deep inferior epigastric perforator flap breast reconstruction. Arch Plast Surg. 2014; 41:63–70.
Article25. Healy C, Ramakrishnan V. Autologous microvascular breast reconstruction. Arch Plast Surg. 2013; 40:3–10.
Article26. Huang WC, Chen HC, Wei FC, Cheng MH, Schnur DP. Chimeric flap in clinical use. Clin Plast Surg. 2003; 30:457–467.
Article27. Coleman JJ 3rd, Tan KC, Searles JM, Hester TR, Nahai F. Jejunal free autograft: analysis of complications and their resolution. Plast Reconstr Surg. 1989; 84:589–595.28. Sardesai MG, Fung K, Yoo JH, Bakker H. Donor-site morbidity following radial forearm free tissue transfer in head and neck surgery. J Otolaryngol Head Neck Surg. 2008; 37:411–416.29. Bae SK, Kang SJ, Kim JW, Kim YH, Sun H. Reconstruction of abdominal wall of a chronically infected postoperative wound with a rectus abdominis myofascial splitting flap. Arch Plast Surg. 2013; 40:28–35.
Article30. Jung JA, Kim YW, Kang SR. Reconstruction of unexpected huge chest wall defect after recurrent breast cancer excision using a TRAM flap combined with partial latissimus dorsi muscle flap. Arch Plast Surg. 2013; 40:76–79.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contribution of Perforator Flaps in the Flap Selection for Head and Neck Reconstruction
- Soft Tissue Coverage Using a Combined Gastrocnemius-medial Sural Artery Perforator Flap
- Perforator Flap versus Conventional Flap
- Reconstruction of the Three-Dimensional Mandibulofacial Defects Using a Single Cutaneous Perforator-Based Fibula Osteocutaneous Flap
- Digital Artery Perforator Flaps