J Korean Med Assoc.
2014 Aug;57(8):653-660. 10.5124/jkma.2014.57.8.653.
Differential diagnosis of common shoulder pain
- Affiliations
-
- 1Department of Rehabilitation Medicine, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea. hjrhee1@dumc.or.kr
- KMID: 2194915
- DOI: http://doi.org/10.5124/jkma.2014.57.8.653
Abstract
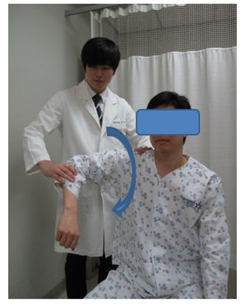
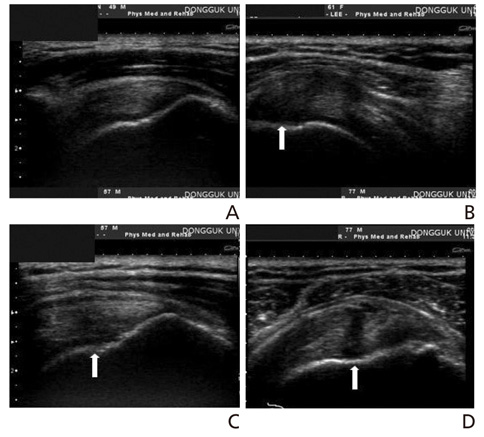
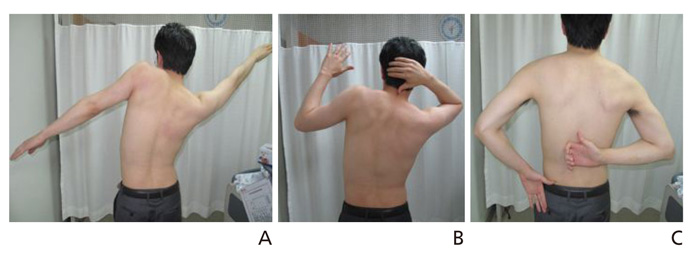
- Shoulder pain is a common problem in outpatient medical practice. Shoulder pain usually causes disability in activities of daily living, and therefore its proper diagnosis and management are essential. The prevalence of shoulder pain in Korea has been gradually increasing, and the differential diagnosis of shoulder pain has become more important. In Korea, the most common causes of shoulder pain are rotator cuff disease, including impingement syndrome (31%), adhesive capsulitis (35%), and calcific tendinitis (4%). This article presents the pathophysiology, clinical characteristics, typical physical examination findings and provocation tests, and radiologic findings of common shoulder diseases, including rotator cuff disease, adhesive capsulitis, and calcific tendinitis, to provide a guide to differential diagnosis. Common shoulder diseases can be easily diagnosed with careful history taking and precise physical examination; moreover, ultrasonography is a useful diagnostic tool for rotator cuff disease and can also assist with the differential diagnosis of shoulder diseases in the outpatient clinic.
MeSH Terms
Figure
Cited by 1 articles
-
Diagnosis and non-operative treatment of shoulder pain
Shi-Uk Lee
J Korean Med Assoc. 2019;62(12):629-635. doi: 10.5124/jkma.2019.62.12.629.
Reference
-
1. Shanahan EM, Sladek R. Shoulder pain at the workplace. Best Pract Res Clin Rheumatol. 2011; 25:59–68.
Article2. National Health Insurance Service. Press release [Internet]. Seoul: National Health Insurance Service;2012. cited 2014 Jun 17. Available from: http://www.nhis.or.kr/portal/site/main/MENU_WBDCC01/.3. Seo KM, Chung SG. Upper extremity pain. In : Han TR, Bang MS, Chung SG, editors. Rehabilitation medicine. 5th ed. Seoul: Koonja Publishing;2014. p. 1032–1055.4. Greenberg DL. Evaluation and treatment of shoulder pain. Med Clin North Am. 2014; 98:487–504.
Article5. Speed C. Shoulder pain. Clin Evid. 2005; 14:1543–1560.6. Lewis JS. Rotator cuff tendinopathy. Br J Sports Med. 2009; 43:236–241.
Article7. Lee SU. Rotator cuff disease: pathology, pathophysiology, and natural course. J Korean Assoc Pain Med. 2007; 6:59–65.8. Factor D, Dale B. Current concepts of rotator cuff tendinopathy. Int J Sports Phys Ther. 2014; 9:274–288.9. Seitz AL, McClure PW, Finucane S, Boardman ND 3rd, Michener LA. Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both? Clin Biomech (Bristol, Avon). 2011; 26:1–12.
Article10. Neer CS 2nd. Impingement lesions. Clin Orthop Relat Res. 1983; 173:70–77.
Article11. Park JY, Choi JH. Treatment of pain around the shoulder joint. J Korean Med Assoc. 2005; 48:1206–1214.
Article12. Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012; 31:589–604.
Article13. Kibler WB, Murrell GA, Pluim B. Shoulder pain. In : Brunker P, Khan K, editors. Brukner & Khan's clinical sports medicine. 4th ed. New York: McGraw-Hill;2012. p. 353–376.14. Hattrup SJ, Cofield RH. Rotator cuff tears with cervical radiculopathy. J Shoulder Elbow Surg. 2010; 19:937–943.
Article15. Codsi M, McCarron J, Brems JJ. Clinical evaluation of shoulder problems. In : Rockwood CA, editor. The shoulder. 4th ed. Philadelphia: Saunders Elsevier;2009. p. 162–168.16. Jain NB, Wilcox RB 3rd, Katz JN, Higgins LD. Clinical examination of the rotator cuff. PM R. 2013; 5:45–56.
Article17. Hegedus EJ, Goode AP, Cook CE, Michener L, Myer CA, Myer DM, Wright AA. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med. 2012; 46:964–978.
Article18. Nazarian LN, Jacobson JA, Benson CB, Bancroft LW, Bedi A, McShane JM, Miller TT, Parker L, Smith J, Steinbach LS, Teefey SA, Thiele RG, Tuite MJ, Wise JN, Yamaguchi K. Imaging algorithms for evaluating suspected rotator cuff disease: Society of Radiologists in Ultrasound consensus conference statement. Radiology. 2013; 267:589–595.
Article19. Lenza M, Buchbinder R, Takwoingi Y, Johnston RV, Hanchard NC, Faloppa F. Magnetic resonance imaging, magnetic re-sonance arthrography and ultrasonography for assessing ro-tator cuff tears in people with shoulder pain for whom sur-gery is being considered. Cochrane Database Syst Rev. 2013; 9:CD009020.
Article20. Park GY. Diagnosis and rehabilitation treatment in adhesive capsulitis of the shoulder. J Korean Med Assoc. 2004; 47:1099–1106.
Article21. Robinson CM, Seah KT, Chee YH, Hindle P, Murray IR. Fro-zen shoulder. J Bone Joint Surg Br. 2012; 94:1–9.
Article22. Neviaser AS, Neviaser RJ. Adhesive capsulitis of the shoulder. J Am Acad Orthop Surg. 2011; 19:536–542.
Article23. Hannafin JA, Chiaia TA. Adhesive capsulitis. A treatment approach. Clin Orthop Relat Res. 2000; 372:95–109.24. Neviaser AS, Hannafin JA. Adhesive capsulitis: a review of current treatment. Am J Sports Med. 2010; 38:2346–2356.25. Siegal DS, Wu JS, Newman JS, Del Cura JL, Hochman MG. Calcific tendinitis: a pictorial review. Can Assoc Radiol J. 2009; 60:263–272.
Article26. Bureau NJ. Calcific tendinopathy of the shoulder. Semin Musculoskelet Radio. 2013; 17:80–84.
Article