J Korean Soc Surg Hand.
2013 Sep;18(3):124-131. 10.12790/jkssh.2013.18.3.124.
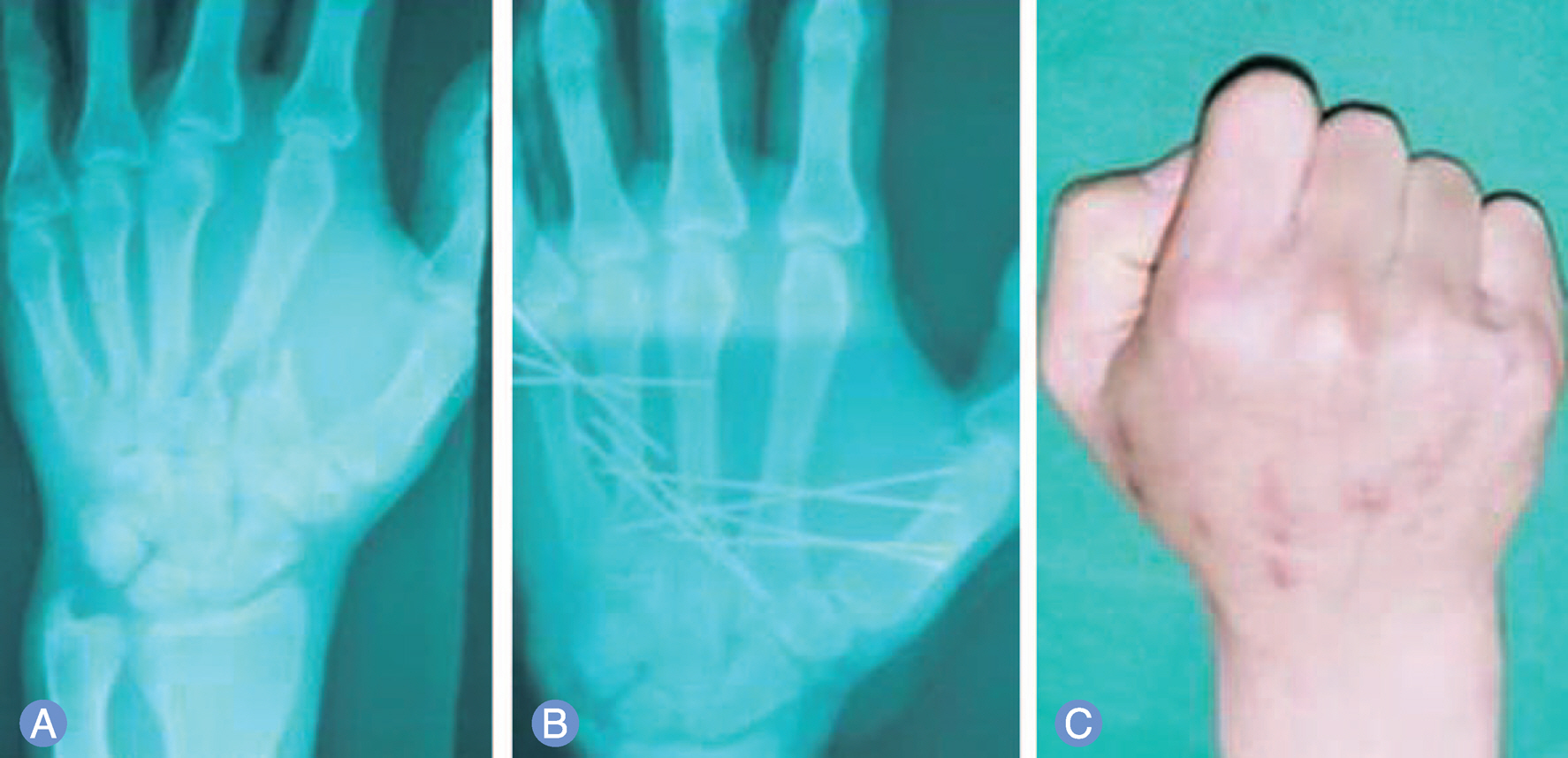
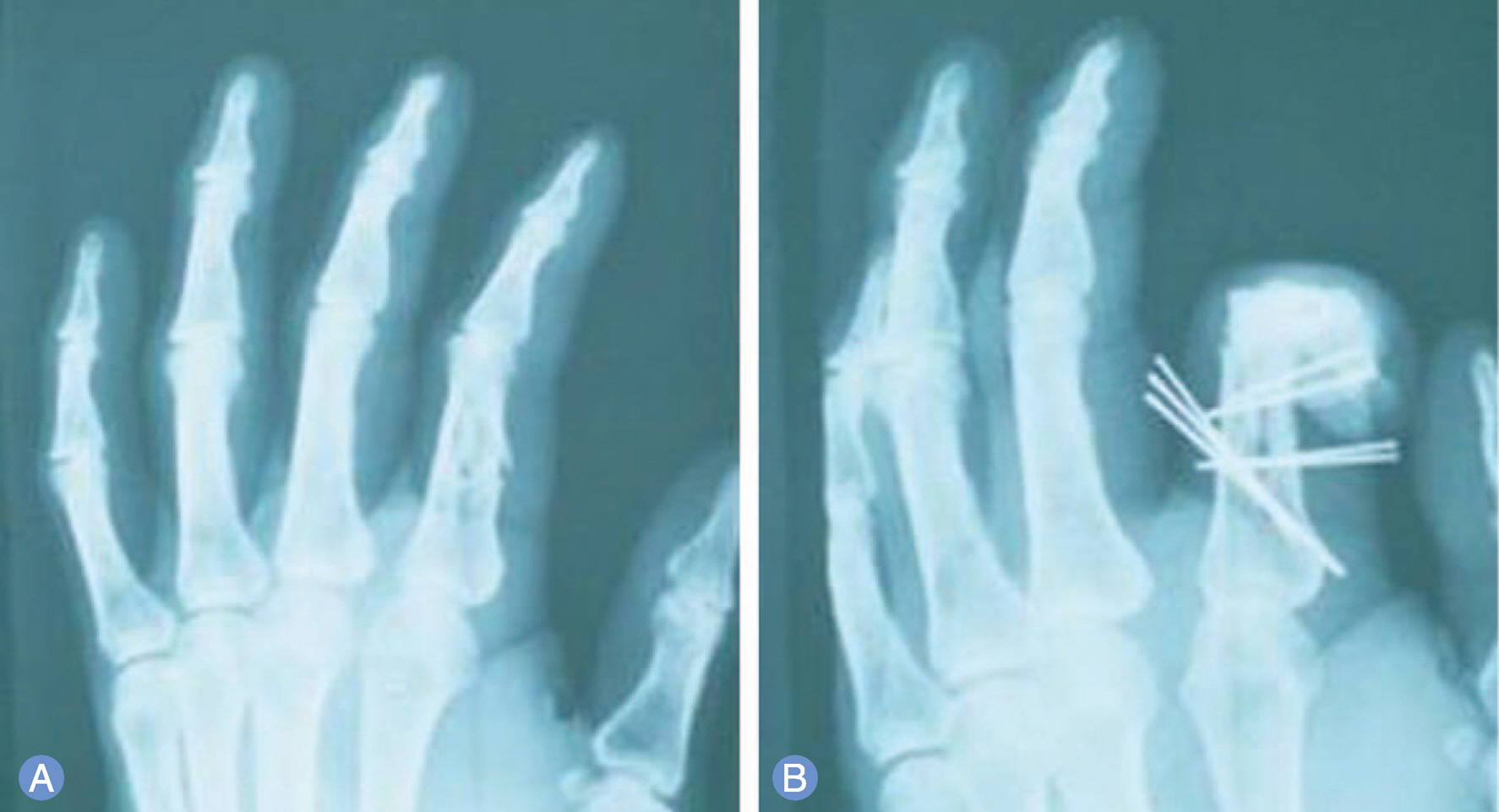
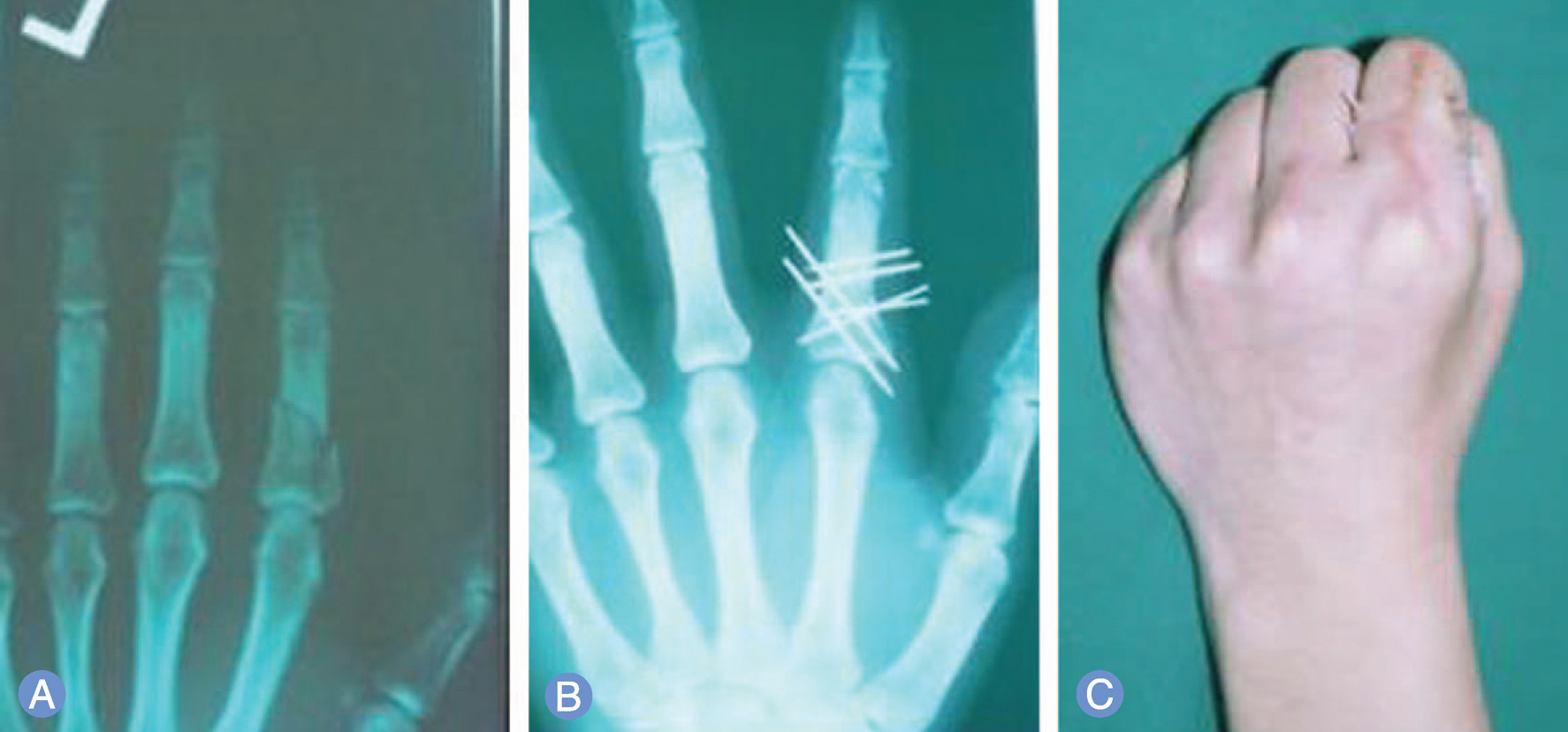
Percutaneous Multiple Kirschner Wire Fixation in the Treatment of Hand Fractures
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Dongguk University Ilsan Hospital, Goyang, Korea.
- 2Department of Plastic and Reconstructive Surgery, Duson Hospital, Ansan, Korea. blueginget@google.com
- KMID: 2194142
- DOI: http://doi.org/10.12790/jkssh.2013.18.3.124
Abstract
- PURPOSE
We reported results of percutaneous multiple K-wire fixation technique without passing through the joint in patients with a hand fracture.
METHODS
We evaluated a total of 116 cases in 94 patients who underwent percutaneous multiple K-wire fixation on dorsal cortex over a 10-year period between 2001 and 2010. The treatment outcomes were evaluated based on total active motion (TAM), as proposed by Widegrow.
RESULTS
Our clinical series of patients achieved good functional outcomes. Of total patients, 89% (84/94) had excellent TAM, 2% (2/94) did good TAM and 9% (8/94) did poor TAM. Postoperatively, our clinical series of patients had such a good compliance as to achieve a TAM of >181degrees when performing the early active movement. There were no notable postoperative complications during the follow-up period.
CONCLUSION
Our results indicate that percutaneous multiple K-wire fixation technique without passing through the joint from normal bone density patients is effective in providing the rigid fixation. Thus, our patients could perform the early movement as promptly as possible and maintaining the full mobility of the rest of the hand.
Keyword
MeSH Terms
Figure
Reference
-
1. Green DP, Rowland SP. Fractures and dislocations in the hand. Rockwood CA, Green DP, editors. Fractures in adults. 3rd ed.Philadelphia, PA: Lippincott Williams & Wilkins;1975. p. 265–344.2. Emmett JE, Breck LW. A review and analysis of 11,000 fractures seen in a private practice of orthopaedic surgery, 1937-1956. J Bone Joint Surg Am. 1958; 40:1169–75.
Article3. Brown PW. The management of phalangeal and metacarpal fractures. Surg Clin North Am. 1973; 53:1393–437.
Article4. Jupiter JB, Koniuch MP, Smith RJ. The management of delayed union and nonunion of the metacarpals and phalanges. J Hand Surg Am. 1985; 10:457–66.
Article5. Wright TA. Early mobilization in fractures of the metacarpals and phalanges. Can J Surg. 1968; 11:491–8.6. Widgerow AD, Edinburg M, Biddulph SL. An analysis of proximal phalangeal fractures. J Hand Surg Am. 1987; 12:134–9.
Article7. Watson-Jones R. Fractures and joint injuries. 4th ed. London: E.&S. Livingstone;1955.8. Swanson AB. Fractures involving the digits of the hand. Orthop Clin North Am. 1970; 1:261–74.
Article9. Stern PJ. Management of fractures of the hand over the last 25 years. J Hand Surg Am. 2000; 25:817–23.
Article10. Curry GJ. Treatment of finger fractures, simple and compound. Am J Surg. 1946; 71:80–3.
Article11. Hsu LP, Schwartz EG, Kalainov DM, Chen F, Makowiec RL. Complications of K-wire fixation in procedures involving the hand and wrist. J Hand Surg Am. 2011; 36:610–6.
Article12. Black D, Mann RJ, Constine R, Daniels AU. Comparison of internal fixation techniques in metacarpal fractures. J Hand Surg Am. 1985; 10:466–72.
Article13. Lamphier TA. Improper reduction of fractures of the proximal phalanges of fingers. Am J Surg. 1957; 94:926–30.
Article14. Rush LV, Rush HL. Evolution of medullary fixation of fractures by the longitudinal pin. Am J Surg. 1949; 78:324–33.
Article15. Dobyns JH, Linscheid RL, Cooney WP 3rd. Fractures and dislocations of the wrist and hand, then and now. J Hand Surg Am. 1983; 8:687–90.
Article16. Clifford RH. Intramedullary wire fixation of hand fractures. Plast Reconstr Surg (1946). 1953; 11:366–71.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Operative Treatment of Metacarpal Shaft Fracture
- Closed Reduction and Percutaneous K-Wire Fixation of Bony Mallet Finger Using an 18 Gauge Needle
- Comparison between Two Kirschner Wire Fixation and Three Wire Fixation, in Treating of Metacarpal Neck Fracture Using Multiple Retrograde Kirschner Wire Fixation
- Aorto-Innominate Venous Fistula after percutaneous kirschner wire fixation of the Sternoclavivular Joint Anterior Dislocation: A case report
- Treatment of the Clavicle Lateral End Fracture by Kirschner wire and Wire fixation