J Korean Neurosurg Soc.
2015 Sep;58(3):175-183. 10.3340/jkns.2015.58.3.175.
Endovascular Treatment of Vertebral Artery Dissecting Aneurysms That Cause Subarachnoid Hemorrhage : Consideration of Therapeutic Approaches Relevant to the Angioarchitecture
- Affiliations
-
- 1Department of Neurosurgery, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea. realeponym@hanmail.net
- KMID: 2191354
- DOI: http://doi.org/10.3340/jkns.2015.58.3.175
Abstract
OBJECTIVE
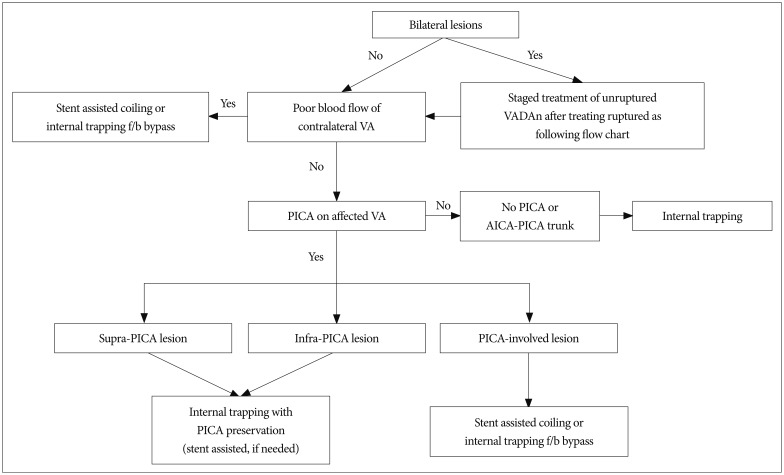
Intracranial ruptured vertebral artery dissecting aneurysms (VADAns) are associated with high morbidity and mortality when left untreated due to the high likelihood of rebleeding. The present study aimed to establish an endovascular therapeutic strategy that focuses specifically on the angioarchitecture of ruptured VADAns.
METHODS
Twenty-three patients with ruptured VADAn received endovascular treatment (EVT) over 7 years. The patient group included 14 women (60.9%) and 9 men (39.1%) between the ages of 39 and 72 years (mean age 54.2 years). Clinical data and radiologic findings were retrospectively analyzed.
RESULTS
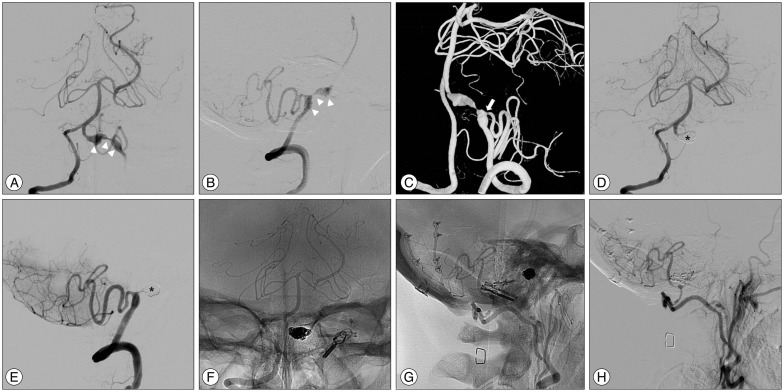
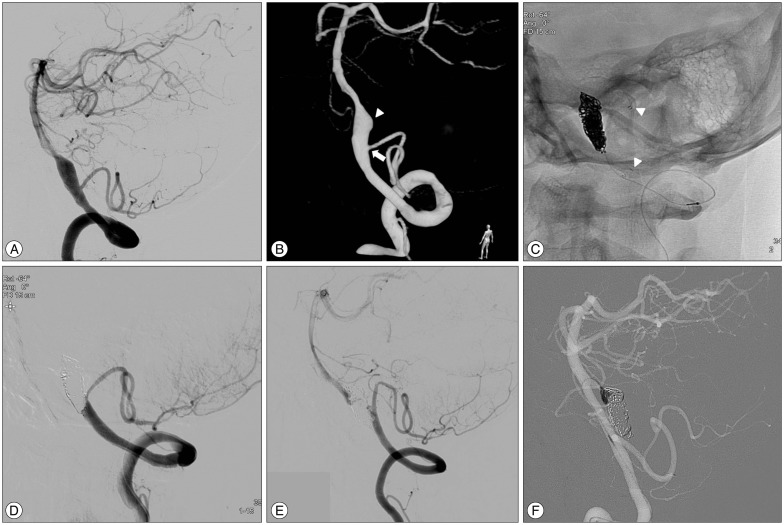
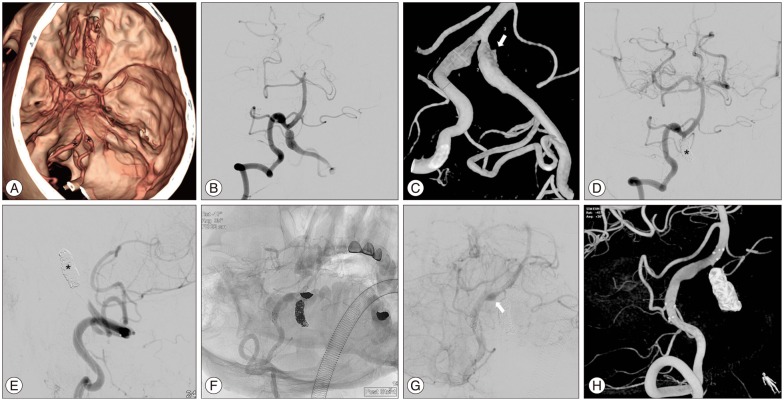
Four patients had aneurysms on the dominant vertebral artery. Fourteen (61%) aneurysms were located distal to the posterior inferior cerebellar artery (PICA). Six (26%) patients had an extracranial origin of the PICA on the ruptured VA, and 2 patients (9%) had bilateral VADAns. Eighteen patients (78%) were treated with internal coil trapping. Two patients (9%) required an adjunctive bypass procedure. Seven patients (30%) required stent-supported endovascular procedures. Two patients experienced intra-procedural rupture during EVT, one of which was associated with a focal medullary infarction. Two patients (9%) exhibited recanalization of the VADAn during follow-up, which required additional coiling. No recurrent hemorrhage was observed during the follow-up period.
CONCLUSION
EVT of ruptured VADAns based on angioarchitecture is a feasible and effective armamentarium to prevent fatal hemorrhage recurrence with an acceptable low risk of procedural complications. Clinical outcomes depend mainly on the pre-procedural clinical state of the patient. Radiologic follow-up is necessary to prevent hemorrhage recurrence after EVT.
MeSH Terms
Figure
Reference
-
1. Aoki N, Sakai T. Rebleeding from intracranial dissecting aneurysm in the vertebral artery. Stroke. 1990; 21:1628–1631. PMID: 2237959.
Article2. Arnold M, Bousser MG, Fahrni G, Fischer U, Georgiadis D, Gandjour J, et al. Vertebral artery dissection : presenting findings and predictors of outcome. Stroke. 2006; 37:2499–2503. PMID: 16960096.3. Chen YA, Qu RB, Bian YS, Zhu W, Zhang KP, Pang Q. Stent placement to treat ruptured vertebral dissecting aneurysms. Interv Neuroradiol. 2013; 19:479–482. PMID: 24355153.
Article4. Chung J, Kim BS, Lee D, Kim TH, Shin YS. Vertebral artery occlusion with vertebral artery-to-posterior inferior cerebellar artery stenting for preservation of the PICA in treating ruptured vertebral artery dissection. Acta Neurochir (Wien). 2010; 152:1489–1492. PMID: 20593207.
Article5. Chung SY, Yoon BH, Park MS, Kim SM. A case of endovascular treatment for followed by side to side bypass for vertebral artery dissecting aneurysms involved posterior inferior cerebellar artery. J Korean Neurosurg Soc. 2014; 55:36–39. PMID: 24570816.
Article6. de Bray JM, Penisson-Besnier I, Dubas F, Emile J. Extracranial and intracranial vertebrobasilar dissections : diagnosis and prognosis. J Neurol Neurosurg Psychiatry. 1997; 63:46–51. PMID: 9221967.
Article7. Endo H, Matsumoto Y, Kondo R, Sato K, Fujimura M, Inoue T, et al. Medullary infarction as a poor prognostic factor after internal coil trapping of a ruptured vertebral artery dissection. J Neurosurg. 2013; 118:131–139. PMID: 23039149.
Article8. Hamada J, Kai Y, Morioka M, Yano S, Todaka T, Ushio Y. Multimodal treatment of ruptured dissecting aneurysms of the vertebral artery during the acute stage. J Neurosurg. 2003; 99:960–966. PMID: 14705721.
Article9. Hamasaki O, Ikawa F, Hidaka T, Kurokawa Y, Yonezawa U. Treatment of ruptured vertebral artery dissecting aneurysms. A short report. Interv Neuroradiol. 2014; 20:304–311. PMID: 24976093.
Article10. Hsu CY, Cheng CY, Lee JD, Lee M, Huang YC, Wu CY, et al. Clinical features and outcomes of spinal cord infarction following vertebral artery dissection : a systematic review of the literature. Neurol Res. 2013; 35:676–683. PMID: 23562138.
Article11. Iihara K, Sakai N, Murao K, Sakai H, Higashi T, Kogure S, et al. Dissecting aneurysms of the vertebral artery : a management strategy. J Neurosurg. 2002; 97:259–267. PMID: 12186451.12. Kim MJ, Chung J, Kim SL, Roh HG, Kwon BJ, Kim BS, et al. Stenting from the vertebral artery to the posterior inferior cerebellar artery. AJNR Am J Neuroradiol. 2012; 33:348–352. PMID: 22051805.
Article13. Kitanaka C, Morimoto T, Sasaki T, Takakura K. Rebleeding from vertebral artery dissection after proximal clipping. Case report. J Neurosurg. 1992; 77:466–468. PMID: 1506896.14. Koh JS, Ryu CW, Lee SH, Bang JS, Kim GK. Bilateral vertebral-artery-dissecting aneurysm causing subarachnoid hemorrhage cured by staged endovascular reconstruction after occlusion. Cerebrovasc Dis. 2009; 27:202–204. PMID: 19153480.
Article15. Luo CB, Chang CY, Teng MM, Chang FC. Endovascular treatment of ruptured vertebral dissecting aneurysms with electrodetachable coils. J Chin Med Assoc. 2005; 68:578–584. PMID: 16379342.
Article16. Lylyk P, Ceratto R, Hurvitz D, Basso A. Treatment of a vertebral dissecting aneurysm with stents and coils : technical case report. Neurosurgery. 1998; 43:385–388. PMID: 9696097.
Article17. MacKay CI, Han PP, Albuquerque FC, McDougall CG. Recurrence of a vertebral artery dissecting pseudoaneurysm after successful stent-supported coil embolization : case report. Neurosurgery. 2003; 53:754–759. discussion 760-761PMID: 12943592.18. Mahmood A, Dujovny M, Torche M, Dragovic L, Ausman JI. Microvascular anatomy of foramen caecum medullae oblongatae. J Neurosurg. 1991; 75:299–304. PMID: 2072169.
Article19. Marinković S, Milisavljević M, Gibo H, Maliković A, Djulejić V. Microsurgical anatomy of the perforating branches of the vertebral artery. Surg Neurol. 2004; 61:190–197. discussion 197PMID: 14751642.
Article20. Mercier PH, Brassier G, Fournier HD, Picquet J, Papon X, Lasjaunias P. Vascular microanatomy of the pontomedullary junction, posterior inferior cerebellar arteries, and the lateral spinal arteries. Interv Neuroradiol. 2008; 14:49–58. PMID: 20557786.
Article21. Mizutani T, Aruga T, Kirino T, Miki Y, Saito I, Tsuchida T. Recurrent subarachnoid hemorrhage from untreated ruptured vertebrobasilar dissecting aneurysms. Neurosurgery. 1995; 36:905–911. discussion 912-913PMID: 7791980.
Article22. Ramgren B, Cronqvist M, Romner B, Brandt L, Holtås S, Larsson EM. Vertebrobasilar dissection with subarachnoid hemorrhage : a retrospective study of 29 patients. Neuroradiology. 2005; 47:97–104. PMID: 15711986.
Article23. Santos-Franco JA, Zenteno M, Lee A. Dissecting aneurysms of the vertebrobasilar system. A comprehensive review on natural history and treatment options. Neurosurg Rev. 2008; 31:131–140. discussion 140PMID: 18309525.
Article24. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. 2001; 344:898–906. PMID: 11259724.
Article25. Shin YS, Kim BM, Kim SH, Suh SH, Ryu CW, Koh JS, et al. Endovascular treatment of bilateral intracranial vertebral artery dissecting aneurysms presenting with subarachnoid hemorrhage. Neurosurgery. 2012; 70(1 Suppl Operative):75–81. discussion 81PMID: 21796008.
Article26. Su W, Gou S, Ni S, Li G, Liu Y, Zhu S, et al. Management of ruptured and unruptured intracranial vertebral artery dissecting aneurysms. J Clin Neurosci. 2011; 18:1639–1644. PMID: 22018807.
Article27. Taha MM, Sakaida H, Asakura F, Maeda M, Toma N, Yamamoto A, et al. Endovascular management of vertebral artery dissecting aneurysms : review of 25 patients. Turk Neurosurg. 2010; 20:126–135. PMID: 20401839.28. Tsukahara T, Wada H, Satake K, Yaoita H, Takahashi A. Proximal balloon occlusion for dissecting vertebral aneurysms accompanied by subarachnoid hemorrhage. Neurosurgery. 1995; 36:914–919. discussion 919-920PMID: 7791981.
Article29. Yamaura A, Watanabe Y, Saeki N. Dissecting aneurysms of the intracranial vertebral artery. J Neurosurg. 1990; 72:183–188. PMID: 2404089.
Article30. Yamaura I, Tani E, Yokota M, Nakano A, Fukami M, Kaba K, et al. Endovascular treatment of ruptured dissecting aneurysms aimed at occlusion of the dissected site by using Guglielmi detachable coils. J Neurosurg. 1999; 90:853–856. PMID: 10223450.
Article31. Yoon WK, Kim YW, Kim SR, Park IS, Kim SD, Jo KW, et al. Angiographic and clinical outcomes of stent-alone treatment for spontaneous vertebrobasilar dissecting aneurysm. Acta Neurochir (Wien). 2010; 152:1477–1486. discussion 1486PMID: 20508955.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Coil Trapping of a Ruptured Dissecting Aneurysm of the Vertebral Artery Using Detachable Coils and Micro-Tornado(R) Coils
- Early Rebleeding after Internal Trapping of a Ruptured Vertebral Artery Dissecting Aneurysm: A Case Report
- Bilateral Vertebral Artery Dissecting Aneurysms: A Long Term Follow-up Results of Microsurgical Trapping and Proximal Occlusion
- Endovascular Treatment of Symptomatic Vertebral Artery Dissecting Aneurysms
- Treatment Outcomes in Patients with a Vertebral Artery Dissecting Aneurysm