J Korean Neurosurg Soc.
2013 Sep;54(3):239-242. 10.3340/jkns.2013.54.3.239.
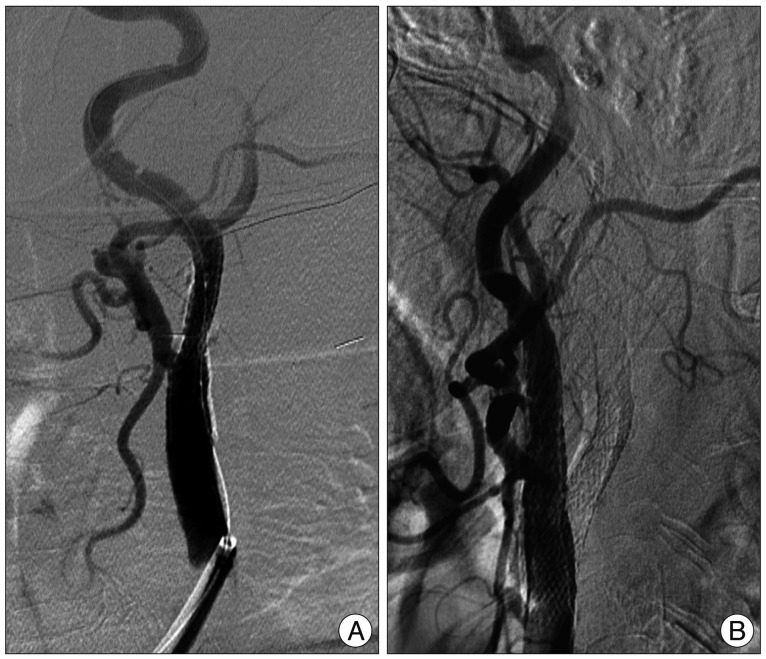
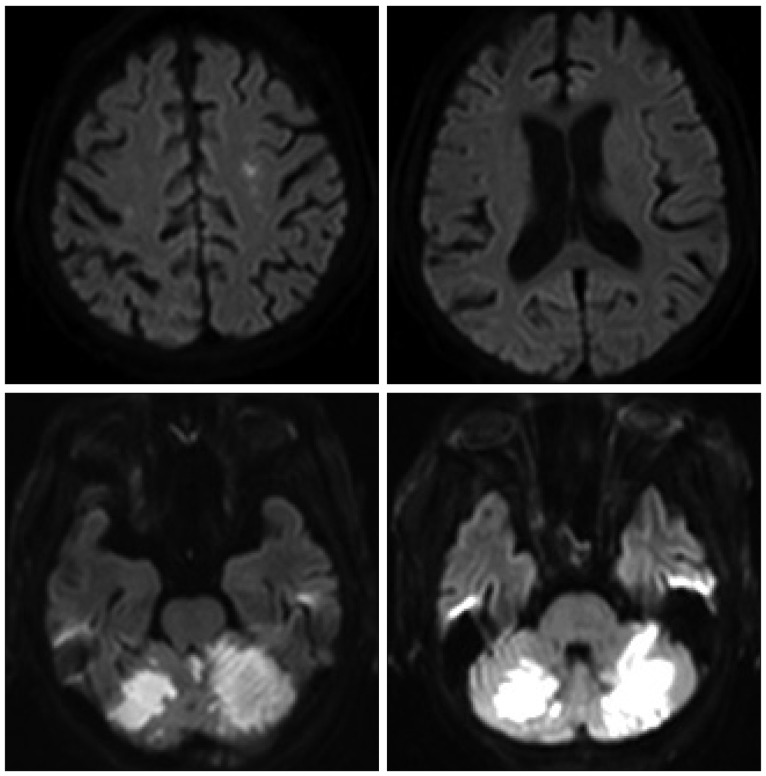
Bilateral Superior Cerebellar Artery Infarction after Stent-Angioplasty for Internal Carotid Artery Stenosis
- Affiliations
-
- 1Department of Neurosurgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea. y77y85@hanmail.net
- 2Department of Radiology, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 3Department of Neurology, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- KMID: 2190905
- DOI: http://doi.org/10.3340/jkns.2013.54.3.239
Abstract
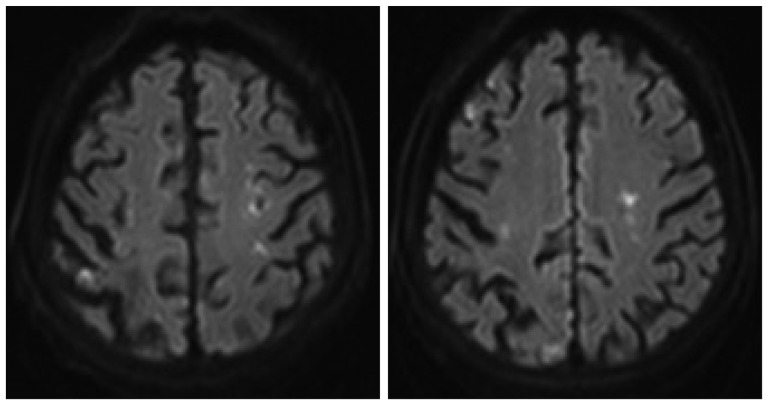
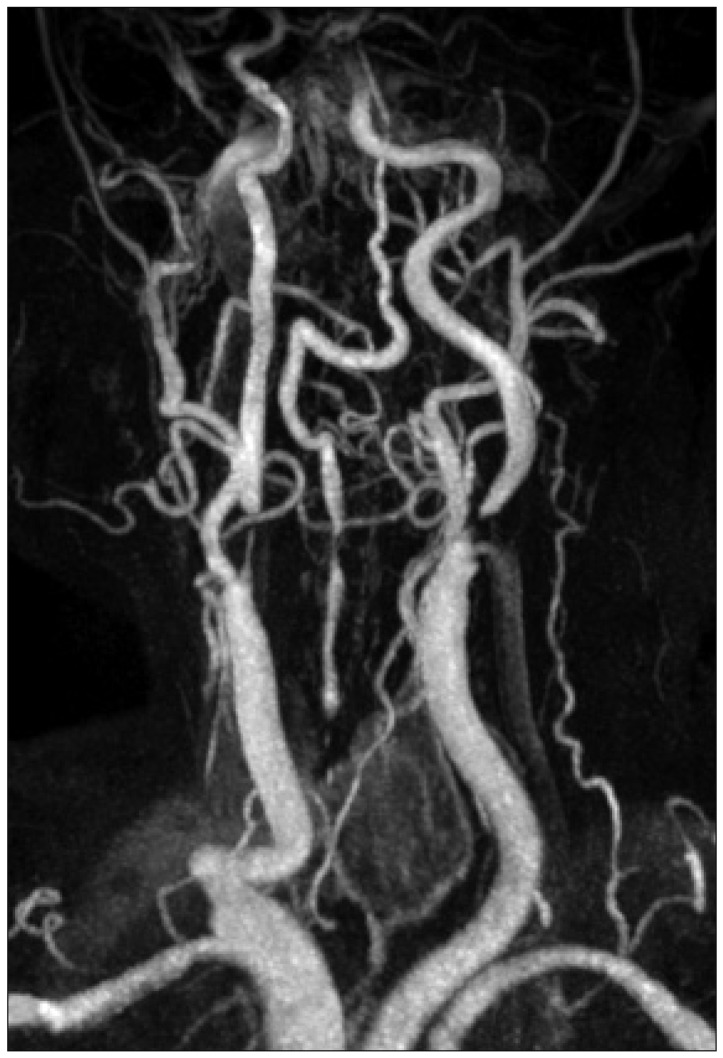
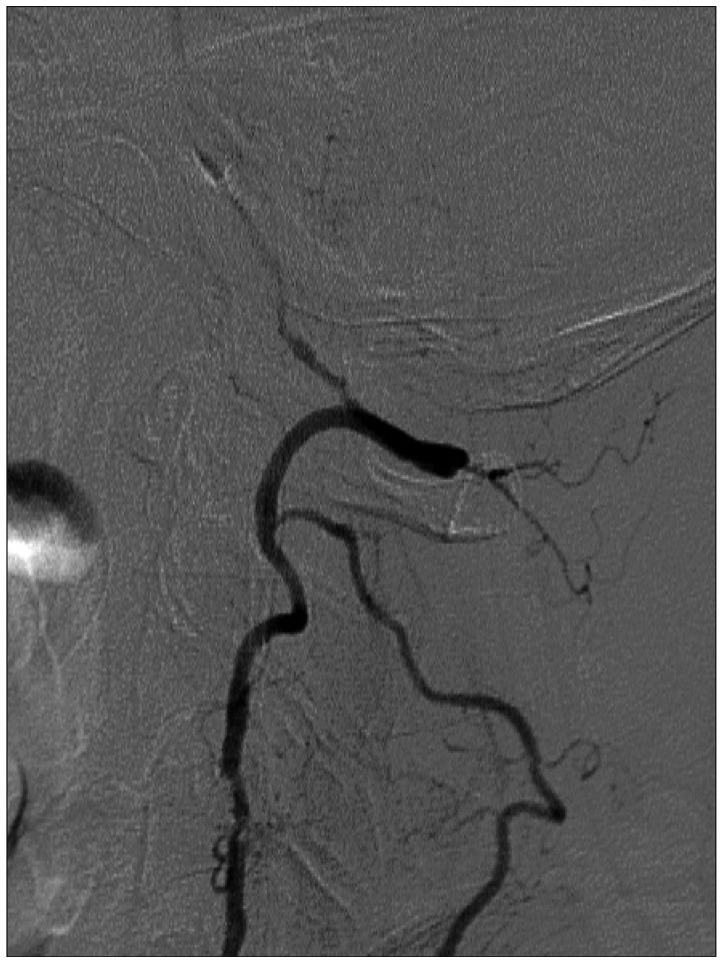
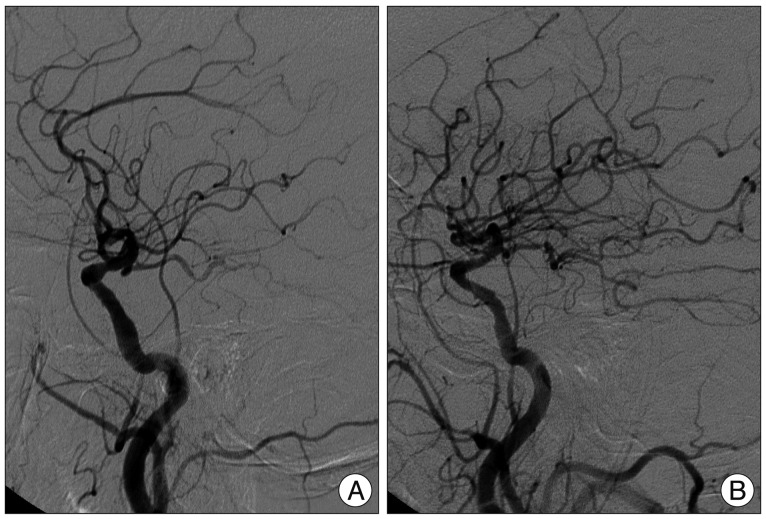
- Spontaneous bilateral cerebellar infarction in the territory of the superior cerebellar arteries is extremely rare. Occasionally there have been reports of bilateral cerebellar infarction due to vertebrobasilar atherosclerotic occlusion or stenosis, whereas no report of bilateral cerebellar infarction due to complicated hemodynamic changes. In this report, we present a patient with bilateral cerebral infarctions related to stenoses of bilateral internal carotid arteries, in whom vertebrobasilar system was supplied by multiple collaterals from both posterior communicating arteries and right external carotid artery. We performed stent-angioplasty of bilateral internal cerebral arterial stenosis, and then acute infarction developed on bilateral superior cerebellar artery territories. The authors assumed that the infarction occurred due to hemodynamic change between internal carotid artery and external carotid artery after stent-angioplasty for stenosis of right internal carotid artery.
MeSH Terms
Figure
Reference
-
1. Grunwald IQ, Politi M, Reith W, Krick C, Karp K, Zimmer A, et al. Hyperperfusion syndrome after carotid stent angioplasty. Neuroradiology. 2009; 51:169–174. PMID: 19104793.
Article2. Jang HJ, Cho KY, Lim JS, Park SK, Lee RS. Cerebral infarction after transfemoral carotid angiography : report of 2 cases. Korean J Cerebrovasc Surg. 2008; 10:528–531.3. Kim DE, Choi SM, Yoon W, Kim BC. Hyperperfusion syndrome after carotid stent-supported angioplasty in patients with autonomic dysfunction. J Korean Neurosurg Soc. 2012; 52:476–479. PMID: 23323169.
Article4. Kim DS, Kim JK, Yoo DS, Huh PW, Cho KS, Kang JK. Complications of cerebral revascularization surgery. Korean J Cerebrovasc Dis. 2001; 3:50–53.5. Kiroğlu Y, Karabulut N, Oncel C, Akdogan I, Onur S. Bilateral symmetric junctional infarctions of the cerebellum : a case report. Surg Radiol Anat. 2010; 32:509–512. PMID: 19760056.
Article7. Meyers PM, Phatouros CC, Higashida RT. Hyperperfusion syndrome after intracranial angioplasty and stent placement. Stroke. 2006; 37:2210–2211. PMID: 16888253.
Article8. Müller M, Schimrigk K. Vasomotor reactivity and pattern of collateral blood flow in severe occlusive carotid artery disease. Stroke. 1996; 27:296–299. PMID: 8571426.
Article9. Rezende MT, Spelle L, Mounayer C, Piotin M, Abud DG, Moret J. Hyperperfusion syndrome after stenting for intracranial vertebral stenosis. Stroke. 2006; 37:e12–e14. PMID: 16339466.
Article10. Romero JR, Pikula A, Nguyen TN, Nien YL, Norbash A, Babikian VL. Cerebral collateral circulation in carotid artery disease. Curr Cardiol Rev. 2009; 5:279–288. PMID: 21037845.
Article11. Sánchez-Arjona MB, Sanz-Fernández G, Franco-Macías E, Gil-Peralta A. Cerebral hemodynamic changes after carotid angioplasty and stenting. AJNR Am J Neuroradiol. 2007; 28:640–644. PMID: 17416813.12. Schechter MM. The occipital-vertebral anastomosis. J Neurosurg. 1964; 21:758–762. PMID: 14210007.
Article13. Shim JH, Rha HK, Kim SR, Joo WI, Kim MC, Choi CR. Hyperperfusion syndrome after extracranial-intracranial bypass surgery. J Korean Neurosurg Soc. 2003; 34:526–530.14. Tada Y, Mizutani T, Nishimura T, Tamura M, Mori N. Acute bilateral cerebellar infarction in the territory of the medial branches of posterior inferior cerebellar arteries. Stroke. 1994; 25:686–688. PMID: 8128527.
Article15. Tsukamoto T, Seki H, Saitoh J, Watanabe K. A case of bilateral cerebellar peduncle infarction. Jpn J Med. 1991; 30:376–378. PMID: 1942654.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Transluminal Angioplasty with Palmaz-Schatz Stent in the Carotid Artery Stenosis
- A Case of Transradial Approach to Carotid Artery Angioplasty and Stenting in Left Internal Carotid Stenosis
- A Case of Transseptal Approach to Carotid Artery Stenting in Right Internal Carotid Stenosis
- How to Escape Stentriever Wedging in an Open-cell Carotid Stent during Mechanical Thrombectomy for Tandem Cervical Internal Carotid Artery and Middle Cerebral Artery Occlusion
- Supra-aortic Arterial Recanalization: Report of 5 cases