J Korean Orthop Assoc.
2009 Jun;44(3):301-310. 10.4055/jkoa.2009.44.3.301.
Autogenous Osteochondral Grafting for Treating Osteochondral Defect of the Femoral Condyle of the Knee Joint
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Inje University, Busan Paik Hospital, Busan, Korea. lilac-lee@hanmail.net
- 2Department of Orthopedic Surgery, Busan Bon Hospital, Busan, Korea.
- KMID: 2186338
- DOI: http://doi.org/10.4055/jkoa.2009.44.3.301
Abstract
-
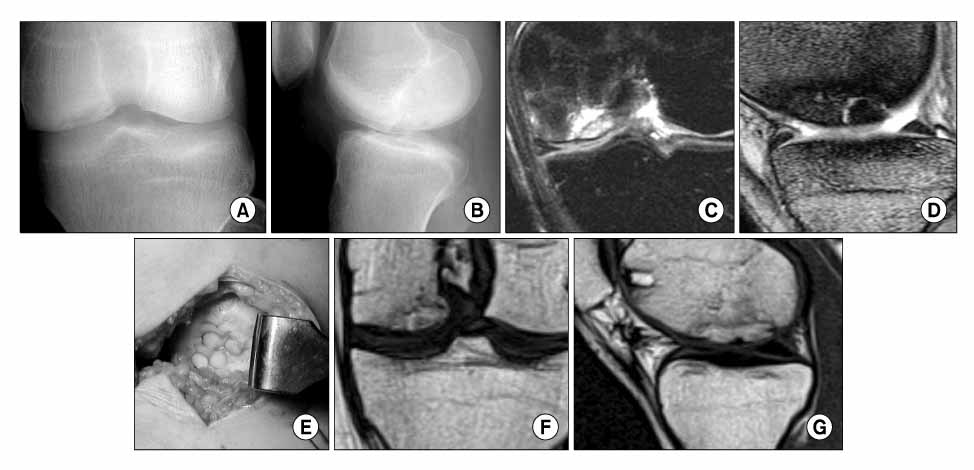
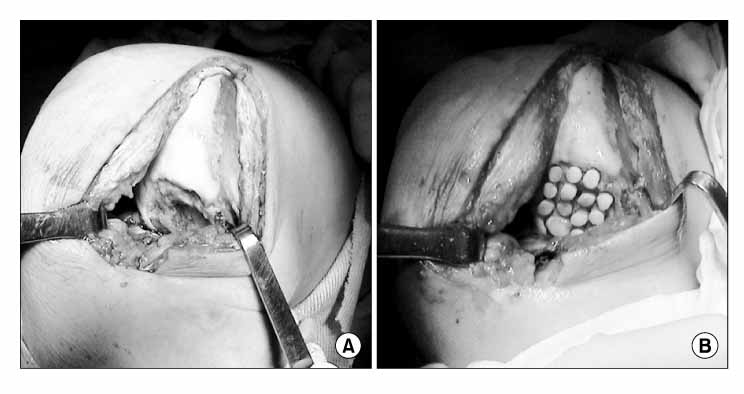
PURPOSE: We wanted to evaluate the outcomes of an autologous osteochondral graft (Mosaicplasty) for treating chondral defects of the femoral condyle and We assessed the factors affecting the clinical results.
MATERIALS AND METHODS
This study enrolled 18 patients (19 cases) who underwent an autogenous osteochondral graft to treat a osteochondral defect in the femoral condyle from July 2000 to June 2006. The average age was 26.2 years old (age range: 16-48 years old). Among the patients, 17 cases were men. In 14 cases, the osteochondral defects were localized in the medial femoral condyle and only 5 cases showed a defect in the lateral femoral condyle. The average size of the osteochondral defects was 4.2 cm2 (1-13 cm2). The Lysholm knee scoring scale and the Tegner's activity score were applied for clinical evaluation. Further, we carried out simple X-ray for all the cases and we performed MRI in 5 cases for the radiological evaluation. Tthe factors affecting the clinical results were also analyzed and the complications were evaluated.
RESULTS
The average follow-up period was 22 months (range: 6-55 months). Eighten out of 19 cases (94.7%) were able to return to ordinary life. The Lysholm knee scoring scale and the Tegner's activity score indicated much better clinical results for small lesions and for young patients. For the radiological results, all the cases displayed a decrease in the size of radiolucent zones on the follow up X-ray. Among the 5 cases for which an MRI was performed, graft unions were observed in 3 cases, but 2 cases displayed continuous peri-graft edema. Any other complications involving the donor and recipient site were not observed.
CONCLUSION
We conclude that autogenous osteochondral grafting is useful for specific patients depending on the size of the lesion and the patient's age. It is a valuable treatment option for osteochondral defects in the knee joint.
Figure
Reference
-
1. Ahmad CS, Cohen ZA, Levine W, Ateshian GA, Mow Van C. Biomedical and topographic considerations for autologous osteochondral grafting in the knee. Am J Sports Med. 2001. 29:201–206.2. Aichroth PM, Patel DV, Moyes ST. A prospective review of arthroscopic debridement for degenerative joint disease of the knee. Int Orthop. 1991. 15:351–355.
Article3. Bohndorf K. Osteochondritis (osteochondrosis) dissecans: a review and new MRI classification. Eur Radiol. 1998. 8:103–112.
Article4. Brittberg M, Lindahl A, Ohlsson C, Isaksson O, Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994. 331:889–895.
Article5. Choi NH. Mosaicplasty for the treatment of the chondral defect of the knee. J Korean Orthop Sports Med. 2005. 4:12–17.6. Curl WW, Krome J, Gordon ES, Paterson Smith B, Poehling GG. Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy. 1997. 13:456–460.
Article7. Duchov J, Hess T, Kohn D. Primary stability of press-fit-implanted osteochondral grafts. Influence of graft size, repeated insertion, and harvesting technique. Am J Sports Med. 2000. 28:24–27.8. In : Gross AE, Hangody L, Minas T, O'Driscoll SW, editors. The surgical treatment of articular cartilage defects of the knee. 2001. Abstracts of the sixty-eighth Annual Meeting of the American Academy of Orthopaedic Surgeons; San Francisco, USA.9. Hangody L, Füles P. Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am. 2003. 85:25–32.10. Hangody L, Kish G, Karapati Z, Szerb I, Udvarhelyi I. Arthroscopic autogenous osteochondral mosaicplasty for the treatment of femoral condylar articular defects. A pre-liminary report. Knee Surg Sports Traumaol Athrosc. 1997. 5:262–267.11. Hangody L, Rathonyi GK, Duska Z, Vásárhelyi G, Füles P, Módis L. Autologous osteochondral mosaicplasty. Surgical technique. J Bone Joint Surg Am. 2004. 86:Suppl 1. S65–S72.12. Horas U, Pelinkovic D, Herr G, Aigner T, Schnettler R. Autologous chondrocyte implantation and osteochondral cylinder transplantation in cartilage repair of the knee joint. A prospective, comparative trial. J Bone Joint Surg Am. 2003. 85:185–192.13. Imhoff AB, Ottl GM, Burkart A, Traub S. Autologous osteochondral transplatation on various joints. Orthopade. 1999. 28:33–44.14. Jakob RP, Franz T, Gautier E, Manil-Varlet P. Autologous osteocondral grafting in the knee: indications, results and reflections. Clin Orthop Relat Res. 2002. 401:170–184.15. Jerosch J, Filler T, Peuker E. Is there an option for harvesting autologous osteochondral grafts without damaging weight-bearing areas in the knee joint? Knee Surg Sports Traumatol Arthrosc. 2000. 8:237–240.
Article16. Johnson LL. Arthroscopic abrasion arthroplasty historical and pathologic perspective: present status. Arthroscopy. 1986. 2:54–69.
Article17. Jürgensen I, Bachmann G, Schleicher I, Haas H. Arthroscopic versus conservative treatment of osteochondritis dissecans of the knee: value of magnetic resonance imaging in therapy planning and follow-up. Arthroscopy. 2002. 18:378–386.18. Koh JL, Wirsing K, Lautenschlager E, Zhang LO. The effect of graft height mismatch on contact pressure following osteochondral grafting: a biomechanical study. Am J Sports Med. 2004. 32:317–320.19. Link TM, Mischung J, Wörtler K, Burkart A, Rummeny EJ, Imhoff AB. Normal and pathological MR findings in osteochondral autografts with longitudinal follow-up. Eur Radiol. 2006. 16:88–96.
Article20. Mankin HJ. The response of articular cartilage to mechanical injury. J Bone Joint Surg Am. 1982. 64:460–466.
Article21. Makino T, Fugioka H, Terukina M, Yoshiya S, Matsui N, Kurosaka M. The effect of graft sizing on osteochondral transplantation. Arthroscopy. 2004. 20:837–840.
Article22. Marcacci M, Kon E, Zaffagnini S, Visani A. Use of autologous grafts for reconstruction of osteochondral defects of the knee. Orthopedics. 1999. 22:595–600.
Article23. Nelson DW, DiPaola J, Colville M, Schmidgall J. Osteochondritis dissecans of the talus and knee: prospective comparison of MR and arthroscopic classifications. J Comput Assist Tomogr. 1990. 14:804–808.24. Newman AP. Articular cartilage repair. Am J Sports Med. 1998. 26:309–324.
Article25. Rodrigo JJ, Steadman RJ, Silliman JF, et al. Improvement of full-thickness chondral defect healing in the human knee after debridement and microfracture using continuous passive motion. Am J Knee Surg. 1994. 7:109–116.26. Peterson L, Menache D, Grande D, et al. Chondracyte transplantation: an experimental model in the rabbit. Trans Orthop Res Soc. 1984. 9:218.27. Schneider T, Fink B, Jerosch J, Assheuer J, Rüther W. The value of magnetic resonance imaging as postoperative control after arthroscopic treatment of osteochondritis dissecans. Arch Orthop Trauma Surg. 1998. 117:235–239.
Article28. Sanders TG, Mentzer KD, Miller MD, Morrison WB, Campbell SE, Penrod BJ. Autogenous osteochondral "plug" transfer for the treatment of focal chondral defects: postoperative MR appearance with clinical correlation. Skeletal Radiol. 2001. 30:570–578.
Article29. Sgaglione NA, Mimiaci A, Gillogy SD, Carter TR. Update on advance surgical techniques in the treatment of traumatic focal articular cartilage legions in the knee. Arthroscopy. 2002. 18:Suppl 1. S9–S32.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concomitant Osteochondral Autograft Transplantation and Fixation of Osteochondral Fragment for Treatment of a Massive Osteochondritis Dissecans: A Report of 8-Year Follow-up Results
- Osteochondral Autograft Using Head of Proximal Phalanx of Toe for Partial Osteochondral Defect of Proximal Interphalangeal Joint: A Case Report
- Osteochondral Lesion in Diffuse Pigmented Villonodular Synovitis of the Knee
- Treatment of Unstable Osteochondral Dissecans Lesion of the Knee Joint Using Autologous Osteochondral Plug
- Bilateral Osteochondritis Dissecans of the Femoral Condyles in Both Knees: A Report of Two Sibling Cases