J Korean Med Assoc.
2008 Apr;51(4):327-334. 10.5124/jkma.2008.51.4.327.
Coronary Artery Disease and Coronary Artery Bypass Surgery in Patients of Middle Age
- Affiliations
-
- 1Department of Cardiovascular Surgery, Sungkyunkwan University School of Medicine, Korea. ytlee@yahoo.com
- KMID: 2185741
- DOI: http://doi.org/10.5124/jkma.2008.51.4.327
Abstract
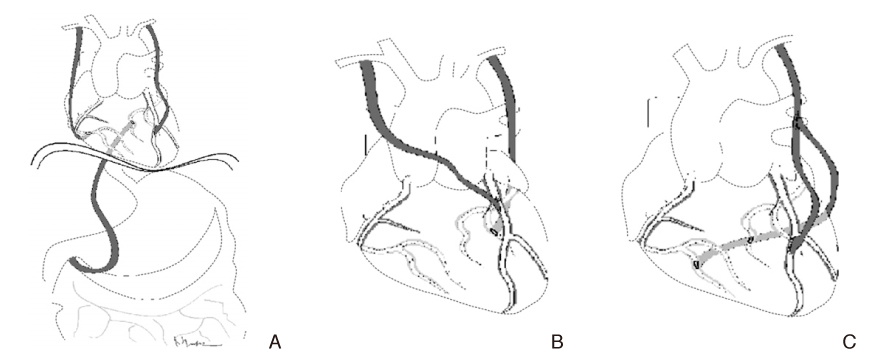
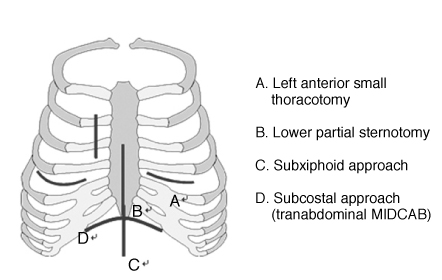
- Coronary artery disease in young patients (< 40 years) is not common. However, when it occurs it has symptoms that are more frequent and a more rapid progression when compared to older affected patients. Younger patients are more likely to have normal coronary arteries and have nonobstructive disease < 70%, single-vessel disease and less extensive coronary artery atherosclerosis. Therefore, it is likely that there are differences in the cardiac risk factors in young patients undergoing coronary artery bypass surgery. Smoking, hypercholesterolemia, unstable angina, and myocardial infarction were more frequent in the young age group, and diabetes and hypertension were more common in older patients. The need for repeated interventions, additional surgery andlate myocardial infarction were more common in younger patients. Favorable factors associated with increased survival included the absence of unstable angina, a left ventricle ejection fraction of =45% and the use of the internal thoracic artery for procedures. The patency of saphenous vein grafts in younger patients was inferior to vein graft patency in the older patients. Risk factors such as hyperlipidemia, smoking and a family history of coronary artery disease may be related to the early graft failure in young patients. The patency of the internal thoracic artery to the left anterior descending artery was above 90% over 10 years; however, it was around 50% for the saphenous vein. Therefore, the aggressive use of internal thoracic arteries, for coronary artery bypass surgery in young patients, was essential for improved late survival and the event free survival (reduced additional interventions, surgeries and hospital admissions). The Ycomposite graft technique or sequential anastomosis, improves the coronary artery anastomosis with fewer arterial grafts. Other arterial grafts such as the gastroepiploic artery, radial artery and inferior epigastric artery could be used for coronary artery bypass surgery in young patients for free grafts, in situ grafts or Y-composite grafts. Young patients that have coronary artery bypass surgery have a favorable prognosis when the internal thoracic arteries or other arterial grafts are used. In addition, such as the Y-composite graft technique and sequential anastomosis can also be used with a high success rate.
Keyword
MeSH Terms
-
Angina, Unstable
Arteries
Atherosclerosis
Coronary Artery Bypass
Coronary Artery Disease
Coronary Vessels
Disease-Free Survival
Epigastric Arteries
Gastroepiploic Artery
Heart Ventricles
Humans
Hypercholesterolemia
Hyperlipidemias
Hypertension
Mammary Arteries
Middle Aged
Myocardial Infarction
Prognosis
Radial Artery
Risk Factors
Saphenous Vein
Smoke
Smoking
Transplants
Veins
Smoke
Figure
Reference
-
1. Zimmerman FH, Cameron F, Fisher LD, Ng G. Myocardial infarction in young adults: angiographic characterization, risk factors and prognosis (coronary artery surgery study registry). J Am Coll Cardiol. 1995. 26:654–661.
Article2. Kannel WB, Abbott RD. Incidence and prognosis of unrecognized myocardial infarction. N Engl J Med. 1984. 311:1144–1147.
Article3. Mosca L. Fuster V, Topol EJ, Nabel EG, editors. Estrogen and Atherothrombosis. Atherothrombosis & coronary artery disease. 2005. Philadelphia: Lippincott Williams and Wilkins;297–307.4. Uddin SN, Siddiqui NI, Bagum F, Malik F, Rahman S, Ali MS. Coronary artery disease in young adults-angiographic profile. Mymensingh Med J. 2004. 13:11–15.5. Rohrer-Gubler I, Niederhauser U, Turina MI. Late outcome of coronary artery bypass grafting in young versus older patients. Ann Thorac Surg. 1998. 65:377–382.
Article6. Graziosi GC, Wolterbeek DW, Kappetein AP, Huysmans HA. Risk factors in coronary artery bypass surgery for patients 40 years of age and younger. Thorac Cardiovasc Surg. 1994. 42:259–263.
Article7. Malinowski M, Mrozek R, Twardowski R, Malinowski M, Mrozek R, Twardowski R, Biernat J, Deja MA, Widenka K, Dalecka AM, Kobielusz-Gembala I, Janusiewicz P, Wos S, Golba KS. Left internal mammary artery improves 5-year survival in patients under 40 subjected to surgical revascularization. Heart Surg Forum. 2006. 9:E493–E498.
Article8. Samuels LE, Sharma S, Kaufman MS, Morris RJ, Brockman SK. Coronary artery bypass grafting in patients in their third decade of life. J Card Surg. 1996. 11:402–407.
Article9. Kelly TF, Craver JM, Jones EL, Hatcher CRJ. Coronary revascularization in patients 40 years and younger: survival experience and long-term follow-up. Am Surg. 1978. 44:675–678.10. Lytle BW, Loop LD. Coronary artery bypass grafting in young adults. Chest. 1987. 91:291–292.
Article11. van Son JAM, Smedts F, Vincent JG, van Lier HJJ, Kubat K. Comparative anatomic studies of various arterial conduits for myocardial revascularization. J Thorac Cardiovasc Surg. 1990. 99:703–707.
Article12. Li XN, Stulz P, Siebenmann PP, Li XN, Stulz P, Siebenmann RP, Yang Z, Lüscher TF. Different effects of activated platelets in the right gastroepiploic and internal mammary arteries. J Thorac Cardiovasc Surg. 1992. 104:1294–1302.
Article13. Rosenfeldt FL, He GW, Buxton BF, Angus JA. Pharmacology of coronary artery bypass grafts. Ann Thorc Surg. 1999. 67:878–888.
Article14. Tector AJ, Amundsen S, Schmahl TM, et al. Total revas-cularization with T grafts. Ann Thorac Surg. 1994. 57:33–39.
Article15. Pick AW, Orszulak TA, Anderson BJ, et al. Single versus bilateral internal mammary artery grafts: 10-year outcome analysis. Ann Thorac Surg. 1997. 64:599–605.
Article16. Lytle BW, Blackstone EH, Loop FD. Two internal thoracic artery grafts are better than one. J Thorac Cardiovasc Surg. 1999. 117:855–872.
Article17. Pym J, Brown PM, Charrette EJ, Parker JO, West RO. Gastroepiploic-coronary anastomosis. A viable alternative bypass graft. J Thorac Cardiovasc Surg. 1997. 94:256–259.18. Acar C, Jebara VA, Portoghese M, Acar C, Jebara VA, Portoghese M, Beyssen B, Pagny JY, Grare P, Chachques JC, Fabiani JN, Deloche A, Guermonprez JL. Revival of the radial artery for coronary artery bypass grafting. Ann Thorac Surg. 1992. 54:652–659.
Article19. Maniar HS, Sundt TM, Barner HB, Maniar HS, Sundt TM, Barner HB, Prasad SM, Peterson L, Absi T, Moustakidis P. Effect of target stenosis and location on radial artery graft patency. J Thorac Cardiovasc Surg. 2002. 123:45–52.
Article20. Sauvage LR, Wu H, Kowalsky TE, Sauvage LR, Wu HD, Kowalsky TE, Davis CC, Smith JC, Rittenhouse EA, Hall DG, Mansfield PB, Mathisen SR, Usui Y. Healing basis and surgical techniques for complete revascularization of the left ventricle using only the internal mammary arteries. Ann Thorac Surg. 1986. 57:33–39.
Article21. Tector A, McDonald ML, Kress DC, Downey FX, Schmahl TM. Purely internal thoracic artery grafts: outcomes. Ann Thorac Surg. 2001. 72:450–455.
Article22. Calafiore AM, Di Giammarco G. Complete revascularization with three or more arterial conduits. Sem Thorac Cardiovasc Surg. 1996. 8:15–23.23. Mavroudis C, Backer CL, Muster AJ, Mavroudis C, Backer CL, Muster AJ, Pahl E, Sanders JH, Zales VR, Gevitz M. Expanding indications for pediatric coronary artery bypass. J Thorac Cardiovasc Surg. 1996. 111:181–189.
Article24. Basso C, Maron BJ, Corrado D, Thiene G. Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden death in young competitive atheletes. J Am Coll Cardiol. 2000. 35:1493–1501.
Article25. Ghosh PK. Anomalous origin of the right coronary artery. Eur J Cardiothorac Surg. 1997. 12:164–165.
Article26. Daehnert I, Rotzsch C, Krause S, Dorszewski A, Kostelka M. Synconpe in a child owing to intramural course of the left coronary artery. Acta Paediatr. 2003. 92:1339–1342.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combined Bilateral Lung Transplantation and Off-Pump Coronary Artery Bypass
- The Right Gastroepiploic Artery Graft for Coronary Artery Bypass Grafting: A 30-Year Experience
- Native Coronary Artery and Grafted Artery Spasm Just after Coronary Artery Bypass Grafting: A Case Report
- Off-Pump Coronary Artery Bypass Grafting in Moyamoya Disease
- A Hybrid Procedure for Coronary Artery Disease with Left Subclavian Artery Stenosis