J Korean Med Assoc.
2004 Jul;47(7):645-652. 10.5124/jkma.2004.47.7.645.
Effectiveness of Bypass Surgery in Treatment and Prevention for Cerebrovascular Occlusive Disease
- Affiliations
-
- 1Department of Neuro Surgery, The Catholic University of Korea, College of Medicine, St. Mary's Hospital, Korea. hkrha@catholic.ac.kr
- KMID: 2183483
- DOI: http://doi.org/10.5124/jkma.2004.47.7.645
Abstract
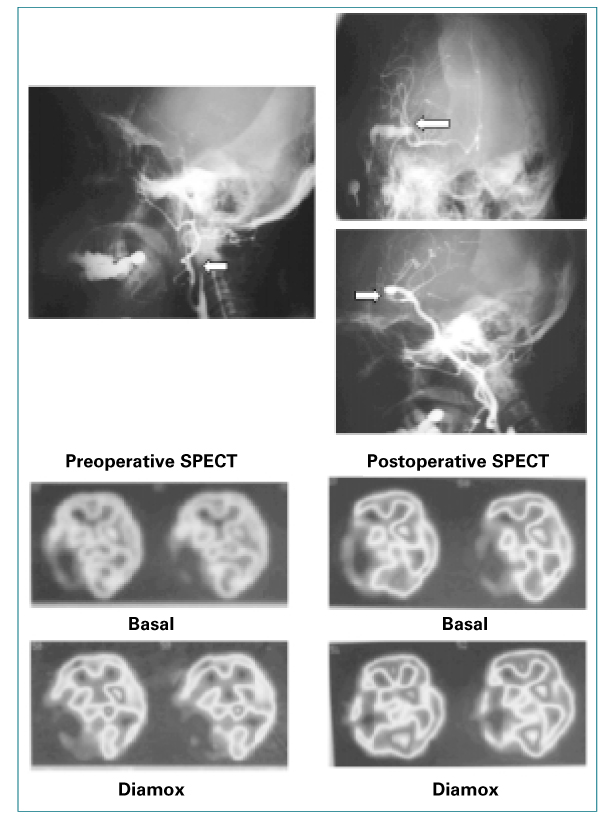
- To study the effect of extracranial-intracranial(EC/IC) bypass on symptomatic patients with hemodynamic cerebral ischemia, we prospectively reviewed 76 patients who underwent EC/IC bypass surgery in patients with occlusive cerebrovascular disease. A series of 76 patients treated in a 7 years period met following criteria. (1) symptomatic internal carotid artery(ICA) or middle cerebral artery(MCA) obstruction or stenosis over 80%. (2) decrease in basal cerebral blood flow(CBF) over 10%. (3) decreased reactivity of CBF in response to acetazolamide. Among these, the types of ischemic episodes were transient ischemic attack(TIA) or reversible ischemic neurological deficit(RIND) in 39, minor stroke in 22, and major stroke in 15. Based on our criteria, superficial temporal artery(STA)-MCA anastomosis was performed in 67 cases and EC-IC bypass grafting using saphenous vein or radial artery in 9. Average follow up period was 26 months(3 months~7 year). Patency of bypass was confirmed by postoperative angiography or magnetic resonence angiography(MRA) in all case except four cases. Of the 72 patients with patiency of bypass, 68 patients(94%) have had an excellent to good outcome with improvement of preoperative neurologic or cognitive dysfunction, 3 patients showed no improvement of preoperative neurologic symptoms and remaining one patient had new developed deficit. All 72 patients with patency of bypass had experienced no further cerebral ischemic events during following period. Postoperative significant improvement of CBF to acetazolamide was showed in 68 cases(94%) of the 72 cases with patency of bypass, while the basal CBF showed significant improved in 31cases. Postoperative permanent neurologic deficit occurred only in one. In view of these finding, the author suggest that EC-IC bypass surgery is a reliable and resonably safe method for establishing new pathways of collateral circulation to the brain and to be considered as an appropriate therapy for improvement of the cerebrovascular reserve capacity in patients with hemodynamic cerebral ischemia, defined using the strict selection criteria employed in this study.
Keyword
MeSH Terms
Figure
Reference
-
1. Yasargil MG. Microsurgery Applied to neurosurgery. 1969. Stuttgart: georg Thieme Verlag;105–115.2. The EC/IC Bypass study group. Failure of Extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. N Engl J Med. 1985. 313:1191–1120.3. Chollet F, Celsis P, Clanet M. SPECT study of cerebral blood flow reactivity after acetezolimide in patients with transient ischemic attacks. Stroke. 1988. 20:458–464.
Article4. Okudaira Y, Bandoh K, Arai H, Sato K. Evaluation of the acetazolamide test. Stroke. 1995. 26:1234–1239.
Article5. Schmideck P, Piepgras A, Leinsinger G, Kirsch CM, Einhaupl K. Improvement of cerebrovascular reserve capacity by EC-IC arterial bypass surgery in patients with ICA occlusion and hemodynamic cerebral ischemia. J Neurosurg. 1994. 81:236–244.
Article6. Hasegawa Y, Yamaguchi T, Tsuchiya T, Minematsu K, Nishimura T. Sequential change of ehmodynamic reserve in patients with major cerebral artery occlusion of severe stenosis. Neuroradiology. 1992. 34:15–21.
Article7. McCormick P, Tomecek F, McKinney J, Ausmane JI. Disabling cerebral transient ischemic attacks. J Neurosurg. 1991. 75:891–901.
Article8. Widder B, Kleiser B, Krapf H. Course of Cerebrovascular reactivity in patients with carotid artery occlusions. Stroke. 1994. 25:1963–1967.
Article9. Yonas H, Smith HA, Durham SR, Pentheny SL, Johnson DW. Increased stroke risk predicted by compromised cerebral blood flow reactivity. J Neurosurg. 1993. 79:483–489.
Article10. Anderson DE, Mclane MP, Reichman OH, Origitano TC. Improved cerebral blood flow and CO2 reactivity after microvascular anastomosis in patients at high risk for recurrent stroke. Neurosurgery. 1992. 31:26–34.
Article11. Batjer HH, Devous MD, Purdy PD. Improvement in regional blood flow and cerebral vasoreactivity after extracranialintracranial arterial bypass. Neurosurgery. 1988. 22:913–919.
Article12. Iwama T, Hashimoto N, Takagi Y, Tsukahara T, Hayashida K. Predictability of extraceanial/intracranial bypass function : a retrospective study of patients with occlussive cerebrovascular disease. Neurosurgery. 1997. 40:53–59.
Article13. Powers WJ, Grubb RL, Raichle ME. Clinical results of extracranial-intracranial bypass surgery in patients with hemodynamic cerebrovascular disease. J Neurosurg. 1898. 79:61–67.
Article14. Spetzler RF, Hadley MN. Wilkins RH, Rengachary SS, editors. Extracranial to intracranial bypass grafting. Neurosurgery. 1996. 2:ed 2. New York: McGRAW-Hill Health Professions Division;2157–2167.15. Vorstrup S, Brun B, Lassen NA. Evaluation of the cerebral vasodilatory capacity by the acetazolimide test before EC-IC bypass surgery in patients with carotid artery occlusions. Stroke. 1986. 17:1291–1298.
Article16. Yasui N, Suzuki A, Sayama I, Kawamura S, Shishido F, Uemura K. Comparison of the clinical results of STA-MCA anastomosis and the medical treatment in the cerebral low perfusion patients with viable brain tissue. Neurological Research. 1991. 13:84–88.
Article18. Rogers S, Sherman DG. Pathophysiology and treatment of acute ischemic stroke. Clinical Pharmacy. 1993. 12:359–373.19. Loftus CM, Biller J. Acute cerebral ischemia. Part II Surgical management. Contemporary Neurosurg. 1994. 16:1–6.20. Grubb RL, Powers WJ. Risks of stroke and current indications for cerebral revascularization in patients with carotid occlusion. Neurosurgery Clinics of North America. 2001. 36:473–485.
Article21. Eguchi T. How to select the candidate of Revascularization and How to evaluate the surgical benefit. J. Korean Neurosurg. 1998. 27:47–45.22. Korbling M, Estro Z. Adults Stem Cell for Tissue Repair-A new Therapeutic Concepts. The new England Journal of Medicine. 2003. 349:6570–582.23. Chen J, Sanberg PR, Li Y, Wang L, Lu M, Chopp M, et al. Intravenous Administration of Human Umbilical Cord Blood Reduces Behavioral Deficits After Stroke in Rats. Stroke. 2001. 32:2682–2688.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Off-Pump Coronary Artery Bypass Grafting in Moyamoya Disease
- Clinical Analysis of Arterial Bypass on the Atherosclerotic Occlusive Disease in Lower Extremities
- Current Indication of Extracranial-Intracranial Bypass Surgery
- The accidental renal artery embolism in patient with aortoiliac occlusive disease with unilateral renal atrophy during aortobifemoral bypass graft: A case report
- Surgical Treatment of Occlusive Cerebrovascular Disease