J Korean Foot Ankle Soc.
2014 Dec;18(4):173-177. 10.14193/jkfas.2014.18.4.173.
Characteristics of Severe Hallux Valgus Deformity with Moderate Intermetatarsal Angle
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yeungnam University College of Medicine, Daegu, Korea. chpark77@naver.com
- 2Department of Orthopaedic Surgery, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 3Department of Orthopaedic Surgery, MSR Hospital, Daegu, Korea.
- KMID: 2181637
- DOI: http://doi.org/10.14193/jkfas.2014.18.4.173
Abstract
- PURPOSE
The purpose of this study is to evaluate the characteristics of hallux valgus with severe hallux valgus angle (HVA) and moderate intermetatarsal angle (IMA) after proximal chevron osteotomy.
MATERIALS AND METHODS
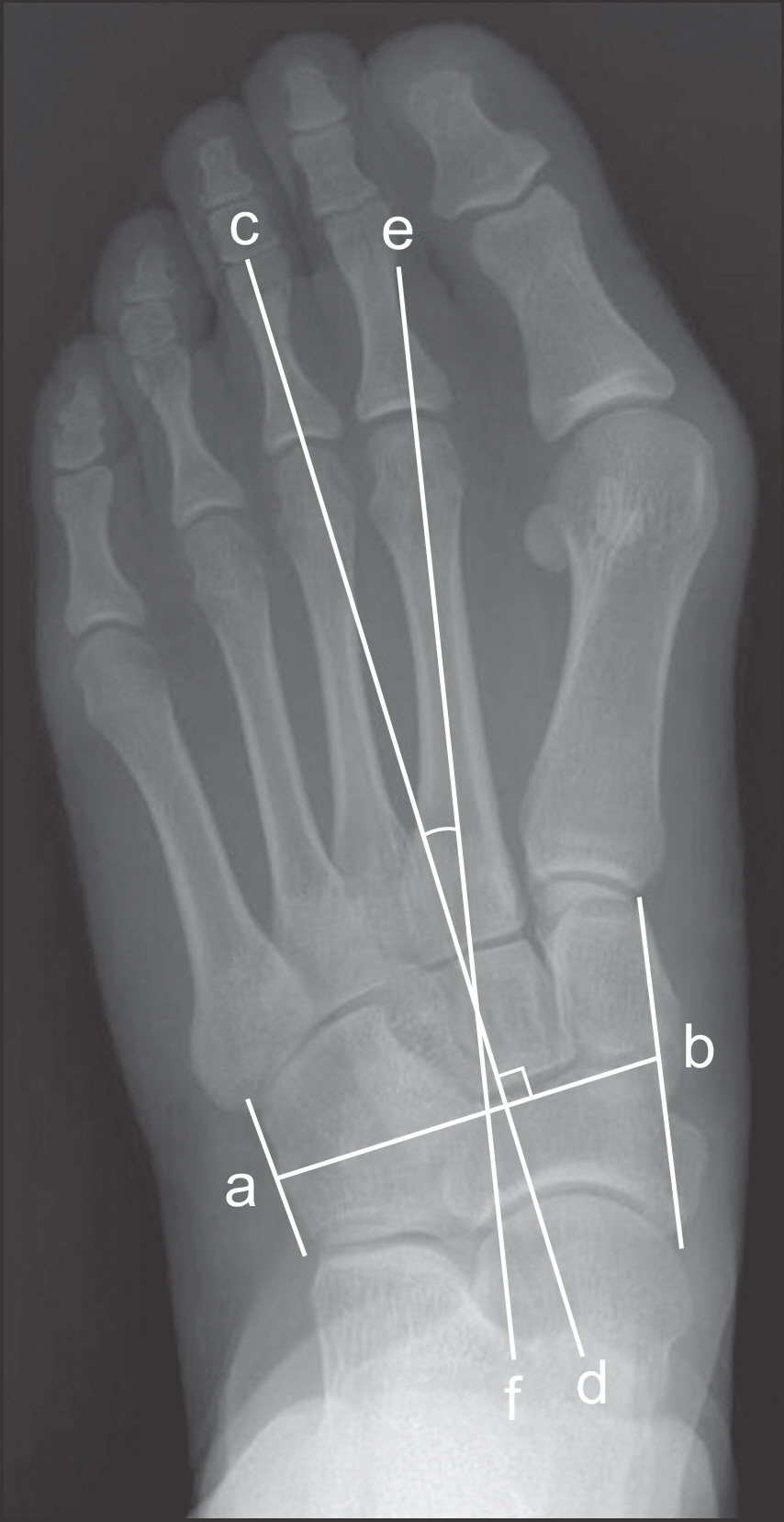
Between January 2008 and December 2010, 41 patients (48 feet) were treated with proximal chevron osteotomy and distal soft tissue procedure for symptomatic severe hallux valgus deformity (HVA > or =40degrees). Patients were divided into two groups, group M (IMA <18degrees) and group S (IMA > or =18degrees). Mean age of patients was 55.7 years (34~70 years) in group M and 60.0 years (44~78 years) in group S. Mean duration of follow-up was 20.4 months (12~41 months) in group M and 18.5 months (12~35 months) in group S. Radiographic parameters, including HVA, IMA, sesamoid position, metatarsus adductus angle (MAA), and distal metatarsal articular angle (DMAA), were compared between groups. Clinical results were assessed using American Orthopaedic Foot and Ankle Society (AOFAS) score and visual analogue scale (VAS). Recurrence rate at the last follow-up was compared between group M and group S.
RESULTS
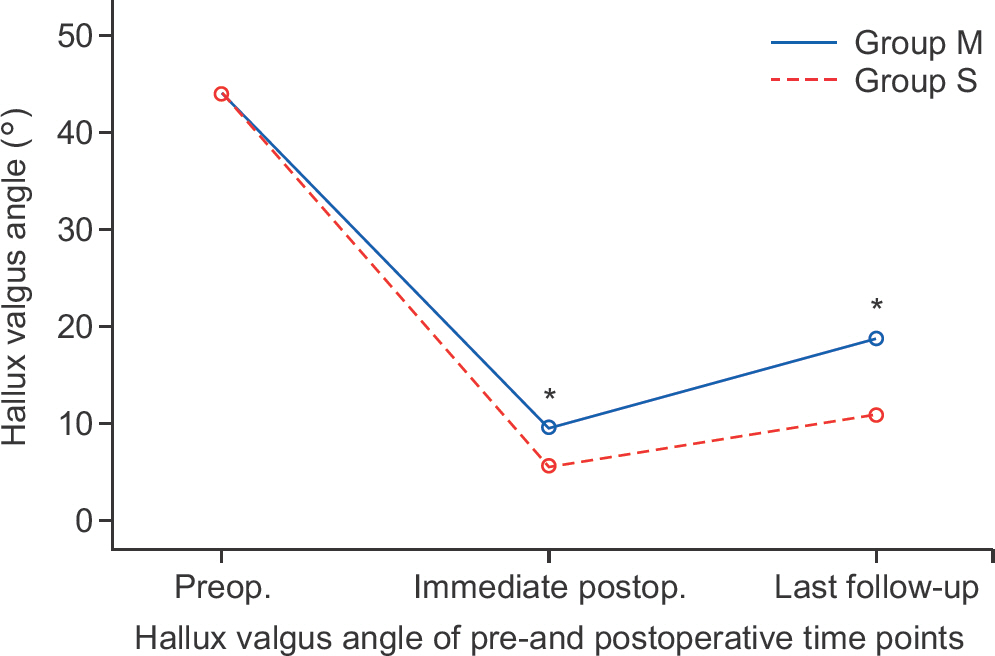
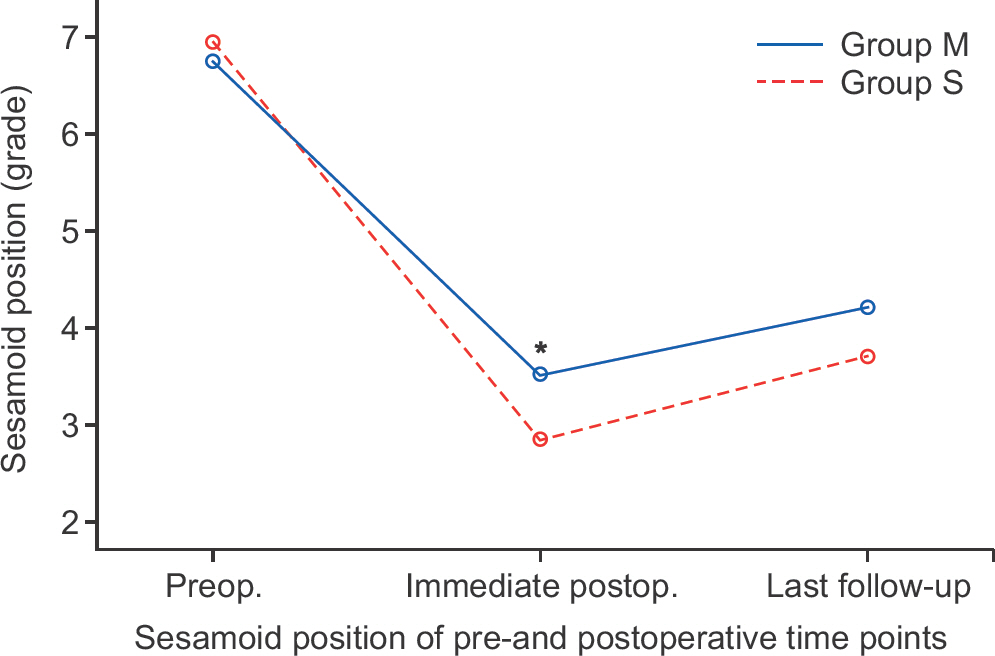
Preoperative HVA and grade of sesamoid position did not differ between the groups. However, immediate postoperative HVA and grade of sesamoid position were significantly larger in group M. Preoperative MAA and DMAA were significantly larger in group M. No significant difference in AOFAS score and VAS was observed between the groups at the last follow-up. Ten of the 27 feet (37.0%) in group M and two of the 21 feet (9.5%) in group S showed hallux valgus recurrence at the last follow-up. Group M showed a significantly higher recurrence rate than group S.
CONCLUSION
Recurrence rate for severe hallux valgus with moderate IMA is higher than that of severe hallux valgus with severe IMA.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Radiographic Risk Factors of Recurrent Hallux Valgus Deformity after Modified Scarf and Akin Osteotomy
Jae Wan Suh, Sung Hyun Kim, Hyun-Woo Park
J Korean Foot Ankle Soc. 2019;23(4):159-165. doi: 10.14193/jkfas.2019.23.4.159.When Do Clinical and Radiographic Results Stabilize after Proximal Chevron Osteotomy in Hallux Valgus?
Chul Hyun Park, Woo Chun Lee, Jae Woo Park, Jeong Jae Moon
J Korean Foot Ankle Soc. 2015;19(3):91-96. doi: 10.14193/jkfas.2015.19.3.91.
Reference
-
1.Easley ME., Trnka HJ. Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int. 2007. 28:748–58.
Article2.Easley ME., Trnka HJ. Current concepts review: hallux valgus part 1: pathomechanics, clinical assessment, and nonoperative management. Foot Ankle Int. 2007. 28:654–9.
Article3.Park CH., Jang JH., Lee SH., Lee WC. A comparison of proximal and distal chevron osteotomy for the correction of moderate hallux valgus deformity. Bone Joint J. 2013. 95:649–56.
Article4.Tanaka Y., Takakura Y., Kumai T., Sugimoto K., Taniguchi A., Hattori K. Proximal spherical metatarsal osteotomy for the foot with severe hallux valgus. Foot Ankle Int. 2008. 29:1025–30.
Article5.Hardy RH., Clapham JC. Observations on hallux valgus; based on a controlled series. J Bone Joint Surg Br. 1951. 33:376–91.6.Dawoodi AI., Perera A. Reliability of metatarsus adductus angle and correlation with hallux valgus. Foot Ankle Surg. 2012. 18:180–6.
Article7.Kitaoka HB., Alexander IJ., Adelaar RS., Nunley JA., Myerson MS., Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994. 15:349–53.
Article8.Markbreiter LA., Thompson FM. Proximal metatarsal osteotomy in hallux valgus correction: a comparison of crescentic and chevron procedures. Foot Ankle Int. 1997. 18:71–6.
Article9.Okuda R., Kinoshita M., Yasuda T., Jotoku T., Shima H. Proximal metatarsal osteotomy for hallux valgus: comparison of outcome for moderate and severe deformities. Foot Ankle Int. 2008. 29:664–70.
Article10.Schneider W., Knahr K. Metatarsophalangeal and intermetatarsal angle: different values and interpretation of postoperative results dependent on the technique of measurement. Foot Ankle Int. 1998. 19:532–6.
Article11.Zettl R., Trnka HJ., Easley M., Salzer M., Ritschl P. Moderate to se-vere hallux valgus deformity: correction with proximal crescentic osteotomy and distal soft-tissue release. Arch Orthop Trauma Surg. 2000. 120:397–402.
Article12.Coughlin MJ. Hallux valgus. J Bone Joint Surg Am. 1996. 78:932–66.13.Robinson AH., Limbers JP. Modern concepts in the treatment of hallux valgus. J Bone Joint Surg Br. 2005. 87:1038–45.
Article14.Thordarson D., Ebramzadeh E., Moorthy M., Lee J., Rudicel S. Correlation of hallux valgus surgical outcome with AOFAS forefoot score and radiological parameters. Foot Ankle Int. 2005. 26:122–7.
Article15.Thordarson DB., Ebramzadeh E., Rudicel SA., Baxter A. Age-adjusted baseline data for women with hallux valgus undergoing corrective surgery. J Bone Joint Surg Am. 2005. 87:66–75.
Article16.Bonnel F., Canovas F., Poirée G., Dusserre F., Vergnes C. Evaluation of the Scarf osteotomy in hallux valgus related to distal metatarsal articular angle: a prospective study of 79 operated cases. Rev Chir Orthop Reparatrice Appar Mot. 1999. 85:381–6.17.Pontious J., Mahan KT., Carter S. Characteristics of adolescent hallux abducto valgus. A retrospective review. J Am Podiatr Med Assoc. 1994. 84:208–18.
Article18.Larholt J., Kilmartin TE. Rotational scarf and akin osteotomy for correction of hallux valgus associated with metatarsus adductus. Foot Ankle Int. 2010. 31:220–8.
Article19.Kilmartin TE., O’Kane C. Correction of valgus second toe by closing wedge osteotomy of the proximal phalanx. Foot Ankle Int. 2007. 28:1260–4.
Article20.Okuda R., Kinoshita M., Yasuda T., Jotoku T., Kitano N., Shima H. Postoperative incomplete reduction of the sesamoids as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. 2009. 91:1637–45.
Article21.Veri JP., Pirani SP., Claridge R. Crescentic proximal metatarsal osteotomy for moderate to severe hallux valgus: a mean 12.2 year follow-up study. Foot Ankle Int. 2001. 22:817–22.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidence of Hallux Valgus Interphalangeus in the Normal and Hallux Valgus Feet and its Correlations with Hallux Valgus Angle and Intermetatarsal Angle
- Chevron Osteotomy as the Treatment of Moderate to Severe Hallux Valgus Deformity
- Treatment of Hallux Valgus with a Proximal Metatarsal Osteotomy and Distal Soft: Tissue Procedure
- Comparison of Proximal and Modified Distal Chevron Osteotomy for the Treatment of Moderate to Severe Hallux Valgus Deformity
- A Clinical Study of Chevron Osteotomy in Bunion - Hallux Valgus