J Gynecol Oncol.
2013 Oct;24(4):367-375. 10.3802/jgo.2013.24.4.367.
The correlates of unemployment and its association with quality of life in cervical cancer survivors
- Affiliations
-
- 1Department of Medical Science, Seoul National University College of Medicine, Seoul, Korea. lawyun@snu.ac.kr
- 2Department of Family Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 3Research Institute and Hospital, National Cancer Center, Goyang, Korea.
- 4Center for Uterine Cancer, National Cancer Center, Goyang, Korea.
- 5Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Department of Obstetrics and Gynecology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 7Department of Obstetrics and Gynecology, Gangnam CHA Hospital, CHA University College of Medicine, Seoul, Korea.
- 8Department of Obstetrics and Gynecology, Keimyung University School of Medicine, Daegu, Korea.
- 9Department of Obstetrics and Gynecology, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea.
- KMID: 2177879
- DOI: http://doi.org/10.3802/jgo.2013.24.4.367
Abstract
OBJECTIVE
Little is known regarding cervical cancer survivors' employment status, which represents social integration of cancer survivors as a pivotal domain of long-term quality of life. The goal of this study was to assess the correlates of unemployment and evaluate the impact on the comprehensive quality of life in cervical cancer survivors.
METHODS
We enrolled 858 cervical cancer survivors from the gynecologic oncology departments of multi-centers in Korea. Factors associated with unemployment were identified using multivariate logistic regression analyses. We assessed different health-related quality of life domains with multivariate-adjusted least-square means between cervical cancer survivors who currently work and do not.
RESULTS
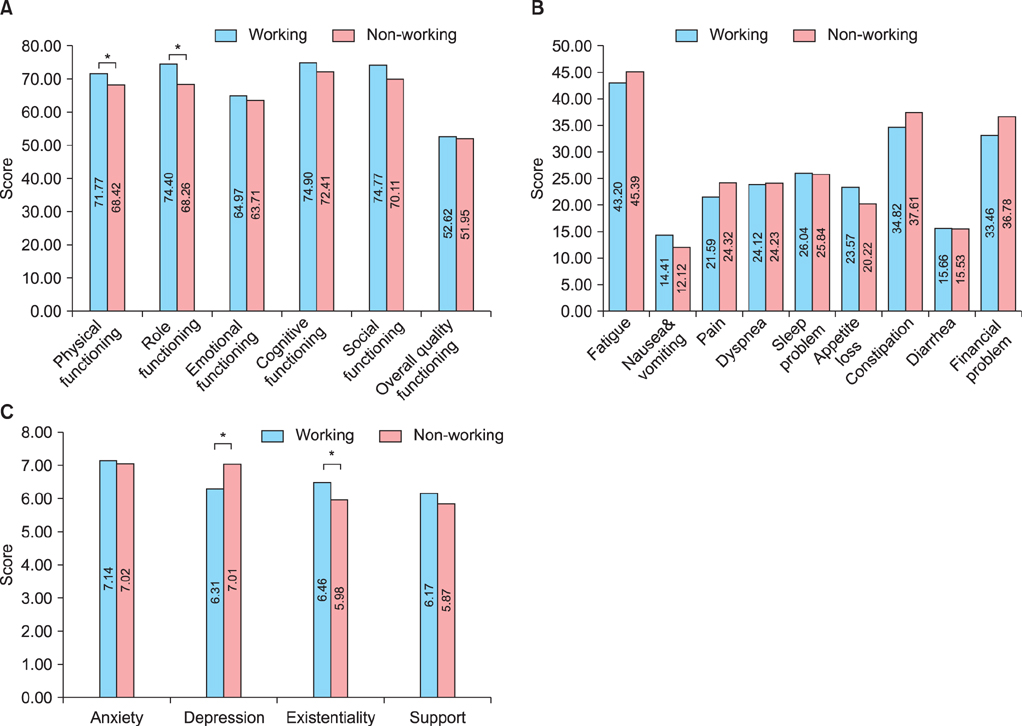
After diagnosis and treatment, the percentage of unemployed survivors increased from 50.6% to 72.8%. Lower income (adjusted odds ratio [aOR], 1.97; 95% confidence interval [CI], 1.38 to 2.81), medical aid (aOR, 1.58; 95% CI, 1.05 to 2.38), two or more comorbidities (aOR, 1.80; 95% CI, 1.12 to 2.90), current alcohol drinkers (aOR, 2.33; 95% CI, 1.54 to 3.52), and employed at the time of diagnosis (aOR, 10.72; 95% CI, 7.10 to 16.16) were significantly associated with unemployment. Non-working groups showed significant differences with respect to physical functioning, role functioning, depression, and existential well-being.
CONCLUSION
The proportion of unemployed cervical cancer survivors seems to increase, with low-income status and the presence of medical aid negatively being associated with employment, in addition to other comorbidities and previous working status. Effort should be made to secure the financial status of cervical cancer survivors.
MeSH Terms
Figure
Cited by 1 articles
-
Factors Affecting Postoperative Occupational Changes and Sick Leave in Patients with Thyroid Cancer
Kyung Ah Park, Young Ja Oh, Sang Hui Chu, Yong Sang Lee, Hang-Seok Chang, Cheong Soo Park
Int J Thyroidol. 2019;12(2):113-119. doi: 10.11106/ijt.2019.12.2.113.
Reference
-
1. Peteet JR. Cancer and the meaning of work. Gen Hosp Psychiatry. 2000; 22:200–205.2. Rasmussen DM, Elverdam B. The meaning of work and working life after cancer: an interview study. Psychooncology. 2008; 17:1232–1238.3. Bergman B, Sorenson S. Return to work among patients with small cell lung cancer. Eur J Respir Dis. 1987; 70:49–53.4. Rieker PP, Fitzgerald EM, Kalish LA, Richie JP, Lederman GS, Edbril SD, et al. Psychosocial factors, curative therapies, and behavioral outcomes: a comparison of testis cancer survivors and a control group of healthy men. Cancer. 1989; 64:2399–2407.5. Mols F, Thong MS, Vreugdenhil G, van de Poll-Franse LV. Long-term cancer survivors experience work changes after diagnosis: results of a population-based study. Psychooncology. 2009; 18:1252–1260.6. Taskila T, Lindbohm ML. Factors affecting cancer survivors' employment and work ability. Acta Oncol. 2007; 46:446–451.7. Bouknight RR, Bradley CJ, Luo Z. Correlates of return to work for breast cancer survivors. J Clin Oncol. 2006; 24:345–353.8. Nagarajan R, Neglia JP, Clohisy DR, Yasui Y, Greenberg M, Hudson M, et al. Education, employment, insurance, and marital status among 694 survivors of pediatric lower extremity bone tumors: a report from the childhood cancer survivor study. Cancer. 2003; 97:2554–2564.9. Torp S, Nielsen RA, Fossa SD, Gudbergsson SB, Dahl AA. Change in employment status of 5-year cancer survivors. Eur J Public Health. 2013; 23:116–122.10. Gudbergsson SB, Fossa SD, Dahl AA. Are there sex differences in the work ability of cancer survivors? Norwegian experiences from the NOCWO study. Support Care Cancer. 2011; 19:323–331.11. Drolet M, Maunsell E, Brisson J, Brisson C, Masse B, Deschenes L. Not working 3 years after breast cancer: predictors in a population-based study. J Clin Oncol. 2005; 23:8305–8312.12. Greimel E, Thiel I, Peintinger F, Cegnar I, Pongratz E. Prospective assessment of quality of life of female cancer patients. Gynecol Oncol. 2002; 85:140–147.13. Frazier LM, Miller VA, Horbelt DV, Delmore JE, Miller BE, Averett EP. Employment and quality of survivorship among women with cancer: domains not captured by quality of life instruments. Cancer Control. 2009; 16:57–65.14. Park SY, Bae DS, Nam JH, Park CT, Cho CH, Lee JM, et al. Quality of life and sexual problems in disease-free survivors of cervical cancer compared with the general population. Cancer. 2007; 110:2716–2725.15. Coates A, Porzsolt F, Osoba D. Quality of life in oncology practice: prognostic value of EORTC QLQ-C30 scores in patients with advanced malignancy. Eur J Cancer. 1997; 33:1025–1030.16. Yun YH, Park YS, Lee ES, Bang SM, Heo DS, Park SY, et al. Validation of the Korean version of the EORTC QLQ-C30. Qual Life Res. 2004; 13:863–868.17. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res. 2002; 52:69–77.18. Shim EJ, Hahm BJ. Anxiety, helplessness/hopelessness and desire for hastened death in Korean cancer patients. Eur J Cancer Care (Engl). 2011; 20:395–402.19. Kim SH, Gu SK, Yun YH, Lee CG, Choi YS, Lee WS, et al. Validation study of the Korean version of the McGill Quality of Life Questionnaire. Palliat Med. 2007; 21:441–447.20. Ahn E, Cho J, Shin DW, Park BW, Ahn SH, Noh DY, et al. Impact of breast cancer diagnosis and treatment on work-related life and factors affecting them. Breast Cancer Res Treat. 2009; 116:609–616.21. Park JH, Park EC, Park JH, Kim SG, Lee SY. Job loss and re-employment of cancer patients in Korean employees: a nationwide retrospective cohort study. J Clin Oncol. 2008; 26:1302–1309.22. Hoving JL, Broekhuizen ML, Frings-Dresen MH. Return to work of breast cancer survivors: a systematic review of intervention studies. BMC Cancer. 2009; 9:117.23. Greenwald HP, McCorkle R, Fennie K. Health status and adaptation among long-term cervical cancer survivors. Gynecol Oncol. 2008; 111:449–454.24. Nachreiner NM, Ghebre RG, Virnig BA, Shanley R. Early work patterns for gynaecological cancer survivors in the USA. Occup Med (Lond). 2012; 62:23–28.25. Wenzel L, DeAlba I, Habbal R, Kluhsman BC, Fairclough D, Krebs LU, et al. Quality of life in long-term cervical cancer survivors. Gynecol Oncol. 2005; 97:310–317.26. Taskila-Brandt T, Martikainen R, Virtanen SV, Pukkala E, Hietanen P, Lindbohm ML. The impact of education and occupation on the employment status of cancer survivors. Eur J Cancer. 2004; 40:2488–2493.27. Munir F, Yarker J, McDermott H. Employment and the common cancers: correlates of work ability during or following cancer treatment. Occup Med (Lond). 2009; 59:381–389.28. Beesley VL, Eakin EG, Janda M, Battistutta D. Gynecological cancer survivors' health behaviors and their associations with quality of life. Cancer Causes Control. 2008; 19:775–782.29. Grimmett C, Bridgewater J, Steptoe A, Wardle J. Lifestyle and quality of life in colorectal cancer survivors. Qual Life Res. 2011; 20:1237–1245.30. Bifulco G, De Rosa N, Tornesello ML, Piccoli R, Bertrando A, Lavitola G, et al. Quality of life, lifestyle behavior and employment experience: a comparison between young and midlife survivors of gynecology early stage cancers. Gynecol Oncol. 2012; 124:444–451.31. Mahar KK, BrintzenhofeSzoc K, Shields JJ. The impact of changes in employment status on psychosocial well-being: a study of breast cancer survivors. J Psychosoc Oncol. 2008; 26:1–17.32. Lee JI, Kim SH, Tan AH, Kim HK, Jang HW, Hur KY, et al. Decreased health-related quality of life in disease-free survivors of differentiated thyroid cancer in Korea. Health Qual Life Outcomes. 2010; 8:101.33. Glass J, Fujimoto T. Housework, paid work, and depression among husbands and wives. J Health Soc Behav. 1994; 35:179–191.34. Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004; 32:57–71.35. Steiner JF, Cavender TA, Nowels CT, Beaty BL, Bradley CJ, Fairclough DL, et al. The impact of physical and psychosocial factors on work characteristics after cancer. Psychooncology. 2008; 17:138–147.36. Ell K, Sanchez K, Vourlekis B, Lee PJ, Dwight-Johnson M, Lagomasino I, et al. Depression, correlates of depression, and receipt of depression care among low-income women with breast or gynecologic cancer. J Clin Oncol. 2005; 23:3052–3060.37. Shin HW, Noh DY, Lee ES, Nam SJ, Park BW, et al. Correlates of existential well-being and their association with health-related quality of life in breast cancer survivors compared with the general population. Breast Cancer Res Treat. 2009; 118:139–150.38. Kobayashi K, Morita S, Shimonagayoshi M, Kobayashi M, Fujiki Y, Uchida Y, et al. Effects of socioeconomic factors and cancer survivors' worries on their quality of life (QOL) in Japan. Psychooncology. 2008; 17:606–611.39. Spelten ER, Verbeek JH, Uitterhoeve AL, Ansink AC, van der Lelie J, de Reijke TM, et al. Cancer, fatigue and the return of patients to work-a prospective cohort study. Eur J Cancer. 2003; 39:1562–1567.40. Ross CE, Mirowsky J. Does employment affect health? J Health Soc Behav. 1995; 36:230–243.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Distress and Quality of Life in Breast Cancer Survivors in Korea
- Health-related Needs and Quality of Life in Childhood Cancer Survivors
- Colorectal Cancer Survivors' Inner Strength, Multiple Identities, and Quality of Life by Gender and Ostomy Presence: A Cross-Sectional Study
- Quality of Life and Associated Factor among Cancer Survivors in Korea
- Comparison of Quality of Life and Sexuality between Cervical Cancer Survivors and Healthy Women