J Cardiovasc Ultrasound.
2012 Dec;20(4):181-188. 10.4250/jcu.2012.20.4.181.
Evaluation of Right Ventricular Systolic Function by the Analysis of Tricuspid Annular Motion in Patients with Acute Pulmonary Embolism
- Affiliations
-
- 1Department of Cardiology in Internal Medicine, School of Medicine, Chungnam National University, Chungnam National University Hospital, Daejeon, Korea. siwanc@cnu.ac.kr
- KMID: 2177405
- DOI: http://doi.org/10.4250/jcu.2012.20.4.181
Abstract
- BACKGROUND
Measurement of right ventricular (RV) systolic function is important for patients with acute pulmonary embolism (PE). However, assessment of RV function is a challenge due to its complex anatomy. We measured RV systolic function with analysis of tricuspid annular motion in acute PE patients.
METHODS
From August 2007 to May 2011, all consecutive PE patients were prospectively included. Tricuspid annular motion was analyzed with tricuspid annular plane systolic excursion (TAPSE) and tricuspid annular systolic velocity (TASV).
RESULTS
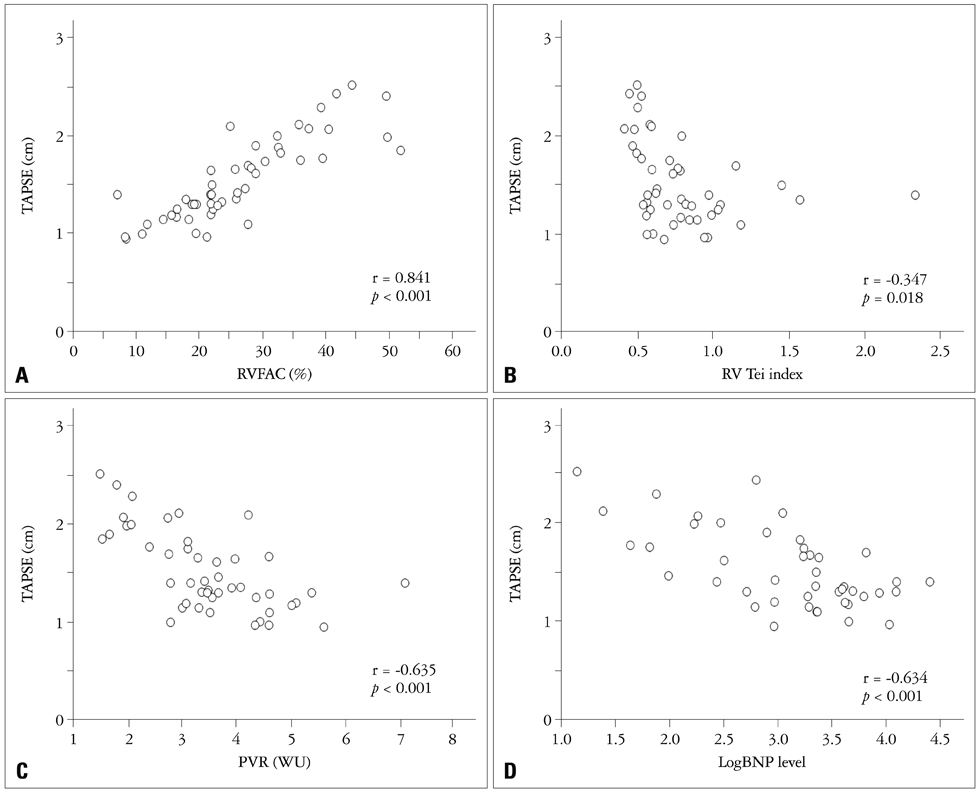
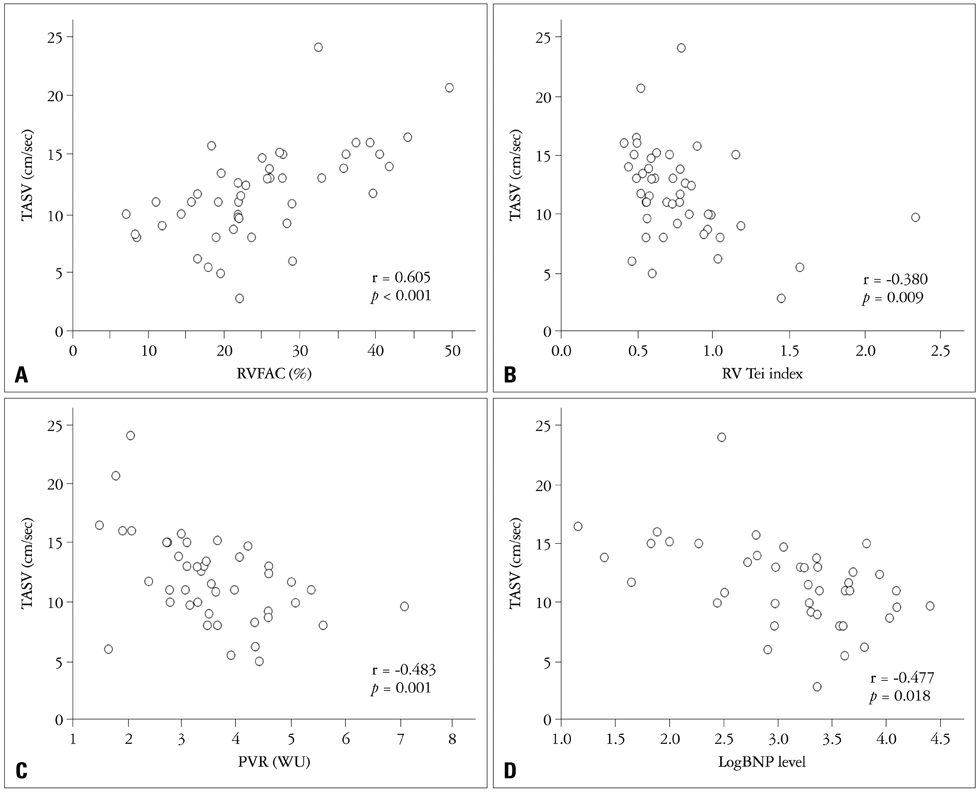
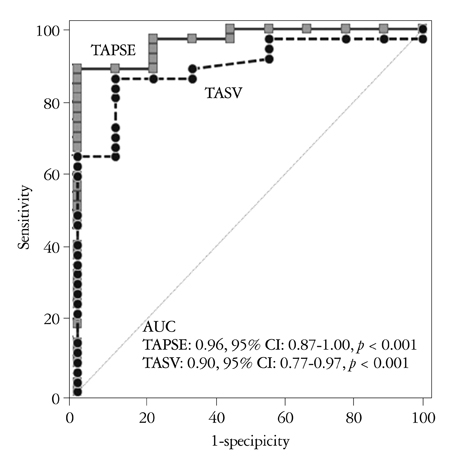
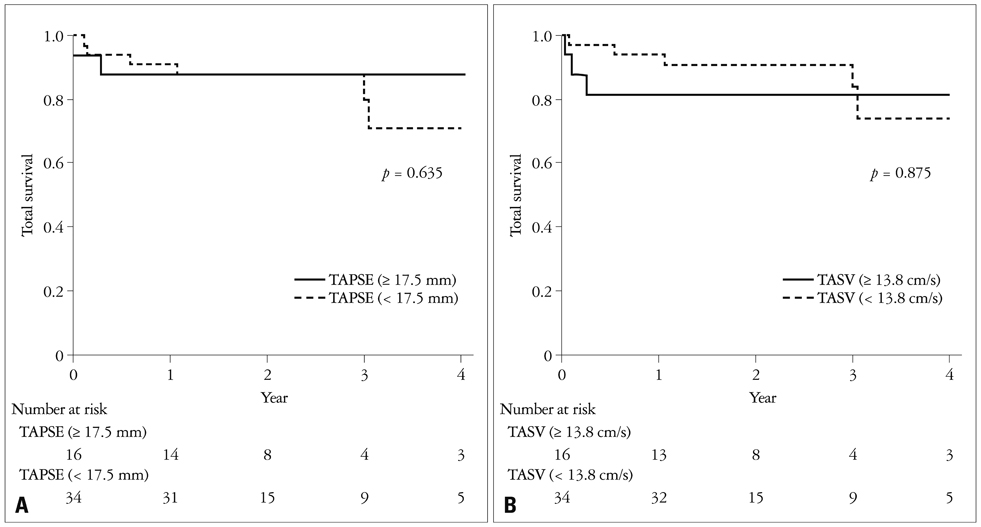
We analyzed total 50 patients (38 females, 68 +/- 14 years). Mean RV fractional area change (RVFAC) was 26.2 +/- 10.8%; RV Tei index 0.78 +/- 0.35; TR Vmax 3.8 +/- 0.5 m/sec; pulmonary vascular resistance (PVR) 3.5 +/- 1.2 WU. TAPSE was 16 +/- 4 mm and TASV was 11.7 +/- 4.0 cm/sec. TAPSE showed significant correlations with RVFAC (r = 0.841, p < 0.001), RV Tei index (r = -0.347, p = 0.018), Log B-type natriuretic peptide (BNP) (r = -0.634, p < 0.001) and PVR (r = -0.635, p < 0.001). TASV also revealed significant correlations with RVFAC (r = 0.605, p < 0.001), RV Tei index (r = -0.380, p = 0.009), LogBNP (r = -0.477, p = 0.001) and PVR (r = -0.483, p = 0.001). The best cutoff of TAPSE for detection of RV systolic dysfunction (defined as RVFAC < 35%) was 1.75 cm [Areas under the curve (AUC) = 0.96, p < 0.001] with a sensitivity of 87% and specificity 91%. The best cutoff for TASV was 13.8 cm/sec (AUC = 0.90, p < 0.001), sensitivity 86% and specificity 78%. However, there was no statistical significance in the detection of RV dysfunction (difference = 0.07, 95% CI = -0.21-0.17, p = 0.130) between TAPSE and TASV.
CONCLUSION
TAPSE and TASV showed significant correlations with conventional echocardiographic parameters of RV function and LogBNP value. These values can be used to detect RV systolic dysfunction more easily in patients with acute PE.
MeSH Terms
Figure
Cited by 1 articles
-
A Comparison of Different Techniques of Two-Dimensional Speckle-Tracking Strain Measurements of Right Ventricular Systolic Function in Patients with Acute Pulmonary Embolism
Jae-Hwan Lee, Jae-Hyeong Park, Kwang-In Park, Mi Joo Kim, Jun Hyung Kim, Moon Sang Ahn, Si Wan Choi, Jin-Ok Jeong, In-Whan Seong
J Cardiovasc Ultrasound. 2014;22(2):65-71. doi: 10.4250/jcu.2014.22.2.65.
Reference
-
1. Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P, Bengel F, Brady AJ, Ferreira D, Janssens U, Klepetko W, Mayer E, Remy-Jardin M, Bassand JP. ESC Committee for Practice Guidelines (CPG). Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur Heart J. 2008. 29:2276–2315.2. Kucher N, Rossi E, De Rosa M, Goldhaber SZ. Prognostic role of echocardiography among patients with acute pulmonary embolism and a systolic arterial pressure of 90 mm Hg or higher. Arch Intern Med. 2005. 165:1777–1781.
Article3. Grifoni S, Olivotto I, Cecchini P, Pieralli F, Camaiti A, Santoro G, Conti A, Agnelli G, Berni G. Short-term clinical outcome of patients with acute pulmonary embolism, normal blood pressure, and echocardiographic right ventricular dysfunction. Circulation. 2000. 101:2817–2822.
Article4. Dell'Italia LJ. The right ventricle: anatomy, physiology, and clinical importance. Curr Probl Cardiol. 1991. 16:653–720.5. Tandri H, Daya SK, Nasir K, Bomma C, Lima JA, Calkins H, Bluemke DA. Normal reference values for the adult right ventricle by magnetic resonance imaging. Am J Cardiol. 2006. 98:1660–1664.
Article6. Cresci SG, Goldstein JA. Hemodynamic manifestations of ischemic right heart dysfunction. Cathet Cardiovasc Diagn. 1992. 27:28–33. discussion 33-4.
Article7. Kaul S, Tei C, Hopkins JM, Shah PM. Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J. 1984. 107:526–531.
Article8. Ueti OM, Camargo EE, Ueti Ade A, de Lima-Filho EC, Nogueira EA. Assessment of right ventricular function with Doppler echocardiographic indices derived from tricuspid annular motion: comparison with radionuclide angiography. Heart. 2002. 88:244–248.
Article9. Meluzín J, Spinarová L, Bakala J, Toman J, Krejcí J, Hude P, Kára T, Soucek M. Pulsed Doppler tissue imaging of the velocity of tricuspid annular systolic motion; a new, rapid, and non-invasive method of evaluating right ventricular systolic function. Eur Heart J. 2001. 22:340–348.
Article10. Saxena N, Rajagopalan N, Edelman K, López-Candales A. Tricuspid annular systolic velocity: a useful measurement in determining right ventricular systolic function regardless of pulmonary artery pressures. Echocardiography. 2006. 23:750–755.
Article11. Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010. 23:685–713. quiz 786-8.
Article12. Grapsa J, Dawson D, Nihoyannopoulos P. Assessment of right ventricular structure and function in pulmonary hypertension. J Cardiovasc Ultrasound. 2011. 19:115–125.
Article13. Abbas AE, Fortuin FD, Schiller NB, Appleton CP, Moreno CA, Lester SJ. A simple method for noninvasive estimation of pulmonary vascular resistance. J Am Coll Cardiol. 2003. 41:1021–1027.
Article14. McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, Lee RT. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol. 1996. 78:469–473.
Article15. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982. 143:29–36.
Article16. Wood KE. Major pulmonary embolism: review of a pathophysiologic approach to the golden hour of hemodynamically significant pulmonary embolism. Chest. 2002. 121:877–905.17. McIntyre KM, Sasahara AA. The hemodynamic response to pulmonary embolism in patients without prior cardiopulmonary disease. Am J Cardiol. 1971. 28:288–294.
Article18. Leibowitz D. Role of echocardiography in the diagnosis and treatment of acute pulmonary thromboembolism. J Am Soc Echocardiogr. 2001. 14:921–926.
Article19. Di Salvo TG, Mathier M, Semigran MJ, Dec GW. Preserved right ventricular ejection fraction predicts exercise capacity and survival in advanced heart failure. J Am Coll Cardiol. 1995. 25:1143–1153.
Article20. Nass N, McConnell MV, Goldhaber SZ, Chyu S, Solomon SD. Recovery of regional right ventricular function after thrombolysis for pulmonary embolism. Am J Cardiol. 1999. 83:804–806. A10
Article21. Rydman R, Söderberg M, Larsen F, Caidahl K, Alam M. Echocardiographic evaluation of right ventricular function in patients with acute pulmonary embolism: a study using tricuspid annular motion. Echocardiography. 2010. 27:286–293.
Article22. Carson JL, Kelley MA, Duff A, Weg JG, Fulkerson WJ, Palevsky HI, Schwartz JS, Thompson BT, Popovich J Jr, Hobbins TE, et al. The clinical course of pulmonary embolism. N Engl J Med. 1992. 326:1240–1245.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usability consideration about mitral annular plane systolic excursion (MAPSE) and tricuspid annular plane systolic excursion (TAPSE) with point of care ultrasound (POCUS) in emergency: untact pilot experiment before clinically applying them in emergency room
- Assessment of Right Ventricular Systolic Function: Conventional Methods and Modified Tricuspid Annular Plane Systolic Excursion
- Quantitative Evaluation of Right-Ventricular Function in Patients with Tricuspid Regurgitation
- Modified Tricuspid Annular Plane Systolic Excursion for Assessment of Right Ventricular Systolic Function
- Pulmonary Thromboembolism and Infarction Caused by Right-Sided Infective Endocarditis in a Patient with Ventricular Septal Defect