J Breast Cancer.
2007 Mar;10(1):85-89. 10.4048/jbc.2007.10.1.85.
The Clinical and, Pathologic Risk Factors for Local Recurrence of Phyllodes Tumor
- Affiliations
-
- 1Department of Surgery, Kosin University Medical School, Busan, Korea. surgery@ns.kosinmed.or.kr
- KMID: 2175005
- DOI: http://doi.org/10.4048/jbc.2007.10.1.85
Abstract
-
PURPOSE: Phyllodes tumors of the breast are biphasic neoplasms. They are composed of epithelium and a spindle cell stroma. However, there is some controversy over its clinical behavior, pathologic characteristics, and local recurrence rates. Therefore we analyzed the clinicopathological characteristics of phyllodes tumor and the risk factor that influence a local recurrence after surgery were analyzed.
METHODS
We retrospectively analyzed the medical records of 73 patients with a phyllodes tumor and who had undergone surgery at the Department of Surgery, Kosin University, from 1994 to 2005. The median follow up period was 73 months (range: 5-250 months). The microscopic slides were re-examined and the pathologic criteria we analyzed were cellular atypia, stromal cellularity, pleomorphism, necrosis, differentiation, the tumor margin, and the number of mitosis. The malignancy was reclassifed using the histological criteria reported by Pietruszka et at. (benign was 0-4 mitoses/10 highpower folds, borderline 5-9 mitoses, and malignant was more than 10 mitoses), The clinical features we evaluated included age, the preoperative diagnosis, the tumor size, surgical methods, and local recurrence.
RESULTS
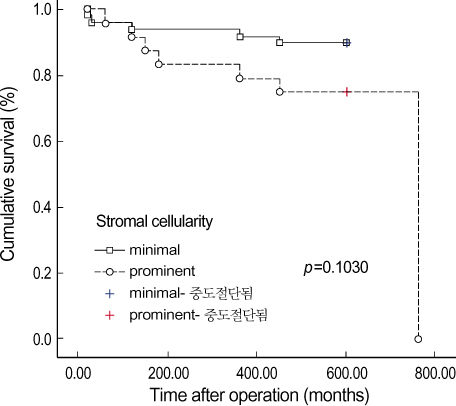
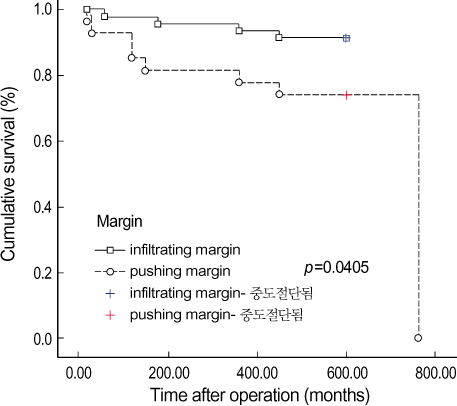
The mean age was 38.2 yr (range: 15-60 yr) and the mean tumor size was 4.3 cm (range: 1.6-18 cm), The most commonly performed surgical procedures were local or wide excision (60 cases, 82.2%), mastectomy in 10 cases (13.7%) and MRM in 3 cases (4.1%). Out of the 73 cases we reviewed, 49 (67.1%) were confirmed as being a benign, 3 (4.1%) were borderline, and 21 (28.7%) were malignant phyllodes tumor. Cellular atypia was minimal in 55 cases (75.3%) and it was prominent in 18 cases (24.6%). The stromal cellularity was minimal in 49 cases (67.1%) and it was prominent in 24 cases (32.8%). The tumor margin was infiltrating in 27 cases (36.9%) and pushing in 46 cases (63.0%). A local recurrence developed in 12 cases (16.4%). There were no dependable histopathological features to predict a local recurrence except for stromal cellularity, and an infiltrating margin.
CONCLUSION
From the above results, the strong prognostic factors that can be used to predict a local recurrence appear to be stromal cellularity, and an infiltrating tumor margin.
Keyword
MeSH Terms
Figure
Reference
-
1. Ko SS, Kim SK, Kim SI, Park BB, Yang WI, Lee KS. Risk factors of local recurrence in phyllodes tumor. J Korean Surg Soc. 2002. 63:378–383.2. Auger M, Hanna W, Kahn HJ. Cystsarcoma phyllodes of the breast and its mimics: an immunohistochemical and ultrastructural study. Arch Pathol Lab Med. 1989. 113:1231–1235.3. Kim HJ, Kim TS, Kang HJ, Cho JC, Park IA, Noh DY, et al. Clinical analysis of phyllodes tumor of the breast. J Korean Surg Soc. 2000. 58:352–360.4. Kleer CG, Giordano TJ, Braun T, Oberman H. Pathologic immunological, and molecular features of benign and malignant phyllodes tumors of the breast. Mod Pathol. 2001. 13:185–190.5. Vorherr H, Vorherr UF, Kutvirt DM, Key CR. Cystosarcoma phyllodes: Epidemiology, pathohistology, pathobiology, diagnosis, therapy, and survival. Arch Gynecol. 1985. 236:173–181.
Article6. Noh DY, Kim SJ, Choe KJ, Kim JP, Kim WH. Malignant cystosarcoma phyllodes. J Korean Cancer Assoc. 1992. 24:730–736.7. Kim SN, Kim WH, Lee SK. Pathologic analysis of 15 cases of phyllodes tumors of the breast. Korean J Pathol. 1993. 27:19–26.8. Piertruska M, Barnes L. Cystsarcoma phyllodes: a clinicopathologic analysis of 42 cases. Cancer. 1978. 41:1974–1983.9. Norris HJ, Taylor HB. Relationship of histologic features to behavior of cystosarcoma phyllodes. Cancer. 1967. 20:2090–2099.
Article10. Lindquist KD, Van Heerden JA, Welland LH, Martin JK. Recunent and metastatic cystosarcoma phyllodes. Am J Surg. 1982. 144:341–343.11. Kim CJ, Kim WH. Pattern of p53 expression in phyllodes tumors of the breast: an immunohistochemical study. J Korean Med Sci. 1993. 8:325–328.
Article12. Hines JR, Murad TM, Beal JM. Prognostic indicutors in cystosarcoma phylloides. Am J Surg. 1987. 153:276–280.13. Noguchi S, Aihara T, Motomura K, Inaji H, Imaoka S, Koyama H, et al. Phyllodes tumor of the breast: pathology, histogenesis, diagnosis, and treatment. Breast Cancer. 1996. 3:79–92.
Article14. Rajan PB, Cranor ML, Rosen PP. Cystosarcona phyllodes in adolescent girls and young women: a study of 45 patients. Am J Surg Pathol. 1998. 22:64–69.15. Lester J, Scout AP. Cystsarcoma phyllodes. Cancer. 1954. 7:335–353.16. Browder W, McQuitty JT Jr, McDonald JC. Malignant cystosarcoma phylloides. Treatment and prognosis. Am J Surg. 1978. 136:239–241.17. Cohn-Cedermark G, Rutqvist LE, Rosendahl I, Silfversward C. Prognostic factors in cystosarcoma phyllodes. A clinicopathologic study of 77 patients. Cancer. 1991. 68:2017–2022.
Article18. Buchberger W, Strasser K, Heim K, Muller E, Schrocksnadel H. Phyllodes tumor: finding on mammography, sonography, and aspiration cytology in 10 cases. AJR. 1991. 157:715–719.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors of Local Recurrence in Phyllodes Tumor of the Breast according to the Clinicopathological Characteristics
- Risk Factors of Local Recurrence in Phyllodes Tumor
- Clinical and Histopathological Correlations of Phyllodes Tumors of the Breast
- DNA Ploidy Analysis as a Prognostic Indicator in Phyllodes Tumor of the Breast
- Sonographic Features of Phyllodes Tumors of the Breast: A Pictorial Review