Intest Res.
2014 Oct;12(4):299-305. 10.5217/ir.2014.12.4.299.
Long-Term Clinical Outcome of Clostridium difficile Infection in Hospitalized Patients: A Single Center Study
- Affiliations
-
- 1Department of Internal Medicine, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea. yousunk69@korea.com
- 2Department ofSurgery, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- KMID: 2174407
- DOI: http://doi.org/10.5217/ir.2014.12.4.299
Abstract
- BACKGROUND/AIMS
Antibiotic usage and increasingly aging populations have led to increased incidence of Clostridium difficile infection (CDI) in worldwide. Recent studies in Korea have also reported increasing CDI incidence; however, there have been no reports on the long-term outcomes of CDI. We therefore investigated the long-term clinical outcomes of patients with CDI, including delayed recurrence, associated risk factors and mortality.
METHODS
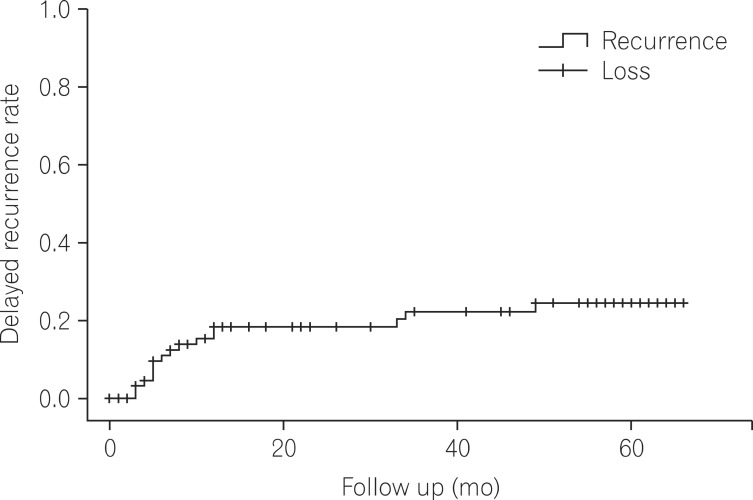
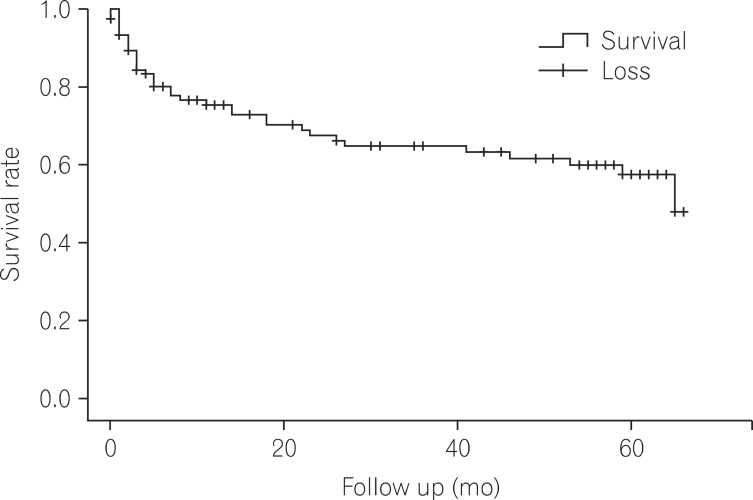
Hospitalized patients diagnosed with CDI at Seoul Paik Hospital between January 2007 and December 2008 were included. Their medical records were retrospectively investigated. 'Delayed recurrence' was defined as a relapse 8 weeks after a successful initial treatment. Multivariate logistic regression analysis was performed to identify risk factors for the delayed recurrence. Kaplan-Meier curves were used to analyze mortality rates.
RESULTS
A total of 120 patients were enrolled; among them, 87 were followed-up for at least 1 year, with a mean follow-up period of 34.1+/-25.1 months. Delayed recurrence was observed in 17 patients (19.5%), and significant risk factors were age (over 70 years, P=0.049), nasogastric tube insertion (P=0.008), and proton pump inhibitor or H2-blocker treatments (P=0.028). The 12- and 24-month mortality rates were 24.6% and 32.5%, respectively. No deaths were directly attributed to CDI.
CONCLUSIONS
Delayed recurrence of CDI was not rare, occurring in 19.5% of the study population. Although CDI-related mortality was not reported, 2-year (32.5%) mortality rate of CDI patients implies that a CDI diagnosis may predict severe morbidity and poor prognosis of the underlying disease.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Rapid and accurate diagnosis of
Clostridium difficile infection by real-time polymerase chain reaction
Pil Hun Song, Jung Hwa Min, You Sun Kim, Soo Yeon Jo, Eun Jin Kim, Kyung Jin Lee, Jeonghun Lee, Hyun Sung, Jeong Seop Moon, Dong Hee Whang
Intest Res. 2018;16(1):109-115. doi: 10.5217/ir.2018.16.1.109.Risk Factors for Delayed Recurrence of
Clostridium difficile Infection
Ji Won Kim
Intest Res. 2014;12(4):266-267. doi: 10.5217/ir.2014.12.4.266.
Reference
-
1. Ricciardi R, Rothenberger DA, Madoff RD, Baxter NN. Increasing prevalence and severity of Clostridium difficile colitis in hospitalized patients in the United States. Arch Surg. 2007; 142:624–631. PMID: 17638799.
Article2. Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010; 31:431–455. PMID: 20307191.
Article3. Lee JK, Cho JY, Kim YS, et al. Comparative value of sigmoidoscopy and stool cytotoxin-A assay for diagnosis of pseudomembranous colitis. Intest Res. 2005; 3:61–67.4. Pepin J, Alary ME, Valiquette L, et al. Increasing risk of relapse after treatment of Clostridium difficile colitis in Quebec, Canada. Clin Infect Dis. 2005; 40:1591–1597. PMID: 15889355.
Article5. Jawa RS, Mercer DW. Clostridium difficile-associated infection: a disease of varying severity. Am J Surg. 2012; 204:836–842. PMID: 23036604.
Article6. Wenisch JM, Schmid D, Tucek G, et al. A prospective cohort study on hospital mortality due to Clostridium difficile infection. Infection. 2012; 40:479–484. PMID: 22527876.
Article7. Bloomfield MG, Sherwin JC, Gkrania-Klotsas E. Risk factors for mortality in Clostridium difficile infection in the general hospital population: a systematic review. J Hosp Infect. 2012; 82:1–12. PMID: 22727824.8. Warny M, Pepin J, Fang A, et al. Toxin production by an emerging strain of Clostridium difficile associated with outbreaks of severe disease in North America and Europe. Lancet. 2005; 366:1079–1084. PMID: 16182895.
Article9. Diggs NG, Surawicz CM. Evolving concepts in Clostridium difficile colitis. Curr Gastroenterol Rep. 2009; 11:400–405. PMID: 19765368.10. Miller M, Gravel D, Mulvey M, et al. Health care-associated Clostridium difficile infection in Canada: patient age and infecting strain type are highly predictive of severe outcome and mortality. Clin Infect Dis. 2010; 50:194–201. PMID: 20025526.
Article11. Musher DM, Aslam S, Logan N, et al. Relatively poor outcome after treatment of Clostridium difficile colitis with metronidazole. Clin Infect Dis. 2005; 40:1586–1590. PMID: 15889354.
Article12. Kim YS, Han DS, Kim YH, et al. Incidence and clinical features of Clostridium difficile infection in Korea: a nationwide study. Epidemiol Infect. 2013; 141:189–194. PMID: 22717061.
Article13. Lee JH, Lee SY, Kim YS, et al. The incidence and clinical features of Clostridium difficile infection; single center study. Korean J Gastroenterol. 2010; 55:175–182. PMID: 20357528.
Article14. Ryu HS, Kim YS, Seo GS, Lee YM, Choi SC. Risk factors for recurrent Clostridium difficile infection. Intest Res. 2012; 10:176–182.
Article15. Choi HK, Kim KH, Lee SH, Lee SJ. Risk factors for recurrence of Clostridium difficile infection: effect of vancomycin-resistant enterococci colonization. J Korean Med Sci. 2011; 26:859–864. PMID: 21738336.
Article16. Jung KS, Park JJ, Chon YE, et al. Risk factors for treatment failure and recurrence after metronidazole treatment for Clostridium difficile-associated diarrhea. Gut Liver. 2010; 4:332–337. PMID: 20981209.
Article17. Tae CH, Jung SA, Song HJ, et al. The first case of antibiotic-associated colitis by Clostridium difficile PCR ribotype 027 in Korea. J Korean Med Sci. 2009; 24:520–524. PMID: 19543521.
Article18. Kim J, Kang JO, Kim H, et al. Epidemiology of Clostridium difficile infections in a tertiary-care hospital in Korea. Clin Microbiol Infect. 2013; 19:521–527. PMID: 22712697.
Article19. McFarland LV, Surawicz CM, Greenberg RN, et al. A randomized placebo-controlled trial of Saccharomyces boulardii in combination with standard antibiotics for Clostridium difficile disease. JAMA. 1994; 271:1913–1918. PMID: 8201735.
Article20. McFarland LV, Surawicz CM, Rubin M, Fekety R, Elmer GW, Greenberg RN. Recurrent Clostridium difficile disease: epidemiology and clinical characteristics. Infect Control Hosp Epidemiol. 1999; 20:43–50. PMID: 9927265.
Article21. Gerding DN. Treatment of Clostridium difficile-associated diarrhea and colitis. Curr Top Microbiol Immunol. 2000; 250:127–139. PMID: 10981361.22. Barbut F, Richard A, Hamadi K, Chomette V, Burghoffer B, Petit JC. Epidemiology of recurrences or reinfections of Clostridium difficile-associated diarrhea. J Clin Microbiol. 2000; 38:2386–2388. PMID: 10835010.
Article23. Bauer MP, Notermans DW, van Benthem BH, et al. Clostridium difficile infection in Europe: a hospital-based survey. Lancet. 2011; 377:63–73. PMID: 21084111.24. Seo GS. Clostridium difficile infection: what's new? Intest Res. 2013; 11:1–13.25. Musher DM, Nuila F, Logan N. The long-term outcome of treatment of Clostridium difficile colitis. Clin Infect Dis. 2007; 45:523–524. PMID: 17638211.26. Garey KW, Sethi S, Yadav Y, DuPont HL. Meta-analysis to assess risk factors for recurrent Clostridium difficile infection. J Hosp Infect. 2008; 70:298–304. PMID: 18951661.27. Johnson S. Recurrent Clostridium difficile infection: a review of risk factors, treatments, and outcomes. J Infect. 2009; 58:403–410. PMID: 19394704.
Article28. Pepin J, Valiquette L, Alary ME, et al. Clostridium difficile-associated diarrhea in a region of Quebec from 1991 to 2003: a changing pattern of disease severity. CMAJ. 2004; 171:466–472. PMID: 15337727.
Article29. O'Connor JR, Johnson S, Gerding DN. Clostridium difficile infection caused by the epidemic BI/NAP1/027 strain. Gastroenterology. 2009; 136:1913–1924. PMID: 19457419.30. Kim H, Jeong SH, Roh KH, et al. Investigation of toxin gene diversity, molecular epidemiology, and antimicrobial resistance of Clostridium difficile isolated from 12 hospitals in South Korea. Korean J Lab Med. 2010; 30:491–497. PMID: 20890081.
Article31. Kim J, Pai H, Seo MR, Kang JO. Epidemiology and clinical characteristics of Clostridium difficile infection in a Korean tertiary hospital. J Korean Med Sci. 2011; 26:1258–1264. PMID: 22022175.
Article32. Walters BA, Roberts R, Stafford R, Seneviratne E. Relapse of antibiotic associated colitis: endogenous persistence of Clostridium difficile during vancomycin therapy. Gut. 1983; 24:206–212. PMID: 6826104.
Article33. Tedesco FJ, Gordon D, Fortson WC. Approach to patients with multiple relapses of antibiotic-associated pseudomembranous colitis. Am J Gastroenterol. 1985; 80:867–868. PMID: 4050760.34. Wilcox MH, Fawley WN, Settle CD, Davidson A. Recurrence of symptoms in Clostridium difficile infection--relapse or reinfection? J Hosp Infect. 1998; 38:93–100. PMID: 9522287.
Article35. O'Neill GL, Beaman MH, Riley TV. Relapse versus reinfection with Clostridium difficile. Epidemiol Infect. 1991; 107:627–635. PMID: 1752311.36. Maroo S, Lamont JT. Recurrent Clostridium difficile. Gastroenterology. 2006; 130:1311–1316. PMID: 16618421.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clostridium difficile Infection: What's New?
- Clostridium difficile Infection: A Worldwide Disease
- A Case of Reactive Arthritis in a Patient with Clostridium Difficile Diarrhea
- New Treatment Option for Recurrent Clostridium difficile Infection
- Clinical Characterization of Clostridium difficile Infection in Elderly Patients