Dement Neurocogn Disord.
2012 Jun;11(2):74-77. 10.12779/dnd.2012.11.2.74.
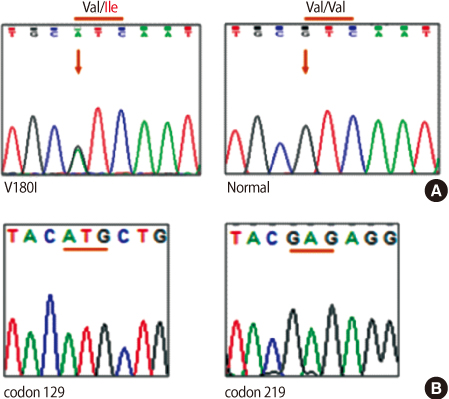
A Case of Familial Creutzfeldt-Jacob Disease (V180I) Initially Presenting with Depression
- Affiliations
-
- 1Department of Neurology, Veterans hospital, Seoul Medical Center, Seoul, Korea. astro76@naver.com
- KMID: 2172239
- DOI: http://doi.org/10.12779/dnd.2012.11.2.74
Abstract
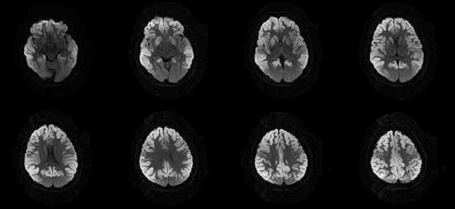
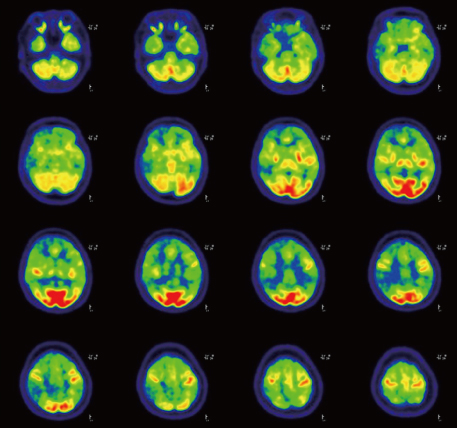
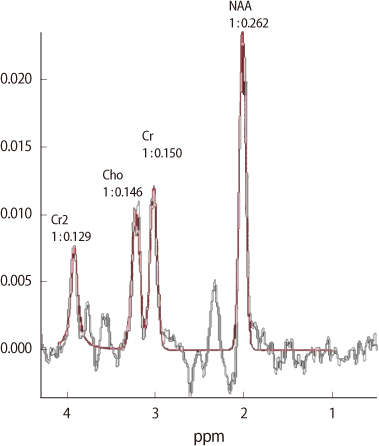
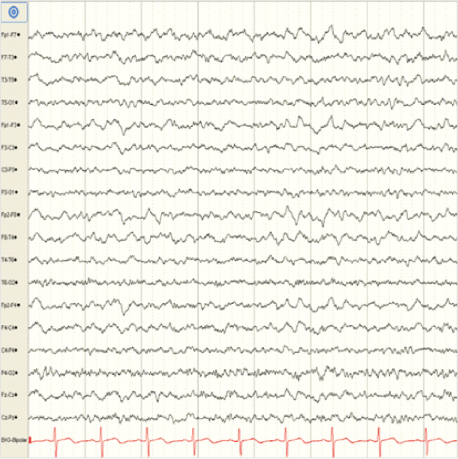
- Creutzfeldt-Jakob disease (CJD) is a degenerative neurological disorder that is incurable and invariably fatal. It is characterized by rapidly progressive dementia presenting with memory loss, personality changes and hallucinations. The symptoms of CJD are caused by progressive death of neurons in the central nervous system, which is associated with build-up of the abnormal prion proteins forming amyloids. In human, CJD can be acquired genetically through a mutation of the gene encoding for the prion protein (PRNP). This occurs in only 5-10% of all CJD cases. We report a 64-year old woman with CJD carrying a V180I mutation that features late onset, rapid progression, no periodic sharp wave complexes on electroencephalography, and cortical signal change and edema in bilateral frontotemporoparietal lobes and basal ganglia on MRI.
MeSH Terms
Figure
Cited by 1 articles
-
Familial Creutzfeldt–Jakob Disease with a PRNP Mutation at Codon 180 Presented with Visual Hallucinations and Illusions
Dong Woo Ryu, Yun Jeong Hong, Jeong Wook Park, Si Baek Lee, Seong Hoon Kim, Yongbang Kim, Min Jae Seong, Byung Seok Kim
Dement Neurocogn Disord. 2019;18(3):105-107. doi: 10.12779/dnd.2019.18.3.105.
Reference
-
1. Rabinovici GD, Wang PN, Levin J, Cook L, Pravdin M, Davis J, et al. First symptom in sporadic Creutzfeldt-Jakob disease. Neurology. 2006. 66:286–287.
Article2. Heinemann U, Krasnianski A, Meissner B, Grasbon-Frodl EM, Kretzschmar HA, Zerr I. Novel PRNP mutation in a patient with a slow progressive dementia syndrome. Med Sci Monit. 2008. 14:CS41–CS43.
Article3. Kong QK, Surewicz WK, Petersen RB, Zhou W, Chen SG, Gambetti P, et al. Prusiner SB, editor. Inherited Prion Diseases. Prion Biology and Disease. 2004. 2nd ed. Cold Spring Harbor: Cold Spring Harbor Laboratory Press;673–776.
Article4. Zerr I, Poser S. Clinical diagnosis and differential diagnosis of CJD and vCJD. With special emphasis on laboratory tests. APMIS. 2002. 110:88–98.5. World Health Organization. WHO Global surveillance, diagnosis and therapy of human transmissible spongiform encephalopathies: Report of a WHO consultation; Emerging and other communicable diseases, surveillance and control. 1998. 02. 9–11.6. Shiga Y, Miyazawa K, Sato S, Fukushima R, Shibuya S, Sato Y, et al. Diffusion-weighted MRI abnormalities as an early diagnostic marker for Creutzfeldt-Jakob disease. Neurology. 2004. 63:443–449.7. Young GS, Geschwind MD, Fischbein NJ, Martindale JL, Henry RG, Liu S, et al. Diffusion-weighted and fluid-attenuated inversion recovery imaging in Creutzfeldt-Jakob disease: high sensitivity and specificity for diagnosis. AJNR Am J Neuroradiol. 2005. 26:1551–1562.
Article8. Yamada M. Prion diseases in Japan: analysis of 918 patients. Rinsho Shinkeigaku. 2007. 47:805–808.
Article9. Chasseigneaux S, Haik S, Laffont-Proust I, De Marco O, Lenne M, Brandel JP, et al. V180I mutation of the prion protein gene associated with atypical PrPSc glycosylation. Neurosci Lett. 2006. 408:165–169.
Article10. Nixon R, Camicioli R, Jamison K, Cervenakova L, Mastrianni JA. The PRNP-V180I mutation is associated with abnormally glycosylated PrP-CJD and Intracellular PrP accumulations. Presented at XIVth International Congress of Neuropathology Scientific Programme. Brain Pathology. 2000. 10:670.
Article11. Jin K, Shiga Y, Shibuya S, Chida K, Sato Y, Konno H, et al. Clinical features of Creutzfeldt-Jakob disease with V180I mutation. Neurology. 2004. 62:502–505.
Article12. Yang TI, Jung DS, Ahn BY, Jeong BH, Cho HJ, Kim YS, et al. Familial Creutzfeldt-Jacob Disease with V180I Mutation. J Korean Med Sci. 2010. 25:1097–1100.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Familial Creutzfeldt-Jakob Disease with V180I Mutation Presented with Broca's Aphasia
- Mad Cow Disease and New Variant Creutzfeldt Jacob Disease
- A Case of Creutzfeldt-Jacob Disease
- Familial Creutzfeldt-Jakob Disease with V180I Mutation
- Patient with Creutzfeldt-Jakob Disease Who Presented Peripheral Type Facial Palsy