Ewha Med J.
2016 Apr;39(2):51-55. 10.12771/emj.2016.39.2.51.
Diffuse Large B-Cell Lymphoma Transformed from a Rectal Mucosa-Associated Lymphoid Tissue Lymphoma
- Affiliations
-
- 1Department of Internal Medicine, Hanil Hospital, Seoul, Korea.
- 2Department of Pathology, Hanil Hospital, Seoul, Korea.
- 3Medical Oncology and Hematology, Department of Internal Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea. parkkoh@daum.net
- KMID: 2171365
- DOI: http://doi.org/10.12771/emj.2016.39.2.51
Abstract
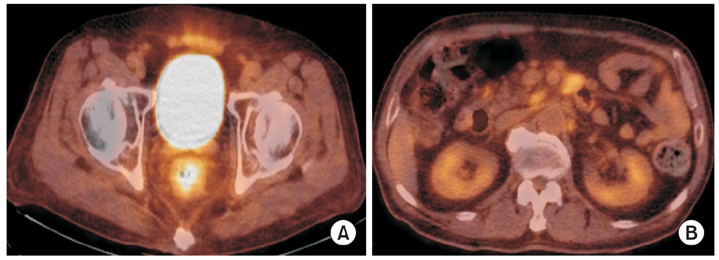
- Primary rectal lymphoma is a rare disease among the gastrointestinal (GI) lymphoma. In particular, diffuse large B-cell lymphoma (DLBCL) transformed from mucosa-associated lymphoid tissue (MALT) lymphoma is often the primary type of GI lymphoma, mostly in stomach or duodenum, but has never been reported in rectum. Here we report an unusual case in which a 75-year-old male patient diagnosed with DLBCL transformed from MALT lymphoma in the rectum. The patient was diagnosed as rectal DLBCL transformed from MALT lymphoma as Lugano stage II2 and was treated with chemotherapy (R-CHOP) with CD-20 monoclonal antibody (rituxaimb). Complete remission of multiple lymphadenopathy and mass forming ulcer of the rectum was achieved after 6 cycles of R-CHOP. He has been free from disease for 12 months.
Keyword
MeSH Terms
Figure
Reference
-
1. Herrmann R, Panahon AM, Barcos MP, Walsh D, Stutzman L. Gastrointestinal involvement in non-Hodgkin's lymphoma. Cancer. 1980; 46:215–222.2. Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972; 29:252–260.3. Koch P, del Valle F, Berdel WE, Willich NA, Reers B, Hiddemann W, et al. Primary gastrointestinal non-Hodgkin's lymphoma: I. Anatomic and histologic distribution, clinical features, and survival data of 371 patients registered in the German Multicenter Study GIT NHL 01/92. J Clin Oncol. 2001; 19:3861–3873.4. Nakamura S, Matsumoto T, Iida M, Yao T, Tsuneyoshi M. Primary gastrointestinal lymphoma in Japan: a clinicopathologic analysis of 455 patients with special reference to its time trends. Cancer. 2003; 97:2462–2473.5. Zucca E, Conconi A, Pedrinis E, Cortelazzo S, Motta T, Gospodarowicz MK, et al. Nongastric marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue. Blood. 2003; 101:2489–2495.6. Montoto S, Fitzgibbon J. Transformation of indolent B-cell lymphomas. J Clin Oncol. 2011; 29:1827–1834.7. Lee SH, Jang BI, Kim TN. A case of primary rectal diffuse large B cell lymphoma presented as multiple polypoid lesions. Korean J Gastrointest Endosc. 2008; 36:302–306.8. Tokunou K, Yamamoto T, Toshimitsu H, Kitamura Y, Ando S. A case of mucosa-associated lymphoid tissue lymphoma of the rectum. Gan To Kagaku Ryoho. 2013; 40:2056–2058.9. Rohatiner A, d'Amore F, Coiffier B, Crowther D, Gospodarowicz M, Isaacson P, et al. Report on a workshop convened to discuss the pathological and staging classifications of gastrointestinal tract lymphoma. Ann Oncol. 1994; 5:397–400.10. Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg. 1961; 49:80–89.11. Kim SJ, Lee GH, Park SH, Shin HD, Jo CL, Kim TH, et al. A case of diffuse large b cell lymphoma transformed from a duodenal low grade malt lymphoma. Korean J Gastrointest Endosc. 2007; 34:103–107.12. Kim JH, Kang DW, Park MJ, Kim JM. High-grade transformation of primary nodal marginal zone B-cell lymphoma: a case report. Korean J Pathol. 2003; 37:282–286.13. Theriault C, Galoin S, Valmary S, Selves J, Lamant L, Roda D, et al. PCR analysis of immunoglobulin heavy chain (IgH) and TcR-gamma chain gene rearrangements in the diagnosis of lymphoproliferative disorders: results of a study of 525 cases. Mod Pathol. 2000; 13:1269–1279.14. Al-Tourah AJ, Gill KK, Chhanabhai M, Hoskins PJ, Klasa RJ, Savage KJ, et al. Population-based analysis of incidence and outcome of transformed non-Hodgkin's lymphoma. J Clin Oncol. 2008; 26:5165–5169.15. Wang SL, Liao ZX, Liu XF, Yu ZH, Gu DZ, Qian TN, et al. Primary early-stage intestinal and colonic non-Hodgkin's lymphoma: clinical features, management, and outcome of 37 patients. World J Gastroenterol. 2005; 11:5905–5909.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Diffuse Large B Cell Lymphoma Transformed from a Duodenal Low Grade MALT Lymphoma
- Gastrointestinal Lymphoma
- Gastrointestinal Lymphoma
- Ileal Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma with a Large-Cell Component That Regressed Spontaneously
- Mucosa-associated Lymphoid Tissue Lymphoma of Parotid Gland