Ewha Med J.
2014 Sep;37(2):136-140. 10.12771/emj.2014.37.2.136.
Pheochromocytoma Presenting with Multiple Cardiovascular Manifestations
- Affiliations
-
- 1Department of Internal Medicine, Sejong General Hospital, Bucheon, Korea.
- 2Division of Cardiology, Department of Internal Medicine, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea. ycw717@naver.com
- KMID: 2171298
- DOI: http://doi.org/10.12771/emj.2014.37.2.136
Abstract
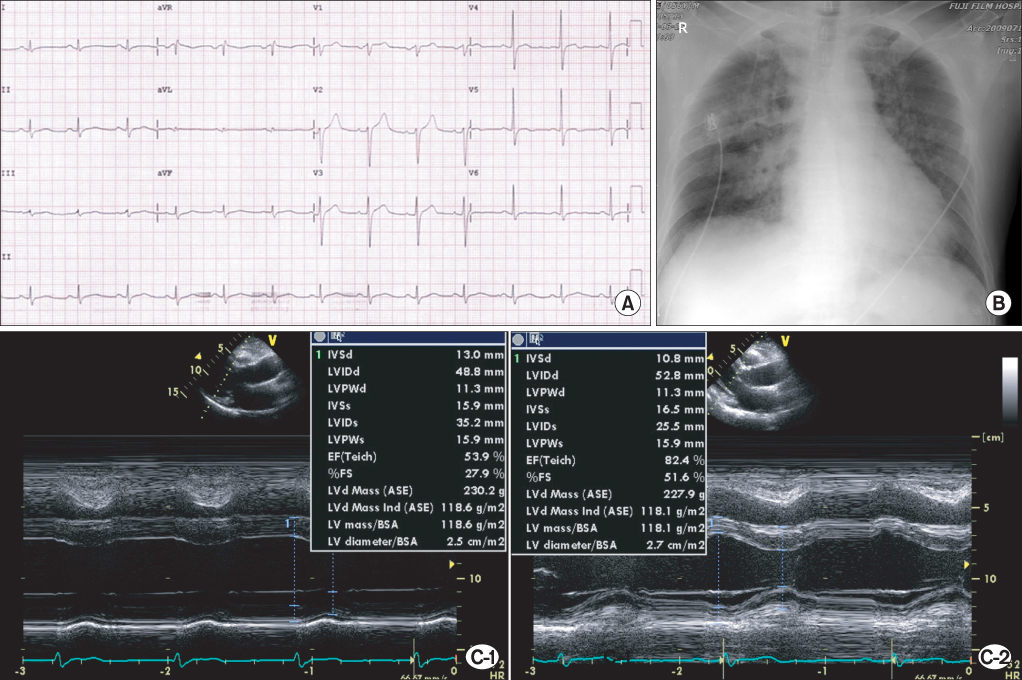
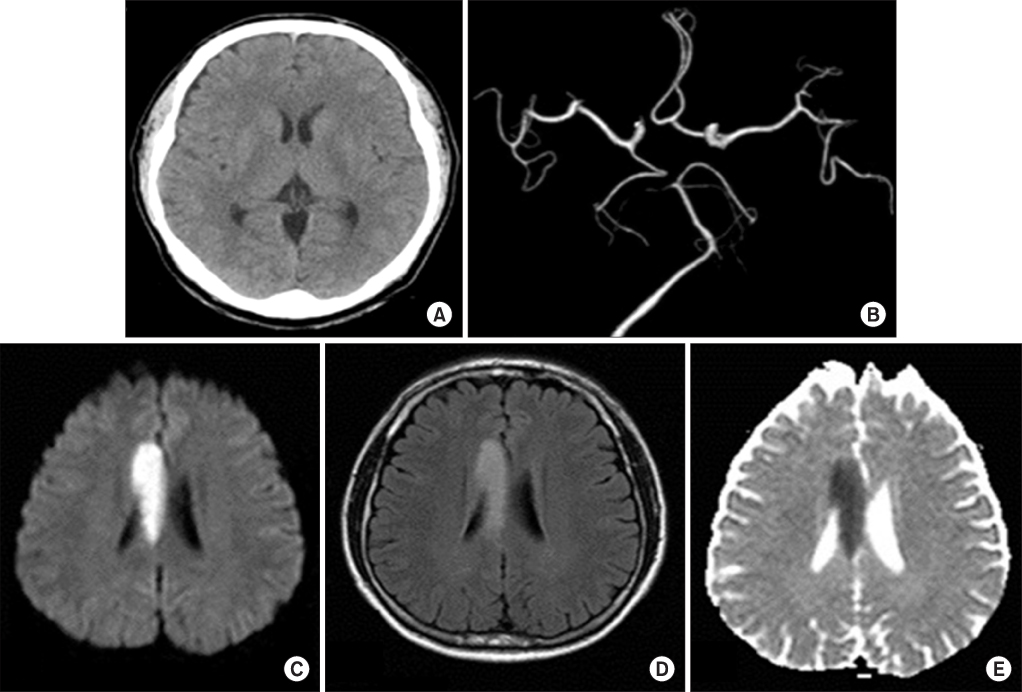
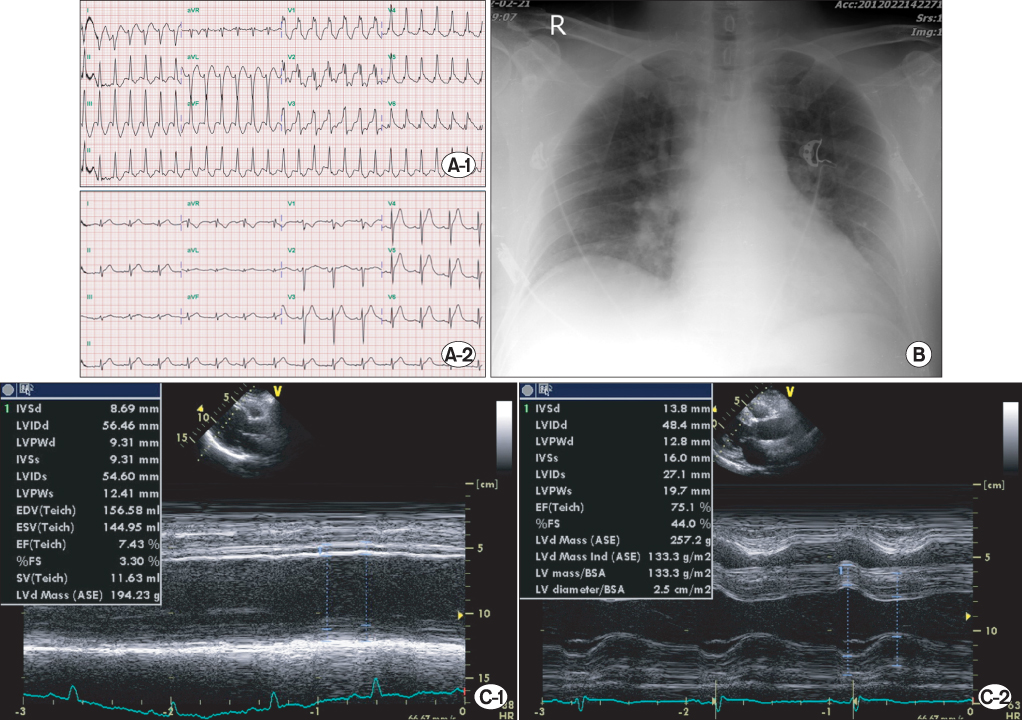
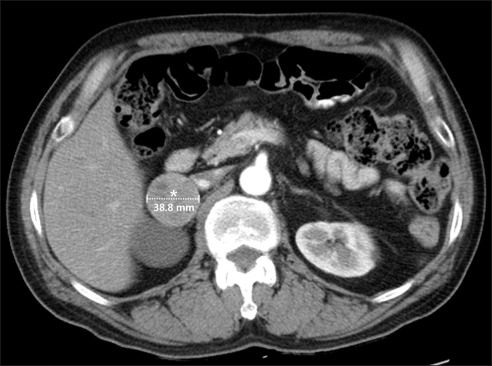
- A 56-year-old man presented with sudden onset of congestive heart failure (New York Heart Association class III to IV) after mild stress and developed various cardiovascular manifestations. At first visit, cardiac enzyme elevation, regional left ventricular (LV) wall motion abnormality and pulmonary edema were evident. However, coronary angiography was normal. LV function was totally recovered at discharge, suspicious of fulminant myocarditis. During the hospital stay, acute non-obstructive stroke without neurologic sequelae occurred. After 3 years, he re-admitted because ventricular tachycardia and severe LV systolic dysfunction (ejection fraction, 15%) were developed. After 3 days of applying percutaneous cardiopulmonary bypass system, the patient was completely recovered. Suspicious of pheochromocytoma, we checked 24-hour urine catecholamines and metanephrines and abdomen computed tomography, which revealed pheochromocytoma. The patient underwent laparoscopic adrenalectomy.
MeSH Terms
Figure
Reference
-
1. Abraham J, Mudd JO, Kapur NK, Klein K, Champion HC, Wittstein IS. Stress cardiomyopathy after intravenous administration of catecholamines and beta-receptor agonists. J Am Coll Cardiol. 2009; 53:1320–1325.2. Wittstein IS. Stress cardiomyopathy: a syndrome of Catecholamine-mediated myocardial stunning? Cell Mol Neurobiol. 2012; 32:847–857.3. Dagartzikas MI, Sprague K, Carter G, Tobias JD. Cerebrovascular event, dilated cardiomyopathy, and pheochromocytoma. Pediatr Emerg Care. 2002; 18:33–35.4. Hill JB, Schwartzman RJ. Cerebral infarction and disseminated intravascular coagulation with pheochromocytoma. Arch Neurol. 1981; 38:395.5. Oh HC, Koh JM, Kim MS, Park JY, Shong YK, Lee KU, et al. A case of ACTH-producing pheochromocytoma associated with pregnancy. Endocr J. 2003; 50:739–744.6. Van YH, Wang HS, Lai CH, Lin JN, Lo FS. Pheochromocytoma presenting as stroke in two Taiwanese children. J Pediatr Endocrinol Metab. 2002; 15:1563–1567.7. Park JW, Park SJ, Hur KY, Kim JH, Choi YL, Park SM, et al. Recurrent ventricular tachycardia in malignant metastatic pheochromocytoma. Circulation. 2012; 125:e435–e438.8. Huang YC, Chang CH, Wang CH, Chang JS. Pheochromocytoma complicated with severe ventricular tachycardia: report of one case. Acta Paediatr Taiwan. 2007; 48:280–284.9. Traykov VB, Kotirkov KI, Petrov IS. Pheochromocytoma presenting with bidirectional ventricular tachycardia. Heart. 2013; 99:509.10. Gregori M, Paneni F, D'Agostino M, Tocci G, Ferrucci A, Savoia C. High blood pressure, ventricular tachycardia and transient left ventricular dysfunction: do not forget pheochromocytoma. High Blood Press Cardiovasc Prev. 2011; 18:57–59.11. Zelinka T, Petrak O, Turkova H, Holaj R, Strauch B, Krsek M, et al. High incidence of cardiovascular complications in pheochromocytoma. Horm Metab Res. 2012; 44:379–384.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Nonfunctioning Cystic Pheochromocytoma
- A Case of Pheochromocytoma Misdiagnosed as Activation of Behcet's Disease
- A Case of Malignant Pheochromocytoma
- Multiple Ruptured Cerebral Aneurysms as a Presenting Feature of Pheochromocytoma in a Patient with Neurofibromatosis 1
- A Case of Calcitonin Secreting Pheochromocytoma