Anesth Pain Med.
2016 Jan;11(1):14-22. 10.17085/apm.2016.11.1.14.
Epidural neuroplasty/epidural adhesiolysis
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Korea University Guro Hospital, Seoul, Korea. clonidine@empal.com
- KMID: 2169063
- DOI: http://doi.org/10.17085/apm.2016.11.1.14
Abstract
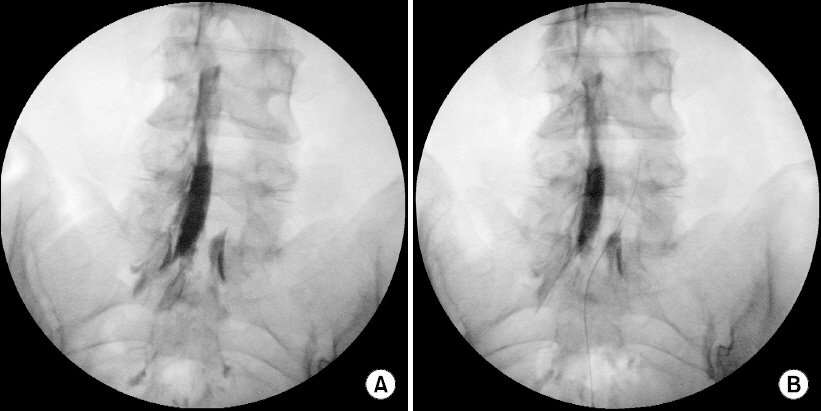
- Epidural neuroplasty is a treatment modality for back pain and/or radiating pain caused by mechanical compression or neural inflammation of intra-spinal neural structures. Since epidural neuroplasty was first introduced as a treatment for pain caused by epidural adhesion such as failed back surgery syndrome (FBSS), it has been performed as a treatment for many kinds of pain of spinal origin including acute/chronic herniation of intervertebral disc, radiculopathy, spinal stenosis, FBSS, epidural adhesion, vertebral compression fracture, vertebral metastasis, resistant multilevel degenerative arthritis, epidural scar pain by infection or meningitis, and whiplash injury. Epidural neuroplasty is a catheterization technique used to treat back pain and/or radiating pain by injecting therapeutic drugs into lesions of epidural space shown as a filling defect in epidurogram. Usually, normal saline, local anesthetics, and steroid are used as therapeutic drugs. The exact mechanisms of action of the procedure are unknown but include 2 postulated mechanisms of action for pain relief. i.e., mechanical adhesiolysis by volume effect and chemical adhesiolysis by injected drugs. Relative large volumes of normal saline injection resolve adhesions and wash out accumulated pain substances; local anesthetics are used for stabilization and analgesia of flaring neural structures and for pain management for procedure related pain; and steroid is used for the treatment of inflammation of neural and peri-neural structures. The resolution of filling defect can be verified by post-procedure epidurogram. The key point of epidural neuroplasty for good results, is the exact localization of the epidural catheter into the epidural lesion.
Keyword
MeSH Terms
-
Analgesia
Anesthetics, Local
Back Pain
Catheterization
Catheters
Cicatrix
Epidural Space
Failed Back Surgery Syndrome
Fractures, Compression
Inflammation
Intervertebral Disc
Intervertebral Disc Displacement
Meningitis
Neoplasm Metastasis
Osteoarthritis
Pain Management
Radiculopathy
Spinal Stenosis
Whiplash Injuries
Anesthetics, Local
Figure
Cited by 1 articles
-
Percutaneous epidural balloon neuroplasty: a narrative review of current evidence
Doo-Hwan Kim, Jin-Woo Shin, Seong-Soo Choi
Anesth Pain Med. 2022;17(4):361-370. doi: 10.17085/apm.22237.
Reference
-
1. Racz GB, Heavner JE, Diede JH. Waldman SD, Winnie AP, editors. Lysis of epidural adhesions utilizing the epidural approach. Interventional Pain Management. 1996. Philadelphia: W.B. Saunders;p. 339–51.2. Racz GB, Holubec JT. Racz GB, editor. Lysis of adhesions in the epidural space. Techniques of Neurolysis. 1989. Boston: Kluwer Academic;p. 57–72. DOI: 10.1007/978-1-4899-6721-3_6.
Article3. Lee SC, Oh WS, Kim JK, Roh CJ, Son JC. Epidural adhesiolysis in low back pain. Korean J Pain. 1997; 10:214–9.4. Waldman SD, Winnie AP. Interventional Pain Management. 1996. Philadelphia: WB Saunders Co;p. 144–5.5. Devulder J, Bogaert L, Castille F, Moerman A, Rolly G. Relevance of epidurography and epidural adhesiolysis in chronic failed back surgery patients. Clin J Pain. 1995; 11:147–50. DOI: 10.1097/00002508-199506000-00011. PMID: 7549172.
Article6. Lee SI, Kim KT, Hwang JK. Endoscopic and non-endoscopic epidural adhesiolysis in FBSS patient. Korean J Anestheisol. 2004; 46:329–35.
Article7. LaRocca H, Macnab I. The laminectomy membrane: Studies in its evolution, characteristics, effects and prophylaxis in dogs. J Bone Joint Surg Br. 1974; 56B:545–50. PMID: 4421702.8. Burton CV. Lumbosacral arachnoiditis. Spine (Phila Pa 1976). 1978; 3:24–30. DOI: 10.1097/00007632-197803000-00006.
Article9. McCarron RF, Wimpee MW, Hudkins PG, Laros GS. The inflammatory effect of nucleus pulposus. A possible element in the pathogenesis of low-back pain. Spine (Phila Pa 1976). 1987; 12:760–4. DOI: 10.1097/00007632-198710000-00009.10. Benner B, Ehni G. Spinal arachnoiditis. The postoperative variety in particular. Spine (Phila Pa 1976). 1978; 3:40–4. DOI: 10.1097/00007632-197803000-00009.11. Fan YF, Chong VF, Tan SK. Failed back surgery syndrome: differentiating epidural fibrosis and recurrent disc prolapse with Gd-DTPA enhanced MRI. Singapore Med J. 1995; 36:153–6. PMID: 7676258.12. Saberski LR, Kitahata LM. Review of the clinical basis and protocol for epidural endoscopy. Conn Med. 1996; 60:71–3. PMID: 8820630.13. Song SO, Lim HJ. Clinical experience of epidural adhesiolysis in patients with failed back surgery syndrome. Korean J Anesthesiol. 2004; 47:547–52.
Article14. Cyriax P. Illustrated manual of orthopaedic medicine: the sacroiliac, buttock and hip. 1983. London: Geigy Pharmaceuticals;p. 210.15. Ramsay M, Roberts C. Epidural injection dose cause an increase in CSF pressure. Anesth Analg. 1991; 73:668. DOI: 10.1213/00000539-199111000-00030. PMID: 1952155.16. Chen C, Cavanaugh JM, Ozaktay AC, Kallakuri S, King AI. Effects of phospholipase A2 on lumbar nerve root structure and function. Spine (Phila Pa 1976). 1997; 22:1057–64. DOI: 10.1097/00007632-199705150-00002.
Article17. Choi KH, Lee SH, Kim TS, Kim HS, Kim KM, Kim DS. A study of the effects of neuroplasty by spinal endoscopy in herniated nucleus pulposus patients for therapeutic purpose. Korean J Anesthesiol. 1999; 37:848–53.
Article18. Benzon HT. Epidural steroid injections for low back pain and lumbosacral radiculopathy. Pain. 1986; 24:277–95. DOI: 10.1016/0304-3959(86)90115-6.
Article19. Hollmann MW, Durieux ME. Prolonged actions of short-acting drugs: local anesthetics and chronic pain. Reg Anesth Pain Med. 2000; 25:337–9. DOI: 10.1053/rapm.2000.7606.
Article20. Hitchcock E. Osmolytic neurolysis for intractable facial pain. Lancet. 1969; 1:434–6. DOI: 10.1016/S0140-6736(69)91479-2.
Article21. Lake DA, Barnes CD. Effects of changes in osmolality on spinal cord activity. Exp Neurol. 1980; 68:555–67. DOI: 10.1016/0014-4886(80)90109-0.
Article22. Jewett DL, King JS. Conduction block of monkey dorsal rootlets by water and hypertonic saline solutions. Exp Neurol. 1971; 33:225–37. DOI: 10.1016/0014-4886(71)90116-6.
Article23. Oh WS, Hong KH, Lee SC. Comparative study for analgesic and adverse effects of 8% and 10% hypertonic saline in epidural adhesiolysis. J Korean Pain Soc. 2000; 13:74–8.24. Heavner JE, Racz GB, Raj P. Percutaneous epidural neuroplasty: Prospective evaluation of 0.9% NaCl versus 10% NaCl with or without Hyaluronidase. Reg Anesth Pain Med. 1999; 24:202–7. DOI: 10.1016/S1098-7339(99)90128-1. PMID: 10338168.25. Gerdesmeyer L, Wagenpfeil S, Birkenmaier C, Veihelmann A, Hauschild M, Wagner K, et al. Percutaneous epidural lysis of adhesions in chronic lumbar radicular pain: a randomized, double-blind, placebo-controlled trial. Pain Physician. 2013; 16:185–96. PMID: 23703406.26. Manchikanti L, Rivera JJ, Pampati V, Damron KS, McManus CD, Brandon DE, et al. One day lumbar epidural adhesiolysis and hypertonic saline neurolysis in treatment of chronic low back pain: a randomized, double-blind trial. Pain Physician. 2004; 7:177–86. PMID: 16868590.27. Park EJ, Park SY, Lee SJ, Kim NS, Koh do Y. Clinical outcomes of epidural neuroplasty for cervical disc herniation. J Korean Med Sci. 2013; 28:461–5. DOI: 10.3346/jkms.2013.28.3.461. PMID: 23487574. PMCID: PMC3594612.
Article28. Moon DE, Park HJ, Kim YH. Assessment of clinical outcomes of cervical epidural neuroplasty using a Racz-catheter and predictive factors of efficacy in patients with cervical spinal pain. Pain Physician. 2015; 18:E163–70. PMID: 25794215.29. Park CH, Lee SH, Lee SC. Preliminary results of the clinical effectiveness of percutaneous adhesiolysis using a Racz catheter in the management of chronic pain due to cervical central stenosis. Pain Physician. 2013; 16:353–8. PMID: 23877451.30. Veihelmann A, Devens C, Trouillier H, Birkenmaier C, Gerdesmeyer L, Refior HJ. Epidural neuroplasty versus physiotherapy to relieve pain in patients with sciatica: a prospective randomized blinded clinical trial. J Orthop Sci. 2006; 11:365–9. DOI: 10.1007/s00776-006-1032-y. PMID: 16897200.
Article31. Kim HJ, Rim BC, Lim JW, Park NK, Kang TW, Sohn MK, et al. Efficacy of epidural neuroplasty versus transforaminal epidural steroid injection for the radiating pain caused by a herniated lumbar disc. Ann Rehabil Med. 2013; 37:824–31. DOI: 10.5535/arm.2013.37.6.824. PMID: 24466517. PMCID: PMC3895522.
Article32. Lee JH, Lee SH. Clinical effectiveness of percutaneous adhesiolysis versus transforaminal epidural steroid injection in patients with postlumbar surgery syndrome. Reg Anesth Pain Med. 2014; 39:214–8. DOI: 10.1097/AAP.0000000000000073. PMID: 24646624.
Article33. Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. A comparative effectiveness evaluation of percutaneous adhesiolysis and epidural steroid injections in managing lumbar post surgery syndrome: a randomized, equivalence controlled trial. Pain Physician. 2009; 12:E355–68. PMID: 19935992.34. Manchikanti L, Cash KA, McManus CD, Pampati V, Singh V, Benyamin R. The preliminary results of a comparative effectiveness evaluation of adhesiolysis and caudal epidural injections in managing chronic low back pain secondary to spinal stenosis: a randomized, equivalence controlled trial. Pain Physician. 2009; 12:E341–54. PMID: 19935991.35. Manchikanti L, Pakanati RR, Bakhit CE, Pampafi V. Role of adhesiolysis and hypertonic saline neurolysis in management of low back pain: evaluation of modification of the Racz protocol. Pain Digest. 1999; 9:91–6.36. Helm Ii S, Benyamin RM, Chopra P, Deer TR, Justiz R. Percutaneous adhesiolysis in the management of chronic low back pain in post lumbar surgery syndrome and spinal stenosis: a systematic review. Pain Physician. 2012; 15:E435–62. PMID: 22828693.37. Hayek SM, Helm S, Benyamin RM, Singh V, Bryce DA, Smith HS. Effectiveness of spinal endoscopic adhesiolysis in post lumbar surgery syndrome: a systematic review. Pain Physician. 2009; 12:419–35. PMID: 19305488.38. Trescot AM, Chopra P, Abdi S, Datta S, Schultz DM. Systematic review of effectiveness and complications of adhesiolysis in the management of chronic spinal pain: an update. Pain Physician. 2007; 10:129–46. PMID: 17256027.39. Chopra P, Smith HS, Deer TR, Bowman RC. Role of adhesiolysis in the management of chronic spinal pain: a systemic review of effectiveness and complications. Pain Physician. 2005; 8:87–100. PMID: 16850047.40. Racz GB, Heavner JE, Trescot A. Percutaneous lysis of epidural adhesions--evidence for safety and efficacy. Pain Pract. 2008; 8:277–86. DOI: 10.1111/j.1533-2500.2008.00203.x. PMID: 18503627.
Article41. Epter RS, Helm S 2nd, Hayek SM, Benyamin RM, Smith HS, Abdi S. Systematic review of percutaneous adhesiolysis and management of chronic low back pain in post lumbar surgery syndrome. Pain Physician. 2009; 12:361–78. PMID: 19305485.42. Oh WS, Lee SJ, Hong KH. Fulminant headache after epiduroscopy. Korean J Pain. 2000; 13:130–3.43. Royakkers AA, Willigers H, van der Ven AJ, Wilmink J, Durieux M, van Kleef M. Catheter-related epidural abscess -- don’t wait for neurological deficits. Acta Anaesthesiol Scand. 2002; 46:611–5. DOI: 10.1034/j.1399-6576.2002.460523.x. PMID: 12027860.44. Soehle M, Sallenfang T. Spinal epidural abscesses, clinical manifestations, prognostic factors and outcomes. Neurosurgery. 2002; 51:79–85. DOI: 10.1097/00006123-200207000-00013. PMID: 12182438.
Article45. Barsa J, Bartra M, Fink BR, Sumi SM. A comparative in vivo study of local neurotoxicity of lidocaine, bupibacaine, 2-chloroprocaine and a mixture of 2-chloroprocaine and bupivacaine. Anesth Analg. 1982; 61:961–7. DOI: 10.1213/00000539-198212000-00001. PMID: 7149299.46. Bainton CR, Strichartz GR. Concentration dependence of lidocaine-induced irreversible conduction loss in frog nerve. Anesthesiology. 1994; 81:657–67. DOI: 10.1097/00000542-199409000-00020.
Article47. Hampl KF, Schneider MC, Ummenhofer W, Drewe J. Transient neurologic symptoms after spinal anesthesia. Anesth Analg. 1995; 81:1148–53. DOI: 10.1213/00000539-199512000-00006. PMID: 7486096.
Article48. Song YK, Kim YD, Kim JH. Acute allergic reaction caused by hyaluronidase used in the pain management: a case report and literature review: a case report. Anesth Pain Med. 2014; 9:174–8.49. Manchikanti L, Pampati V, Fellows B, Rivera JJ, Damron KS, Beyer C, et al. Effectiveness of percutaneous adhesiolysis with hypertonic saline neurolysis in refractory spinal stenosis. Pain Physician. 2001; 4:366–73. PMID: 16902683.50. Manchikanti L, Bakhit CE. Percutaneous lysis of epidural adhesions. Pain Physician. 2000; 3:46–64. PMID: 16906207.
Article51. Manchikanti L, Staats PS, Singh V, Schultz DM, Vilims BD, Jasper JF, et al. Evidence-based practice guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2003; 6:3–81. PMID: 16878163.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebellar Infarction Following Epidural Abscess after Epidural Neuroplasty
- Percutaneous Epidural Neuroplasty
- Percutaneous Epidural Neuroplasty
- The Sensory Change on the S2 Area after Epidural Adhesiolysis: A case report
- Massive Epidural Hematoma Caused by Percutaneous Epidural Neuroplasty: A Case Report