J Korean Orthop Assoc.
2015 Jun;50(3):215-224. 10.4055/jkoa.2015.50.3.215.
Percutaneous Epidural Neuroplasty
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul Sacred Heart General Hospital, Seoul, Korea. msh124@paran.com
- 2Woorichuck Hospital Spine Center, Cheonan, Korea.
- KMID: 1851955
- DOI: http://doi.org/10.4055/jkoa.2015.50.3.215
Abstract
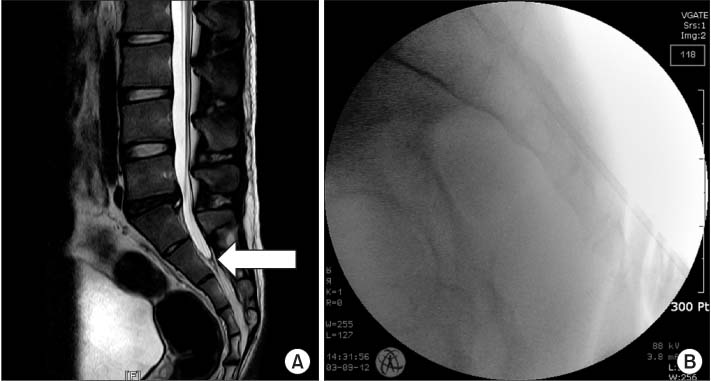
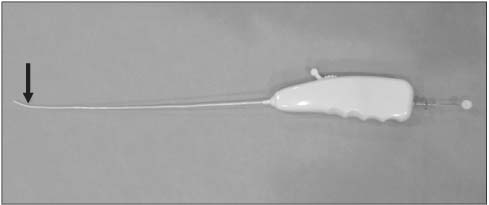
- Interventional pain management by percutaneous epidural neuroplasty (PEN) has potential as a useful treatment method in chronic low back and/or radicular pain that is refractory to other conservative treatments. The effect of PEN is known to result from targeting of drug delivery to areas of pathology in the spinal epidural space. The procedure involves removing barriers, such as epidural fibrosis, that prevent drug from reaching target sites. Therefore, the goal during lysis of epidural adhesions is to penetrate mechanical barriers impeding injected material from spreading effectively into the areas of pathology in the epidural space by the catheter. An additional lavage effect, reducing the local concentration of proinflammatory substances seems possible. Although a true mechanical lysis of postsurgical adhesions or scar tissues by means of PEN appears to be impossible because it has been proven by experimental biomechanical study, mild to moderate adhesions may be broken up by a PEN catheter allowing the medications to reach the target site through the new channel made by the catheter. This review will focus on the adhesiolysis technique using the sacral hiatus approach in treatment of chronic low back pain with/without lumbosacral radiculopathy.
MeSH Terms
Figure
Reference
-
1. Manchikanti L, Helm Ii S, Pampati V, Racz GB. Percutaneous adhesiolysis procedures in the medicare population: analysis of utilization and growth patterns from 2000 to 2011. Pain Physician. 2014; 17:E129–E139.2. Chan CW, Peng P. Failed back surgery syndrome. Pain Med. 2011; 12:577–606.
Article3. Hsu E, Atanelov L, Plunkett AR, Chai N, Chen Y, Cohen SP. Epidural lysis of adhesions for failed back surgery and spinal stenosis: factors associated with treatment outcome. Anesth Analg. 2014; 118:215–224.4. Veihelmann A, Devens C, Trouillier H, Birkenmaier C, Gerdesmeyer L, Refior HJ. Epidural neuroplasty versus physiotherapy to relieve pain in patients with sciatica: a prospective randomized blinded clinical trial. J Orthop Sci. 2006; 11:365–369.
Article5. Veihelmann A. The significance of immunology in orthopaedics today. Orthopade. 2003; 32:736–743.6. Specchia N, Pagnotta A, Toesca A, Greco F. Cytokines and growth factors in the protruded intervertebral disc of the lumbar spine. Eur Spine J. 2002; 11:145–151.
Article7. Ozaktay AC, Cavanaugh JM, Asik I, DeLeo JA, Weinstein JN. Dorsal root sensitivity to interleukin-1 beta, interleukin-6 and tumor necrosis factor in rats. Eur Spine J. 2002; 11:467–475.8. Heavner JE, Racz GB, Raj P. Percutaneous epidural neuroplasty: prospective evaluation of 0.9% NaCl versus 10% NaCl with or without hyaluronidase. Reg Anesth Pain Med. 1999; 24:202–207.9. Abdi S, Datta S, Trescot AM, et al. Epidural steroids in the management of chronic spinal pain: a systematic review. Pain Physician. 2007; 10:185–212.10. Devulder J, Bogaert L, Castille F, Moerman A, Rolly G. Relevance of epidurography and epidural adhesiolysis in chronic failed back surgery patients. Clin J Pain. 1995; 11:147–150.
Article11. Lee JH, Lee SH. Clinical effectiveness of percutaneous adhesiolysis using Navicath for the management of chronic pain due to lumbosacral disc herniation. Pain Physician. 2012; 15:213–221.12. Birkenmaier C, Baumert S, Schroeder C, Jansson V, Wegener B. A biomechanical evaluation of the epidural neurolysis procedure. Pain Physician. 2012; 15:E89–E97.13. Manchikanti L, Bakhit CE. Percutaneous lysis of epidural adhesions. Pain Physician. 2000; 3:46–64.
Article14. Kim JH, Jung HJ, Nahm FS, Lee PB. Does improvement in epidurography following percutaneous epidural neuroplasty correspond to patient outcome? Pain pract. Published online April 21, 2014. DOI: 10.1111/papr.12197.
Article15. Rydell N, Balazs EA. Effect of intra-articular injection of hyaluronic acid on the clinical symptoms of osteoarthritis and on granulation tissue formation. Clin Orthop Relat Res. 1971; 80:25–32.
Article16. Helm S. A review of the role of epidural percutaneous adhesiolysis. Pain Manag. 2012; 2:609–616.
Article17. Helm Ii S, Benyamin RM, Chopra P, Deer TR, Justiz R. Percutaneous adhesiolysis in the management of chronic low back pain in post lumbar surgery syndrome and spinal stenosis: a systematic review. Pain Physician. 2012; 15:E435–E462.18. Kim SB, Kim MK, Kim KD, Lim YJ. Unintended complication of intracranial subdural hematoma after percutaneous epidural neuroplasty. J Korean Neurosurg Soc. 2014; 55:170–172.
Article19. Sekiguchi M, Yabuki S, Satoh K, Kikuchi S. An anatomic study of the sacral hiatus: a basis for successful caudal epidural block. Clin J Pain. 2004; 20:51–54.
Article20. Jo DH, Yang HJ, Kim JJ. Approach for epiduroscopic laser neural decompression in case of the sacral canal stenosis. Korean J Pain. 2013; 26:392–395.
Article21. Gerdesmeyer L, Wagenpfeil S, Birkenmaier C, et al. Percutaneous epidural lysis of adhesions in chronic lumbar radicular pain: a randomized, double-blind, placebo-controlled trial. Pain Physician. 2013; 16:185–196.22. Manchikanti L, Rivera JJ, Pampati V, et al. One day lumbar epidural adhesiolysis and hypertonic saline neurolysis in treatment of chronic low back pain: a randomized, double-blind trial. Pain Physician. 2004; 7:177–186.23. Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. A comparative effectiveness evaluation of percutaneous adhesiolysis and epidural steroid injections in managing lumbar post surgery syndrome: a randomized, equivalence controlled trial. Pain Physician. 2009; 12:E355–E368.24. Manchikanti L, Cash KA, McManus CD, Pampati V, Singh V, Benyamin R. The preliminary results of a comparative effectiveness evaluation of adhesiolysis and caudal epidural injections in managing chronic low back pain secondary to spinal stenosis: a randomized, equivalence controlled trial. Pain Physician. 2009; 12:E341–E354.25. Jamison DE, Hsu E, Cohen SP. Epidural adhesiolysis: an evidence-based review. J Neurosurg Sci. 2014; 58:65–76.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebellar Infarction Following Epidural Abscess after Epidural Neuroplasty
- Unintended Complication of Intracranial Subdural Hematoma after Percutaneous Epidural Neuroplasty
- Percutaneous Epidural Neuroplasty
- Massive Epidural Hematoma Caused by Percutaneous Epidural Neuroplasty: A Case Report
- Ultrasound-guided removal of epidural catheter breakage after percutaneous epidural neuroplasty: A case report